60 Copyright 2012 The Korean Society of Neuro-Ophthalmology http://neuro-ophthalmology.co.kr
Acute Demyelinating Disease in the Brainstem: Initial Manifestation of Neuromyelitis Optica Spectrum Disorder Associated with Sjögren Syndrome
Su Sin Park, MD, Hak Seung Lee, MD, Hyuk Chang, MD
Department of Neurology, Wonkwang University School of Medicine, Institute of Wonkwang Medical Science, Iksan, Korea
Optic neuritis or longitudinally extensive myelitis in Sjögren syndrome suggests a neuromyelitis optica spectrum disorder (NMOSD), which includes recurrent isolated optic neuritis, and optic neuritis or myelitis in the context of certain organ-specific and non-organ- specific autoimmune disease. We report a patient with sudden vertigo and dysequilibrium who showed acute demyelinating le- sion in the pontomesencephalic area associated with positive antinuclear antibody, Sjögren syndrome A (SSA) antibody and NMO- IgG.
Keywords: Neuromyelitis optica spectrum disorder; Sjögren syndrome
INTRODUCTION
Sjögren’s syndrome (SS) is an autoimmune disorder that is character- ized by lymphocytic infiltration of exocrine glands resulting in sicca syn- dromes. SS has also been associated with various extraglandular mani- festations including neurologic dysfunction ranging from paresthesias to central nervous system lesions.1 Central nervous system (CNS) in- volvement has been variably reported in 0-68% of the SS patients.2 With the recent discovery of an antibody to aquaporin-4 (NMO-IgG), which is considered to be specific for neuromyelitis optica (NMO),3 an overlap between patients with primary SS and neuromyelitis optica spectrum diseases (NMOSD) is being noted. In addition, patients with NMO have asymptomatic and symptomatic brain MRI lesions, of which several le- sions have been suggested as characteristic findings of brain abnormali- ties in patients with NMO and NMO-IgG.4 We report a patient with sudden vertigo and dysequilibrium who showed acute demyelinating le- sion in the pontomesencephalic area associated with positive antinuclear antibody, Sjögren syndrome A (SSA) antibody and NMO-IgG.
CASE REPORT
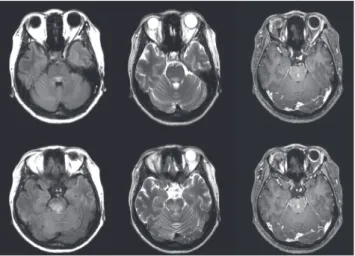
A previously healthy 40-year-old woman noticed with acute onset of vertigo and disequilibrium. Within 5 days, she noted whirling vertigo, oscillopsia and falling and became unable to walk without support. Her past medical and family histories were unremarkable. Initial neurologi- cal examination showed spontaneous upbeating nystagmus, bilateral gaze evoked nystagmus (GEN) and bilateral truncal ataxia. Other physi- cal examination and routine blood test results were unremarkable. Three days after admission, she developed sudden diplopia and bilateral op- thalmoplegia was observed. Brain MRI showed irregular marginated mild brain swelling lesion in midbrain and pons with suspicious mild enhancement suggesting acute demyelinating disease (Fig. 1). The eryth- rocyte sedimentation rate was 12 mm/h. There was no evidence of a hy- percoagulation. Tests for antiphospholipid antibodies and lupus antico- agulant were negative. She had normal or negative studies for serum an- giotensin converting enzyme, and syphilis serology, p and c ANCA, rheumatoid factor, and chest X-ray. There was a positive result of anti- SSA antibody (1:500) and antinuclear antibody. In addition, low titer of
Correspondence to: Hak Seung Lee, MD
Department of Neurology, Wonkwang University School of Medicine, 344-2 Shinyong-dong, Iksan 570-711, Korea Tel: +82-63-859-1410; Fax: +82-63-842-7379; E-mail: nmgom@wonkwang.ac.kr
Received: Jun. 6, 2012 / Accepted: Jun. 6, 2012
CASE REPORT
ISSN: 2234-0971 대한안신경의학회지: 제2권 제1호
Clin Neuroophthalmol 2(1):60-61, June 2012
Park SS, et al. • Acute Demyelinating Disease in the Brainstem: Neuromyelitis Optica Spectrum Disorder(NMOSD) with Sjogren Syndrome
Clin Neuroophthalmol 2(1):60-61, June 2012 http://neuro-ophthalmology.co.kr 61
NMO-IgG was detected in the patient’s serum. Cerebrospinal fluid was normal with negative oligoclonal bands.
