저작자표시-비영리-변경금지 2.0 대한민국 이용자는 아래의 조건을 따르는 경우에 한하여 자유롭게 l 이 저작물을 복제, 배포, 전송, 전시, 공연 및 방송할 수 있습니다. 다음과 같은 조건을 따라야 합니다: l 귀하는, 이 저작물의 재이용이나 배포의 경우, 이 저작물에 적용된 이용허락조건 을 명확하게 나타내어야 합니다. l 저작권자로부터 별도의 허가를 받으면 이러한 조건들은 적용되지 않습니다. 저작권법에 따른 이용자의 권리는 위의 내용에 의하여 영향을 받지 않습니다. 이것은 이용허락규약(Legal Code)을 이해하기 쉽게 요약한 것입니다. Disclaimer 저작자표시. 귀하는 원저작자를 표시하여야 합니다. 비영리. 귀하는 이 저작물을 영리 목적으로 이용할 수 없습니다. 변경금지. 귀하는 이 저작물을 개작, 변형 또는 가공할 수 없습니다.
Analysis of ultrasonic parameters of pylorus
in idiopathic hypertrophic pyloric stenosis
patients: a retrospective study
by
Joohyun Sim
Major in Medicine
Department of Medical Sciences
The Graduate School, Ajou University
Analysis of ultrasonic parameters of pylorus
in idiopathic hypertrophic pyloric stenosis
patients: a retrospective study
by
Joohyun Sim
A Dissertation Submitted to The Graduate School of
Ajou University in Partial Fulfillment of the
Requirements for the Degree of
Master of Medicine
Supervised by
Jeong Hong, M.D., Ph.D.
Major in Medicine
Department of Medical Sciences
The Graduate School, Ajou University
This certifies that the dissertation
of Joohyun Sim is approved.
SUPERVISORY COMMITTEE
Jeong Hong
Chang-Kwon Oh
Je Hwan Won
The Graduate School, Ajou University
December, 23rd, 2019
i
- ABSTRACT -
Analysis of ultrasonic parameters of pylorus in idiopathic
hypertrophic pyloric stenosis patients: a retrospective study
Purpose: Pyloric muscle thickness (PMT) equal to or greater than 4mm and canal length
equal to or greater than 16mm are widely accepted for diagnosis of idiopathic hypertrophic pyloric stenosis (IHPS). However, up to 25% of IHPS patients show discordant ultrasonic parameters compared to current diagnostic criteria. We analyzed the ultrasonic parameters of pylorus of IHPS patients to discover their correlation to patient characteristics and aimed to find a new diagnostic value.
Method: Medical records of 131 IHPS patients who received pyloromyotomy from 1994 to
2016 were reviewed. All patients presented with characteristic clinical symptoms. The patients were divided into two groups according to their eligibility for current criteria as Discordance group (n=32) and Concordance group (n=99). Baseline characteristics were reviewed and ultrasonic parameters were measured, and then the volume of the pylorus was estimated by calculation using the parameters.
Results: The proportion of neonates were higher in Discordance group (43.8% vs.13.1%,
p<0.001). Mean postconceptional age of Concordance group was 19.4 days older than that of Discordance group at the time of US examination (p<0.001). Average weight of Concordance group was 4.29±0.74kg while that of Discordance group were 3.76±0.91kg. Also, the median chronological age at the time of US was 28.0 [21, 35] days in Discordance group and 44.0 [29.5, 54.5] days in Concordance group (p<0.001). In Discordance group,
ii
proportion of PMT over PD was 31.87±3.24%, while it was 35.06±3.61 % in Concordance group. Postconceptional age and being neonate were remained as significant variables after multivariate linear regression (R2=0.390).
