The incidence of esophageal perforations during bal- loon dilation is 0-14% (1-3). An esophageal perfora- tion is classified into three types: a type I-intramural per- foration; a type II-transmural perforation; and a type III- transmural perforation with mediastinal leakage (4).
Fasting, parenteral alimentation, and antibiotics are gen- erally used to treat types-I and II esophageal perfora- tions. However, a type III esophageal perforation show- ing progressive clinical deterioration needs to be treated surgically (4, 5). There are no reports of a successful con- servative treatment for a type III esophageal rupture af- ter esophageal balloon dilation.
We report a case of a successful conservative, non-sur- gical treatment for a transmural perforation with medi-
astinal leakage after a balloon dilation.
Case Report
A 43-year-old man was admitted to our institution complaining of intermittent swallowing difficulties with an 11 year duration. The patient had received a subtotal gastrectomy with an esophagogastrostomy 11 years ear- lier due to a bleeding ulcer in the gastric fundus, and had subsequently experienced severe swallowing diffi- culties for seven days. One year after surgery, the pa- tient received an esophageal stent at the anastomotic site because the site showed a severe focal stenosis.
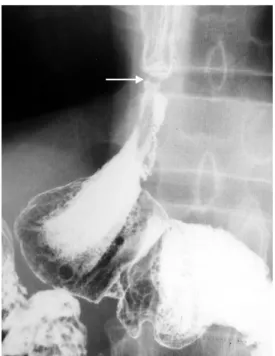
However, the stent was removed two weeks after place- ment under endoscopic guidance on account of its up- ward migration. Subsequently, the patient’s swallowing difficulty improved markedly from 2 (intolerance to soft food) to 0 (regular feeding). The patient had received esophagography at a local clinic due to swallowing diffi- culties. The esophagography showed severe focal steno- sis at the anastomotic site (Fig. 1).
J Korean Radiol Soc 2005;53:91-94
─ 91 ─
Conservative Treatment of Transmural Perforation with Mediastinal Leakage after Balloon Dilation: A Case Report1
Hyo-Sung Kwak, M.D.1, Young-Min Han, M.D.1,2, Gyung-Ho Chung, M.D.1
1Department of Radiology, 2Institute of Cardiovascular Research, Chonbuk National University Medical School
Received May 23, 2005 ; Accepted June 27, 2005
Address reprint requests to : Young-Min Han, M.D., Department of Radiology, Institute of Cardiovascular Research, Chonbuk National University Hospital,
Keumam Dong 634-18, Chonju 560-182, South Korea.
Tel. 82-63-250-1176 Fax. 82-63-272-0481 E-mail: ymhan@chonbuk.ac.kr
A 43-year-old man was admitted complaining of swallowing difficulties. The esopha- gography revealed severe stenosis at the esophagogastric anastomotic site.
Esophagography after balloon dilatation showed a transmural perforation with medi- astinal leakage. The patient was treated conservatively for one week at which time the esophagography showed no further leakage at the anastomotic site and the good pas- sage of barium. A 2-year follow-up chest computed tomography (CT) showed good pa- tency of the esophageal lumen and the marked resorption of barium in the medi- astinum.
Index words :Esophagus
Postoperative stricture Interventional procedures Perforation
Pharynx topical anesthesia was routinely performed using a lidocaine gel before the procedure. No sedatives or general anesthetic were used. The patient was then asked swallowed a small amount (10 mL) of barium in order to opacity the narrowed esophageal lumen. A 0.035-inch angled exchange guide wire (Radiofocus wire; Terumo, Tokyo, Japan) was then inserted through
the patient’s mouth, across the stricture, and into the distal part of the stomach under fluoroscopic guidance.
A deflated balloon catheter (20 mm in diameter and 3 cm long; Medi-tech/Boston Scientific, Watertown, Mass) was passed over the guide wire to span the stricture.
The balloon catheter was passed through the stricture, and inflated until the hourglass deformity had disap- peared. This inflation was repeated twice. After the pro- cedure, an esophagography revealed the extravasation of barium into the mediastinum and peritoneum, repre- senting a type III esophageal perforation (Fig. 2).
The patient was admitted to hospital and treated con- servatively by fasting, antibiotics administration, and parenteral alimentation for seven days, after which the follow-up esophagography revealed the patency of the anastomotic site and no barium leakage into the medi- astinum (Fig. 3). The patient’s diet was unrestricted after discharge. A two-year follow-up chest CT showed good patency of the anastomotic site lumen and a marked re- sorption of the barium at the mediastinum.
Discussion
Stricture formation that impedes gastric emptying is a relatively common complication after gastric surgery, and involves anastomosis creating or pyloroplasty. The duration of stricture formation after a gastrectomy varies from 13 days to 10 years (mean: 14 months).
Hyo-Sung Kwak, et al: Conservative Treatment of Transmural Perforation with Mediastinal Leakage after Balloon Dilation
─ 92 ─ Fig. 2. Immediate esophagography after the procedure reveals an esophageal perforation with barium spilling into the medi- astinum (arrows). This is a type III esophageal perforation.
Fig. 3. The one-week follow-up esophagography demonstrates good patency of the anastomotic lumen and no further barium leakage.
Fig. 1. Esophagography shows a severe focal stenosis at the anastomotic site (arrow).
Treatment of the stenosis with a fluoroscopically guided balloon dilation avoids the need for further surgery (6).
An esophageal perforation can be induced by an esophageal procedure, such as a bougienage or balloon dilation, or it can result from a spontaneous esophageal rupture, as in Boerhaave’s syndrome (5). In the case of balloon dilation, the corrosive strictures have a higher rate of esophageal perforation than a postoperative stric- ture. In corrosive stricture patients, extra caution must be taken during balloon dilation in order to avoid an esophageal perforation (3).