She was treated with high-dose intravenous methylprednisolone (500 mg/day for 5 days) followed by daily steroid supplementation. After ste- roid pulse therapy, however, there was no improvement of clinical symp- toms such as disequilibrium and bilateral ophthalmoplegia. Eighteen days after admission, she was transferred to other urban university hos- pital.
DISCUSSION
This case demonstrates that SS with CNS involvement shows charac- teristic findings of NMO, both radiologically and serologically. Although the frequency of CNS manifestations in SS patients is variable, it is usual- ly seen in 6-20% of patients.5 CNS symptoms include seizures, cognitive dysfunctions, aseptic meningoencephalitis, acute or chronic progressive myelopathy, spinal subarachnoid hemorrhage, and optic neuropathy.6 Acute demyelinating disease in brainstem has rarely been reported in SS patients.
NMO patients show concomitant autoantibodies, variably from 38 to 75%, of which anti-Ro/SS antibody (SSA-Ab) is frequently detectable in NMO-IgG seropositive patients.7 In addition, recurrent myelitis and NMO show positivity for SSA-Ab, more frequently (77%) than in mono- phasic disease (33%).8 Radiologically, high proportions of sero-positive patients had large lesions, cavity formation, and lesions meeting Barkhof
MRI criteria, as well. Thus, these serologic and MRI findings of NMO- Ab positive patients suggest that NMO-Ab is related to vigorous disease activity and more intense autoimmunity, causing extensive, destructive, and disseminated CNS lesions.
Generally, two possible mechanisms explain the CNS structural dam- age in SS; one is demyelination and the other is vasculitis.9 Patients with other autoimmune diseases, including neuro-Behcet’s disease or system- ic lupus erythematosus, show brain MRI findings of acute infarction or vasogenic edema, although distinctive mechanisms causing different MRI findings in SS have not been elucidated.10 This case demonstrates that SS with CNS involvement shows more frequent characteristic find- ings of NMO, both radiologically and serologically compared with a pre- vious study.7 In conclusion, This case suggests that the coexistence of NMOSD should be explored in SS patients with recurrent CNS manifes- tations, particularly if they have brain abnormalities characteristic of NMO.
REFERENCES
1. Ozgocmen S, Gur A. Treatment of central nervous system involvement associated with primary Sjögren’s syndrome. Curr Pharm Des 2008;
14:1270-1273.
2. Delalande S, de Seze J, Fauchais AL, Hachulla E, Stojkovic T, Ferriby D, et al. Neurologic manifestations in primary Sjögren syndrome: a study of 82 patients. Medicine 2004;83:280-291.
3. Weinshenker BG, Wingerchuk DM. Neuromyelitis optica: Clinical syn- drome and the NMO-IgG autoantibody marker. Curr Top Microbiol Im- munol 2008;318:343-356.
4. Pittock SJ, Lennon VA, Krecke K, Wingerchuk DM, Lucchinetti CF, Wein- shenker BG. Brain abnormalities in neuromyelitis optica. Arch Neurol 2006;63:390-396.
5. Binder A, Snaith ML, Isenberg D. Sjögren’s syndrome: a study of its neu- rological complications. Br J Rhematol 1988;27:275-280.
6. Manabe Y, Sasaki C, Warita H, Hayashi T, Shiro Y, Sakai K, et al. Sjögren’s syndrome with acute transverse myelopathy as the initial manifestation. J Neurol Sci 2000;176:158-161.
7. Pittock SJ, Lennon VA, de Seze J, Vermersch P, Homburger HA, Winger- chuk DM, et al. Neuromyelitis optica and non organ-specific autoimmu- nity. Arch Neurol 2008;65:78-83.
8. Hummers LK, Krishnan C, Casciola-Rosen L, Rosen A, Morris S, Ma- honey JA, et al. Recurrent transverse myelitis associated with anti-Ro (SSA) autoantibodies. Neurology 2004;62:147-149.
9. Morgan K, McFarland HF, Pillemer SR. Central nervous system disease in primary Sjögren’s syndrome: the role of magnetic resonance imaging.
Semin Arthritis Rheum 2004;34:623-630.
10. Hiwatashi A, Garber T, Moritani T, Kinoshita T, Westesson PL. Diffusion- weighted MR imaging of neuro-Behcet’s disease: a case report. Neurora- diology 2003;45:468-471.
Fig. 1. FLAIR (left), T2 weighted (middle), and T1 enhanced image (right) show irregular marginated brain swelling in midbrain and pons with mild enhance- ment. These findings are suggestive of acute demyelinating disease.