Conclusion: Pyloric volume of IHPS patients were strongly related to their postconceptional
age, and it suggested that the diagnostic criteria may differ according to the patient’s size and time of diagnosis. Future diagnostic criteria for IHPS should reflect the dynamic nature of the patients.
iii
TABLE OF CONTENTS
ABSTRACT ··· ⅰ
TABLE OF CONTENTS ··· iii
LIST OF FIGURES ··· iv LIST OF TABLES ··· v I. INTRODUCTION ··· 1 II. METHODS ··· 3 A. STUDY POPULATION ··· 3 B. DATA COLLECTION ··· 5 C. STATISTICAL ANALYSIS ··· 8 III. RESULTS ··· 9 A. BASELINE CHARACTERISTICS ··· 9
B. ULTRASONIC PARAMETERS OF THE PATIENTS ··· 10
C. PYLORIC MUSCLE VOLUME AND RELATED FACTORS ··· 13
IV. DISCUSSION ··· 15
V. CONCLUSION ··· 18
REFERENCES ··· 19
iv
LIST OF FIGURES
Fig. 1. Study population. ··· 4
Fig. 2.
Calculation of the volume of pylorus with the pipe model.
··· 7v
LIST OF TABLES
Table 1. Baseline characteristics. ··· 6
Table 2. Ultrasonic measurements of pylorus ··· 11
Table 3. Pearson correlation. ··· 14
Table 4. Partial correlation. ··· 14
- 1 -
I. INTRODUCTION
Idiopathic Hypertrophic Pyloric Stenosis (IHPS) is one of the most common causes of abdominal surgery in neonates and infants. Incidences reported are 2 to 5 in 1000 live births and as high as 8.2 to 12.3 cases per 1000 live births in United States [1-3]. It is an idiopathic cause of gastric outlet obstruction, which typically occurs during the 2nd to 12th week of life and is more common in boys than girls [4, 5]. Premature infants tend to present at a later chronological age than term infants [6, 7]. Clinical diagnosis is easily made with characteristic symptoms such as nonbilious vomiting and hypochloremic hypokalemic metabolic alkalosis. Treatment is open or laparoscopic pylorotomy, while some reports natural course without surgery [8].
Although thorough examination is sufficient to establish the diagnosis without the need for any imaging modality[9], upper gastrointestinal study with contrast was once considered the test of choice. In these days, ultrasonography has become a critical adjunct in confirming the diagnosis of IHPS by measuring pyloric muscle thickness (PMT) and canal length (PCL).
However, there is some discrepancy in the literature concerning the diagnostic criteria which should be used to interpret an US study result as abnormal. Also, clinical diagnosis of IHPS is inconclusive in 15-25% of cases[10]. In Republic of Korea, as suggested by Stunden et al.[11], diagnostic criteria of PMT equal to or greater than 4mm and PCL equal to or greater than 15mm are widely accepted in consensus of pediatric surgeons[12]. Diagnostic criteria of ultrasonography may differ in other countries, as PMT equal to or greater than 3 to 4mm and PCL equal to or greater than 15 to 18mm are reported in many previous studies [3-5, 13]. In several studies, pyloric volume was calculated with ultrasonic measurements to suggest a novel diagnostic criteria for IHPS because of discordance between clinical symptoms and
- 2 -
measured parameters. Westra et al.[14] suggested that pyloric volume of 1.4mL or more as volumetric criteria. Rohrschneider et al.[9] showed in their study with 85 IHPS patients that they had a mean pyloric volume of 2.7±1.1mL while normal group had a mean pyloric volume of 0.6±0.3mL. In Korea, Lee et al. [15] showed a result with average pyloric volume of 3.26± 1.38 mL.
We analyzed ultrasonic parameters of pylorus retrospectively in IHPS patients and compared to see any discordance with current diagnostic criteria. We also analyzed if the parameters were proportional to specific patient factors such as chronological age at presentation, duration of symptoms, body measurements, and other gestational factors. This is the first series of Korean IHPS patients which compared the characteristics of those who fulfill the criteria and those who do not.
- 3 -
II. METHODS
A. Study population
We reviewed the medical records of 322 pediatric patients who underwent Fredet-Ramstedt pyloromyotomy after diagnosis of IHPS from May 1994 to December 2016. All were confirmed with pyloric hypertrophy in the operational field according to their operational record. Among them, electronically accessible ultrasonic records were available for 131 patients. As a result, 131 patients were selected for the final analysis (Fig. 1). The patients were divided into two groups according to the current IHPS criteria used in Korea. Thirty two patients with pyloric muscle thickness thinner than 4mm or canal length shorter than 16mm were grouped as Discordance group and 99 patients who fulfilled the criteria for both dimensions were called Concordance group.
