INTRODUCTION
Coronavirus disease 2019 (COVID-19) is a newly identified in- fectious disease with rapid human to human transmission capaci- ty. COVID-19 can result in several fatal complications such as acute respiratory distress syndrome, RNAaemia, acute cardiac in- jury, acute kidney injury, secondary infection, and septic shock [1,2]. Since February 21, 2020, the authors of this paper have been working at a hospital designated for treating COVID-19 pa- tients and by June 15, 2020, 1,027 COVID-19 patients had been
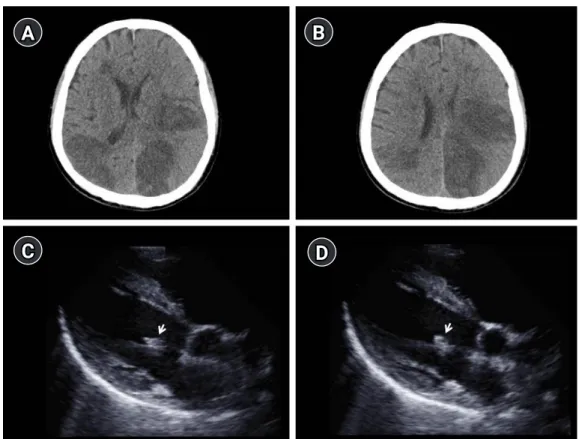
Cerebral infarction caused by
endocarditis in a patient with COVID-19
Doo Hyuk Kwon, MD 1 ; Jae-Seok Park, MD 2 ; Hyung Jong Park, MD 1 ; Sung-Il Sohn, MD 1 ; Jeong-Ho Hong, MD, PhD 1
1
Department of Neurology, Keimyung University School of Medicine, Daegu, Republic of Korea
2