I N F E C T I O N C O N T R O L AND H O S P I T A L E P I D E M I O L O G Y N O V E M B E R 2 0 1 2 , V O L . 3 3 , N O . 11
O R I G I N A L A R T I C L E
Differences in the Risk Factors for Surgical Site Infection between
Total Hip Arthroplasty and Total Knee Arthroplasty in the Korean
Nosocomial Infections Surveillance System (KONIS)
Kyoung-Ho Song, MD;1 Eu Suk Kim, MD;1 Young Keun Kim, MD;2 Hye Young Jin, RN;3 Sun Young Jeong, RN;4
Yee Gyung Kwak, MD;5 Yong Kyun Cho, MD;6 Joohon Sung, PhD;7 Yeong-Seon Lee, PhD;8 Hee-Bok Oh, PhD;8
Tae Kyun Kim, MD;9 Kyung-Hoi Koo, MD;9 Eui-Chong Kim, MD;10 June Myung Kim, MD;11 Tae Yeol Choi, MD;12
Hyo Youl Kim, MD;2 Hee Jung Choi, MD;15'' Hong Bin Kim, M D ;U KONIS Study Groupb
OBJECTIVE. To compare the characteristics and risk factors for surgical site infections (SSIs) after total hip arthroplasty (THA) and total knee arthroplasty (TKA) in a nationwide survey, using shared case detection and recording systems.
DESIGN. Retrospective cohort study.
SETTING. Twenty-six hospitals participating in the Korean Nosocomial Infections Surveillance System (KONIS). PATIENTS. From 2006 to 2009, all patients undergoing THA and TKA in KONIS were enrolled.
RESULTS. SSI occurred in 161 (2.35%) of 6,848 cases (3,422 THAs and 3,426 TKAs). Pooled mean SSI rates were 1.69% and 2.82% for THA and TKA, respectively. Of the cases we examined, 42 (26%) were superficial-incisional SSIs and 119 (74%) were "severe" SSIs; of the latter, 24 (15%) were deep-incisional SSIs and 95 (59%) were organ/space SSIs. In multivariate analysis, a duration of preoperative hospital stay of greater than 3 days was a risk factor for total SSI after both THA and TKA. Diabetes mellitus, revision surgery, prolonged duration of surgery (above the 75th percentile), and the need for surgery due to trauma were independent risk factors for total and severe SSI after THA, while male sex and an operating room without artificial ventilation were independent risk factors for total and severe SSI after TKA. A large volume of surgeries (more than 10 procedures per month) protected against total and severe SSI, but only in patients who underwent TKA.
CONCLUSIONS. Risk factors for SSI after arthroplasty differ according to the site of the arthroplasty. Therefore, clinicians should take into account the site of arthroplasty in the analysis of SSI and the development of strategies for reducing SSI.
Infect Control Hosp Epidemiol 2012;33(11):1086-1093
Total hip arthroplasty (THA) and total knee arthroplasty suggested that the risk factors for prosthetic joint infection (TKA) are frequent orthopedic surgical procedures in Korea.1 may differ according to which joint is replaced.6 However, Although surgical site infection (SSI) after arthroplasty is un- most studies have not considered the site of arthroplasty, and common, it is associated with substantial morbidity and eco- there are unresolved issues concerning the risk factors for SSI nomic cost,2"4 and identifying correctable risk factors is im- after arthroplasty.7 We have performed a retrospective cohort portant in reducing its incidence.5 It has recently been study on a large number of Korean patients undergoing THA
Affiliations: 1. Department of Internal Medicine, Seoul National University Bundang Hospital, Seongnam, Republic of Korea; 2. Department of Internal Medicine, Yonsei University Wonju College of Medicine, Wonju, Republic of Korea; 3. Infection Control Office, Ajou University Hospital, Suwon, Republic of Korea; 4. Infection Control Office, Ewha Womans University Mokdong Hospital, Seoul, Republic of Korea; 5. Department of Internal Medicine, Inje University Ilsan Paik Hospital, Goyang, Republic of Korea; 6. Division of Infectious Diseases, Gachon University Gil Hospital, Incheon, Republic of Korea; 7. Department of Epidemiology and Institute of Environment and Health, Seoul National University School of Public Health, Seoul, Republic of Korea; 8. Center for Infectious Diseases, Korea National Institute of Health, Osong, Republic of Korea; 9. Department of Orthopedic Surgery, Seoul National University Bundang Hospital, Seongnam, Republic of Korea; 10. Department of Laboratory Medicine, Seoul National University College of Medicine, Seoul, Republic of Korea; 11. Division of Infectious Diseases, Yonsei Medical Center, Seoul, Republic of Korea; 12. Department of Laboratory Medicine, Hanyang University Hospital, Seoul, Republic of Korea; 13. Department of Internal Medicine, Ewha Womans University College of Medicine, Seoul, Republic of Korea.