- 4 - Figure 1. Study Population
- 5 -
B. Data collection
Baseline characteristics of each patient were collected from the electronic medical records (Table 1). Pyloric parameters of the patients were not remained in the electronic medical record archives, so they were measured on the saved images of the preoperative ultrasonography using picture archiving and communication system (PACS). The muscle thickness was measured for the muscularis propria only, excluding other layers such as mucosa, submucosa, and serosa on the cross-sectional image of pylorus. The diameter was measured for the longest line across the middle portion of the cross-sectional pylorus. The canal length was re-measured as well, for the longest length of the canal shown among the captured images.
For volumetric analysis of pylorus, pyloric volume was calculated to visualize the amount of hypertrophy. The volume of the pylorus was estimated by calculation of the volume of a pipe (Fig.2).
The study was approved by the Institutional Review Board (AJIRB-MED-MDB-19-240), and informed consents were waived due to its retrospective study design.
- 6 - Table 1. Baseline characteristics
Discordance n=32 Concordance n=99 p-value Sex, M:F 25:7 77:22 0.967 Neonates, n (%) 14 (43.8) 13 (13.1) <0.001 Prematurity, n (%) 6 (18.8) 9 (9.1) 0.197*
Gestational Age (Days) 271.03±14.87 271.51±14.30 0.869
Postconceptional Age (Days) 300.41±15.41 319.81±22.74 <0.001 Weight at Birth (kg) 3.08±0.73 3.30±0.62 0.100 Weight at US (kg) 3.76±0.91 4.29±0.74 0.001 Height at US (cm) 53.58±4.50 55.58±3.77 0.029 BMI (kg/m2) 13.16±2.19 13.89±1.83 0.098 Duration of Symptom (Days) 6.5 [3.5, 9.5] 14.0 [6.5, 21.5] <0.001** Chronological Age at US (days) 28.0 [21, 35] 44.0 [29.5, 54.5] <0.001**
* Fisher’s exact test. **Mann-Whitney U test. Values are expressed in mean±standard deviation or median [interquartile range]. US, Ultrasonography; BMI, Body Mass Index.
- 7 -
- 8 -
C. Statistical analysis
Student’s t-test and Mann-Whitney-U test were used to compare the continuous variables between the two groups, which were expressed as mean standard deviation or median [interquartile range (IQR)]. The categorical variables were presented as frequency (%) and statistically compared using the chi-square or Fisher’s exact test when appropriate. Related factors of the patients and pyloric muscle volume were evaluated by Pearson correlation and partial correlation. Multiple linear regression analysis was performed for variables that showed statistical significance in correlations. Statistical analysis was performed using SPSS® Statistics 25.0 (IBM Corp., Armonk, NY).
- 9 -
III. RESULTS
A. Baseline characteristics
A total of 32 patients were classified as Discordance group and 99 patients were classified as Concordance group (Table 1). The Discordance group, whose initial diagnosis was inconclusive because of the discordance to known criteria, made up to 24.4% of the total population. In both groups, male to female ratio was about 3.5:1.
The proportions of neonates were 43.8% in Discordance group and 13.1% in Concordance group, which had a statistical significance (p<0.001). Although the proportion of premature patients with gestational age < 37 weeks were 18.8% and 9.1% in Discordance group and Concordance group respectively, they did not have a statistical significance. In both groups, mean gestational age was 271 days, which could be converted to 38 weeks and 5 days. However, postconceptional age showed a difference between the two groups. Concordance group showed a mean of 19.4 days of older postconceptional age at the time of US examination, and it also had a statistical significance (p<0.001).