An esophageal perforation may be classified into three types (4). Type I involves an intramural esophageal rup- ture, which is defined as a natural drainage of leaked barium back into the esophageal lumen. Type II is a well-contained transmural rupture, which is defined as the localization of leaked barium without any spillage into the mediastinum. Type III is a transmural rupture with mediastinal spillage, which is defined as the free spillage of leaked barium into the mediastinum, pleura or peritoneum. Our patient had a type III esophageal perforation.
The treatment of an esophageal rupture normally in- volves the early surgical closure with or without rein- forcement (5). Sato et al. reported a spontaneous esophageal rupture treated successfully by conservative therapy (7), and Heindel et al. reported the successful treatment of a ruptured anastomotic esophageal stric- ture after a bougienage with a Dacron-covered nitinol stent (8). Tsunoda et al. also reported good results using a covered metallic stent for the treatment of a sponta- neous rupture of the esophagus (9). Skinner et al. em- phasized that early diagnosis of esophageal perforation is critical (5). They suggested the selective use of conser- vative treatment in the following cases: (a) patients who are clinically stable at the time of presentation and re- main so; (b) patients who had taken nothing by mouth prior to the esophageal instrumentation or balloon dila- tion, and in whom the rupture is detected before any major contamination, or patients with a perforation di- agnosed after such a long delay that they demonstrate tolerance of the perforation without the need for surgery; and (c) patients with esophageal disruptions that are well-contained within the mediastinum or a pleural loculus (5). Types I and II esophageal perfora- tions are generally treated conservatively by fasting, an- tibiotics administration, and parenteral alimentation.
Type III esophageal perforations need to be treated sur-
gically particularly if the patient shows a gradually dete- riorating clinical status (4, 5). In our case, the esophageal perforation was type III, and the barium contrast medi- um spilled out of the perforation into the mediastinum and peritoneum but was localized as a result of postop- erative adhesion. Conservative therapy was used in our case because the patient did not show a gradually deteri- orating clinical status or barium localization. The patient experienced a good recovery seven days after the proce- dure and could swallow all types of foods during the three-year follow-up.
In conclusion, type III esophageal perforation after a balloon dilation in cases of a postoperative anastomotic site stricture must be treated with caution. It is proposed that conservative treatment, such as fasting, parenteral alimentation, and intravenous antibiotics are a good al- ternative to surgery when the perforation shows locula- tion in the mediastinum or peritoneum, without a grad- ual deterioration in the patient’s clinical status.
Acknowledgements: The author is grateful to Bonnie Hami, MA, Department of Radiology, University Hospitals of Cleveland, for her editorial assistance in the preparation of this manuscript.
References
1. Maynar M, Guerra C, Reyes R, Mayor J, Garcia J, Facal P, et al.
Esophageal strictures: balloon dilation. Radiology 1988;167:703-706 2. Lange EE, Shaffer HA. Anastomotic strictures of the upper gas- trointestinal tract: results of balloon dilation. Radiology 1988;167:
45-50
3. Song HY, Han YM, Kim HN, Kim CS, Choi KC. Corrosive esophageal stricture: safety and effectiveness of balloon dilation.
Radiology 1992;184:373-378
4. Kang SG, Song HY, Lim MK, Yoon HK, Goo DE, Sung KB.
Esophageal rupture during balloon dilation of strictures of benign or malignant causes: prevalence and clinical importance. Radiology 1998;209:741-746
5. Skinner DB, Little AG, DeMeester TR. Management of esophageal perforation. Am J Surg 1980;139:760-764
6. Holt PD, de Lange EE, Shaffer HA. Strictures afte gastric surgery:
treatment with fluoroscopically guided balloon dilation. AJR Am J Roentgenol 1995;164:895-899
7. Sato T, Obinata I, Takahashi S, Sasagawa M, Wanifuchi T, Sato I, et al. Spontaneous esophageal rupture successfully treated by con- servative therapy: report of two cases. Surg Today 2002;32:421-425 8. Heindel W, Grossmann A, Fischback R, Michel O, Lackner K.
Treatment of a ruptured anastomotic esophageal stricture follow- ing bougienage with a Dacron-covered nitinol stent. Cardiovas Intervent Radiol 1996;19:431-434
9. Tsunoda S, Shimada Y, Watanabe G, Nakau M, Imamura M.
Covered metallic stent treatment of a patient with spontaneous rupture of the esophagus. Dis Esophagus 2001;14:254-257
J Korean Radiol Soc 2005;53:91-94
─ 93 ─
Hyo-Sung Kwak, et al: Conservative Treatment of Transmural Perforation with Mediastinal Leakage after Balloon Dilation
─ 94 ─
대한영상의학회지 2005;53:91-94
풍선확장술 후 발생한 종격동 누출이 동반된 식도 전층 천공의 보존치료: 증례 보고1
1전북대학교 의과대학 영상의학과, 2심혈관연구소 곽효성1・한영민1,2・정경호1
연하곤란으로 내원한 43세 남자의 식도조영술상 식도위연결술을 시행한 부위에 심한 협착이 보였다. 풍선확장술후 시행한 식도조영술에서 전층천공(벽경유뚫림)과 종격동 누출(세로관 누출)이 보였고, 일주일동안 보존치료를 한 후, 연결부위에 더 이상의 누출은 없었고, 바륨 통과도 잘 되었다. 2년의 흉부 전산화단층촬영(CT) 추적검사에서 식도내강 은 잘 유지되며, 종격동내 바륨도 흡수되었다.