'These authors contributed equally to this article. ••Participating hospitals are listed in "Acknowledgments."
D I F F E R E N T RISK F A C T O R S FOR SSI B E T W E E N T H A AND TKA I O 8 7
and TKA to characterize and identify the risk factors asso-ciated with SSIs according to site of arthroplasty, using pro-spective data from the Korean Nosocomial Infections Sur-veillance System (KONIS).810
METHODS SSI Surveillance
Twenty-six hospitals participated in this prospective survey of SSIs occurring after arthroplasty, as part of the KONIS from 2006 to 2009.8"10 A basic requirement of participating hospitals was to have at least 1 full-time infection control practitioner on staff. The hospitals in this survey volunteered to participate on a yearly basis, and consecutive 6-month surveillance from July to December was mandatory. All pa-tients were enrolled in a common web-based case-recording system and were followed up at intervals for 1 year. Surgical site examination was performed by the attending surgeon or, if necessary, by an infectious diseases specialist. Clinical in-formation was reviewed by independent infection control practitioners in a prospective manner. Patients who failed to return for clinical follow-up were telephoned by an infection control practitioner to complete a standardized form. During the follow-up period, patients suspected of having SSI were identified by surgeons and infection control practitioners, using the criteria of the Centers for Disease Control and Prevention (CDC).11 In this article, deep-incisional and or-gan/space SSIs are referred to as "severe" SSIs, whereas "total" SSIs also include superficial-incisional SSIs.1213
Data Collection
We collected demographic data on the following factors: Hos-pital-related factors were hospital size, monthly number of surgeries, and operating room characteristics. Operating
room characteristics were divided into 3 categories according to the nature of the ventilation system in the operating room: (1) high-efficiency particulate air (HEPA)-filtered laminar airflow ventilation, (2) conventional turbulent ventilation with HEPA-filtered air, and (3) no artificial ventilation.7 Pre-and perioperative factors were duration of preoperative hos-pital stay, wound class,14 American Society of Anesthesiology (ASA) physical score,15 duration of surgery, emergency status, need for surgery due to trauma, and surgery performed under general anesthesia, among others (see Table 2 for a complete list). Variables associated with antimicrobial prophylaxis (AMP) were time of first dose and choice and duration of therapy. Parenteral AMP initiated within 1 hour before in-cision for cephalosporins or within 2 hours for vancomycin or fluoroquinolones was considered to be appropriate timing of administration.16
Statistical Analyses
Differences between patients with SSI and patients without SSI were analyzed using the x2 test for categorical variables and the t-test for continuous variables. To identify indepen-dent risk factors for SSI, a stepwise multiple logistic regression model was used. Risk factors with P values of less than .10 in univariate analysis were included in the initial model, and forward stepwise selection was performed to define significant risk factors. P values of less than .05 were considered to be statistically significant in the multivariate analysis. National Nosocomial Infections Surveillance (NNIS) risk index cate-gories were excluded from the multivariate analysis because each component was already included in the model. In the analysis of AMP, patients who had received preoperative an-tibiotics for infections at any anatomical sites were excluded. PASW for Windows (ver. 18; SPSS) was used for all statistical analyses in this study.