Body weight at the time of birth did not show statistically significant difference but the body weight and height at the time of US examination showed a statistical significance. Concordance group was 4.29±0.74kg in weight and 53.58±4.50cm in height while Discordance group was 3.76±0.91kg and 55.58±3.77cm, respectively. However, Body Mass Index (BMI) did not show a significant difference. The median duration of symptom was shorter in Discordance group (6.5 [3.5, 9.5] days) than in Concordance group (14.0 [6.5, 21.5] days), which had a statistical significance (p<0.001). Also, the median chronological age at the time of US was 28.0 [21, 35] days in Discordance and 44.0 [29.5, 54.5] days in Concordance groups (p<0.001)
- 10 -
B. Ultrasonic parameters of the patients
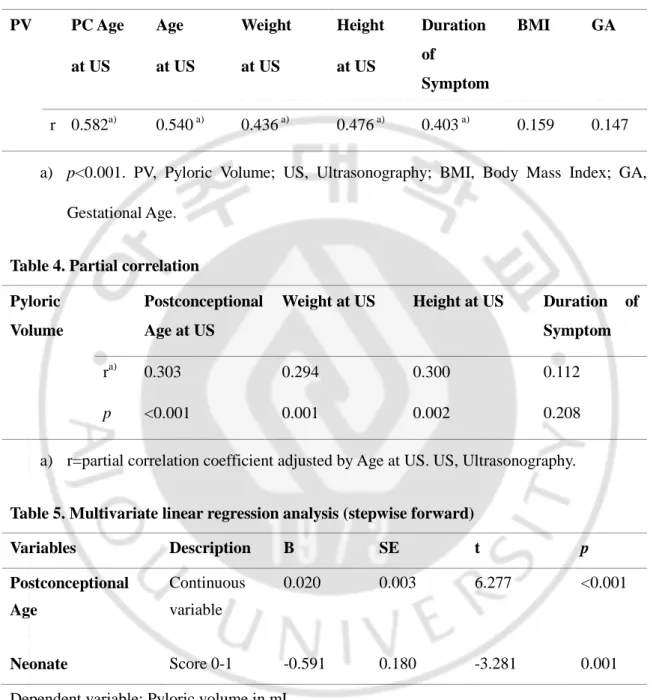
Values of pyloric muscle thickness (PMT) were significantly higher in Concordance group (3.74±0.35 vs. 4.86 0.59, p<0.001). Values of pyloric canal length (PCL), pyloric diameter (PD), and pyloric volume (PV) were also higher in Concordance group (Table2). However, the volume of lumen were not different in both groups (0.29±0.18 vs. 0.33±0.21, p=0.423). Thus, the proportion of lumen volume to pyloric volume was significantly higher in Discordance group. In Discordance group, proportion of PMT in PD was 31.87±3.24%, while it was 35.06± 3.61 % in Concordance group. In all IHPS patients, PMT/PD was same or greater than 0.27 (Fig.3).
- 11 - Table 2. Ultrasonic measurements of pylorus
Discordance n=32
Concordance n=99
p- value
Pyloric Muscle Thickness (mm) 3.74±0.35 4.86±0.59 <0.001
Pyloric Canal Length (mm) 17.99±3.36 21.26±2.89 <0.001
Pyloric Diameter 11.79±1.16 13.92±1.50 <0.001
Pyloric Volume (mL) 1.72±0.49 2.98±0.87 <0.001
Lumen Volume (mL) 0.29±0.18 0.33±0.21 0.423
% of Lumen/Pyloric volume 16.00±6.18 10.67±5.34 <0.001
% of PMT/PD 31.87±3.24 35.06±3.61 <0.001
Values are expressed in mean standard deviation. PMT, Pyloric Muscle Thickness; PD, Pyloric Diameter.
- 12 - Figure 3. Histogram for PMT/PD in all IHPS patients
- 13 -
C. Pyloric muscle volume and related factors
Pearson correlation between pyloric muscle volume and several factors were shown in Table 3. Postconceptional age, chronological age, weight, and height at the time of US examination seemed to have correlation with pyloric muscle volume (p<0.001). Partial correlation between above factors and pyloric volume was analyzed with adjustment by chronological age (Table 4). Then duration of symptom turned to be statistically insignificant. Multivariate linear regression analysis was performed with significant variables and a dummy variable (Table 5). If the patient was a neonate under chronological age of 28 days, it was scored as 1, while infants were scored as 0. Postconceptional age and being neonate remained as significant variables (R2=0.390).
- 14 - Table 3. Pearson correlation
PV PC Age at US Age at US Weight at US Height at US Duration of Symptom BMI GA r 0.582a) 0.540 a) 0.436 a) 0.476 a) 0.403 a) 0.159 0.147
a) p<0.001. PV, Pyloric Volume; US, Ultrasonography; BMI, Body Mass Index; GA, Gestational Age.
Table 4. Partial correlation Pyloric
Volume
Postconceptional Age at US
Weight at US Height at US Duration of Symptom
ra) 0.303 0.294 0.300 0.112
p <0.001 0.001 0.002 0.208
a) r=partial correlation coefficient adjusted by Age at US. US, Ultrasonography.
Table 5. Multivariate linear regression analysis (stepwise forward)
Variables Description B SE t p Postconceptional Age Continuous variable 0.020 0.003 6.277 <0.001 Neonate Score 0-1 -0.591 0.180 -3.281 0.001
Dependent variable: Pyloric volume in mL Coefficient B=-3.563, p=0.001
- 15 -
IV. DISCUSSION
Diagnostic imaging modality of IHPS has been evolved although clinical diagnosis can be made with characteristic symptoms. Upper gastrointestinal study with contrast was once considered the test of choice but advances in real-time ultrasonography has become a critical adjunct in confirming the diagnosis of IHPS by measuring PMT and PCL. Furthermore, evaluation of peristaltic movement and gastric emptying by ultrasonography was considered as an aid to the morphologic diagnostic criteria. However, unlike definite numbers, evaluation of functional aspects of pylorus would be subjective to radiologists.
Up to 25% of IHPS patients are initially inconclusive in diagnosis because even though their symptoms are present, ultrasonic measurements do not fulfill the criteria. In our cohort, IHPS patients discordant to diagnostic criteria were 24.4%, and this was similar to previous report [10]. According to our data, the characteristics of these patients tend to be “smaller” in size and “younger” in age, in terms of body weight, height, and chronological age and postconceptional age at presentation. Iqbal et al. also suggested in their series of 318 ultrasounds, that there were correlation between age and weight and the measurements of the pylorus [3].
The authors chose the postconceptional age as a variable because the number of premature infants were too small to undergo statistical analysis. Also, duration of vomiting symptom tends to be shorter in the Discordance group but this variable did not show correlation to pyloric volume after adjustment by chronological age. Although Hsu et al. suggested size of pylorus did not matter in diagnosis of IHPS [16], out result showed that smaller pylorus can be a hypertrophic pylorus in smaller infants.
- 16 -
popularized due to complexness of its calculation and possible errors in measuring the dynamic shape of the pylorus. Simplifying the curved pipe to a straight pipe, Westra et al.[14] suggested a cutoff value of 1.4mL to confirm the diagnosis of IHPS. According to our result, the smallest value of pyloric volume was 0.95mL and 94.7% of the patients met the criteria.
In the multivariate linear regression model in predicting pyloric volume, postconceptional age and being a neonate were two factors that showed statistical significance. Although the equation may not be able to suggest a pathologic limit of pyloric volume in all patients, it could be interpreted that the pathologic pyloric volume could be a dynamic value according to patient factors, not a set number.
An interesting finding among the ultrasonic parameters is the proportion of PMT to PD. Pyloric diameter consists of thickness of two muscle layers and a lumen diameter. The proportion of single layer of PMT to the PD was 31.87±3.24% in the Discordance group while 35.06±3.61% in the Concordance group. Although this study was conducted without a control group, Rohrschneider et al.[9] reported that the PD and PMT of normal group were 8.4±1.7mm and 1.8±0.5mm, respectively. Calculating the proportion of mean PMT to mean PD according to their data, it would be 21.43% in the normal group, and IHPS group had PMT of 4.7±0.9mm and PD of 14±2mm, and the proportion of mean PMT to mean PD would be 33.57% in the IHPS group. Since all patients in our cohort who were diagnosed of IHPS showed more than 27% of PMT/PD regardless of their age and size, it could be possible that proportion of PMT to PD over 27% would be adjunct diagnostic criteria in “smaller” and “younger” IHPS patients who do not meet the current ultrasonic criteria. Further study should be conducted with a control group to evaluate if there exists a diagnostic value in the proportion of PMT to PD in the
- 17 -
patients suspected to have IHPS.
The limitation of this study is that this is a retrospective study conducted in a single center in Korea. Also, this study includes IHPS patients only, due to its retrospective nature. A larger cohort with a control group is needed to review possible diagnostic criteria of IHPS patients discordant to current diagnostic criteria.
- 18 -
V. CONCLUSION
While treatment for IHPS is relatively easy, diagnosis is still an enigma. Because up to 25% of IHPS patients show discordant ultrasonic parameters compared to current diagnostic criteria, our study tried to search for other variables that could be used in adjunct. However, our study shows that pyloric volume of IHPS patients were strongly related to their postconceptional age, and it suggested that the diagnostic criteria may not be a set value that could be measured. Also, the proportion of PMT to PD in IHPS patients was never mentioned in other studies before but it needs to be proven in further studies. Future diagnostic criteria for IHPS should reflect the dynamic nature of the patients.
- 19 -
REFERENCES
[1] Leaphart CL, Borland K, Kane TD, Hackam DJ. Hypertrophic pyloric stenosis in newborns younger than 21 days: remodeling the path of surgical intervention. J Pediatr Surg. 2008;43:998-1001.
[2] Safford SD, Pietrobon R, Safford KM, Martins H, Skinner MA, Rice HE. A study of 11,003 patients with hypertrophic pyloric stenosis and the association between surgeon and hospital volume and outcomes. J Pediatr Surg. 2005;40:967-72; discussion 72-3.
[3] Iqbal CW, Rivard DC, Mortellaro VE, Sharp SW, St Peter SD. Evaluation of ultrasonographic parameters in the diagnosis of pyloric stenosis relative to patient age and size. J Pediatr Surg. 2012;47:1542-7.
[4] Gale HI, Gee MS, Westra SJ, Nimkin K. Abdominal ultrasonography of the pediatric gastrointestinal tract. World J Radiol. 2016;8:656-67.
[5] El-Gohary Y, Abdelhafeez A, Paton E, Gosain A, Murphy AJ. Pyloric stenosis: an enigma more than a century after the first successful treatment. Pediatr Surg Int. 2018;34:21-7.
[6] Costanzo CM, Vinocur C, Berman L. Prematurity Affects Age of Presentation of Pyloric Stenosis. Clin Pediatr (Phila). 2017;56:127-31.
[7] Lee SK, Kim SH, Lee WY, Kim HH. Infantile hypertrophic pyloric stenosis:clinical differences between premature and full-term Infants. J Korean Assoc Pediatr Surg. 1998;4:34-8. [8] Lim CW, Park HK, Yeom JS, Park T, Park JS, Youn HS, et al. A natural course of an infantile hypertrophic pyloric stenosis without adequate surgical procedure. J Korean Assoc Pediatr Surg. 2015;21:46-9.
- 20 -
[9] Rohrschneider WK, Mittnacht H, Darge K, Troger J. Pyloric muscle in asymptomatic infants: sonographic evaluation and discrimination from idiopathic hypertrophic pyloric stenosis. Pediatr Radiol. 1998;28:429-34.
[10] Tunell WP, Wilson DA. Pyloric stenosis: diagnosis by real time sonography, the pyloric muscle length method. J Pediatr Surg. 1984;19:795-9.
[11] Stunden RJ, LeQuesne GW, Little KE. The improved ultrasound diagnosis of hypertrophic pyloric stenosis. Pediatr Radiol. 1986;16:200-5.
[12] Huh YS, Lim MK, Kim KR. Clinical analysis of infantile hypertrophic pyloric stenosis. J Korean Assoc Pediatr Surg. 1998;4:39-47.
[13] Miura S, Haku E, Hirai T, Marugami N, Itoh T, Tanaka T, et al. Ultrasound follow-up of infantile hypertrophic pyloric stenosis (IHPS) during conservative therapy: ultrasound findings as criteria for diagnosis and cure. J Med Ultrasonics. 2008;35:51-6.
[14] Westra SJ, de Groot CJ, Smits NJ, Staalman CR. Hypertrophic pyloric stenosis: use of the pyloric volume measurement in early US diagnosis. Radiology. 1989;172:615-9.
[15] Lee SK, Oh JW, Oh YK, Kim CG. Ultrasonographic diagnosis by pyloric volume measurement in congenital hypertrophic pyloric stenosis. J Korean Pediatr Soc. 1994;37:1595-9. [16] Hsu P, Klimek J, Nanan R. Infantile hypertrophic pyloric stenosis: does size really matter? J Paediatr Child Health. 2014;50:827-8.
- 21 - -국문요약-
비후성 유문 협착증에서 초음파를 이용한 유문근 측정값에 대한
후향적 분석
아주대학교 대학원 의학과 심 주 현 (지도교수: 홍 정) 서론: 영아기의 비후성 유문 협착증(IHPS)은 비교적 흔한 복부수술의 원인 질환으로 특징적인 구토 증상과 혈중 전해질 이상 소견으로 임상적 진단이 쉽게 내려진다. 확진은 복부초음파를 통한 유문근 두께 및 길이 측정으로 가능하다. 진단 기준은 문헌마다 차이는 있으나 두께는 3mm이상, 유문관의 길이는 15mm 이상으로 널리 이용되고 있다. 저자들은 IHPS로 진단되어 수술을 시행한 환아에서 후향적으로 초 음파 소견을 분석하여 공용되고 있는 초음파 소견의 진단 기준과 차이가 있는지 비 교하여 보고자 하였다. 또한 유문근의 직경, 두께 및 길이의 측정값이 환아의 특정 인자들과 비례적인 상관관계가 있는지 확인하고자 하였다. 방법: 본원에서 1994년부터 2016년까지 IHPS 로 진단되어 수술을 시행받은 131명의 환아를 대상으로 후향적으로 분석하였다. 모두 특징적인 임상 증상으로 복부 초음 파를 시행하였고 개복을 통한 유문근절개술시 모두 유문근 비후가 확인되었다. 분 석을 위해 수술 전 초음파 소견상 보이는 유문근의 두께, 직경, 유문관 길이를 다시- 22 - 정밀하게 계측하였다. 근육 두께는 유문부 단면에서 장막층, 점막하층, 유문관의 점 막층을 제외한 근육 부분을, 직경은 유문부의 중심 부분 중 최대 길이를 측정하였 다. 유문관 길이 역시 재측정하였다. 유문근의 두꺼워진 정도를 비교하기 위해 유문 근 용적을 계산하였고 환아의 각 항목과 유문근 용적의 관계는 이변량 상관계수 및 편상관관계 분석을 이용하여 확인하였다. 결과: 환아들은 한국에서 통용되는 유문근 비후 진단기준 (유문근 두께 4mm 이상, 유문관 길이 16mm 이상)에 부합하는 군과 적합한 군으로 나누어 비교하였다. 신생 아 비율은 부합군에서 더 높았다 (43.8% vs.13.1%, p<0.001). 평균 교정연령은 적합군 이 부합군보다 19.4일 많았고 초음파 검사시 평균 몸무게 또한 4.29 0.74kg로 3.76 0.91kg인 부합군보다 높게 측정되었다. 또한 검사 당시 출생 후 일수는 부합군 에서 중위수가 28일, 적합군에서 44일로 적합군이 더 많았다. 부합군에서 유문 직경 대비 유문근 두께의 비율은 31.87 3.24%이며 적합군에서는 35.06 3.61 %로 나타났 다. 교정연령과 신생아여부는 다변량 선형회귀분석에서도 통계학적으로 유의하게 나타났다. (R2 =0.390) 결론: 유문근비후 환아의 유문근용적은 교정연령과 연관성이 높게 나타났다. 따라서 이는 환아의 크기와 진단 시기에 따라 진단기준이 다르게 적용되어야 할 것이라 보 여진다. 추후 유문근비후증의 진단기준은 이러한 환아들의 동적 변수들이 반영되어 야 할 것으로 보인다.