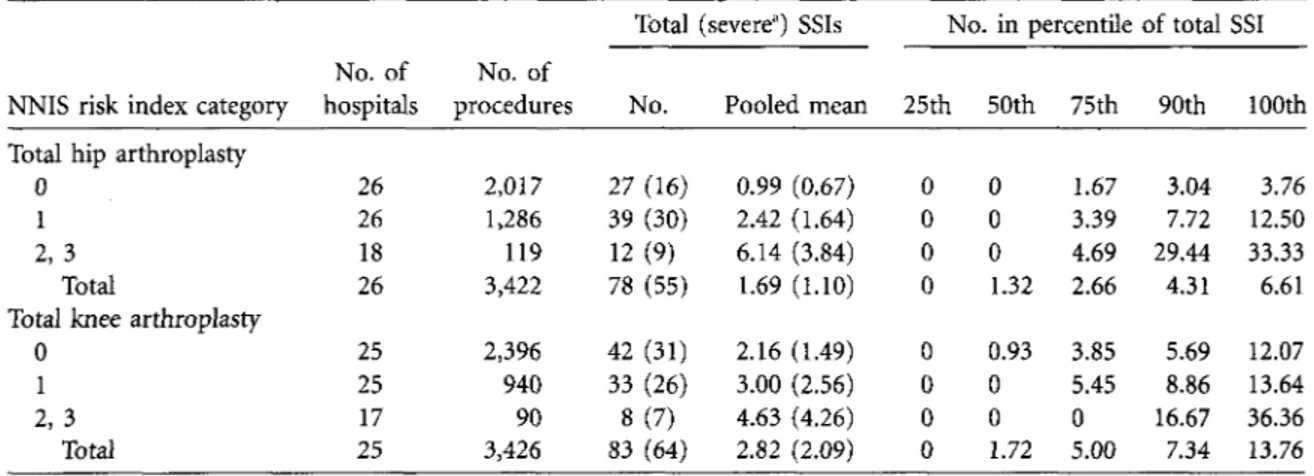
TABLE i. Pooled Means and Key Percentiles of the Distribution of Rates of Surgical Site Infection (SSI) after Total Hip Arthroplasty and after Total Knee Arthroplasty
Total (severe*) SSIs No. in percentile of total SSI NNIS risk index category
No. of hospitals
No. of
procedures No. Pooled mean 25th 50th 75th 90th 100th Total hip art
0 1 2, 3
Total
hroplasty
Total knee arthroplasty 0 1 2,3 Total 26 26 18 26 25 25 17 25 2,017 1,286 119 3,422 2,396 940 90 3,426 27 (16) 39 (30) 12(9) 78 (55) 42 (31) 33 (26) 8(7) 83 (64) 0.99 (0.67) 2.42 (1.64) 6.14 (3.84) 1.69 (1.10) 2.16 (1.49) 3.00 (2.56) 4.63 (4.26) 2.82 (2.09) 0 0 0 0 0 0 0 0 0 0 0 1.32 0.93 0 0 1.72 1.67 3.39 4.69 2.66 3.85 5.45 0 5.00 3.04 7.72 29.44 4.31 5.69 8.86 16.67 7.34 3.76 12.50 33.33 6.61 12.07 13.64 36.36 13.76
NOTE. Data are from the Korean Nosocomial Infections Surveillance System, 2006-2009. SSI rates were calculated as the no. of SSIs per 100 surgeries. NNIS, National Nosocomial Infections Surveillance.
r
TABL E 2 . Univariat e Analysi s o f Ris k Factor s fo r Tota l Surgica l Sit e Infectio n (SSI ) afte r Tota l Hi p Arthroplast y an d afte r Tota l Kne e Arthroplast y Variabl e Hospital-relate d characteristic s Hospita l siz e > 90 0 bed s Mor e tha n 1 0 surgerie s performe d pe r mont h Operatin g roo m characteristic s HEPA-filtere d lamina r ai r flow HEPA-filtere d turbulen t ai r flow N o artificia l ventilatio n Intrinsic , patient-relate d (preoperative ) factor s Mal e se x Age , mea n year s ± SD * Preoperativ e hospita l sta y o f > 3 day s Bilatera l surger y Contaminate d o r dirt y woun d AS A scor e > 3 Diabete s mellitu s Obesit y (BM I > 25 ) Smokin g withi n 1 mont h Curren t systemi c steroi d therap y NNI S ris k inde x 0 1 2, 3 SS I (N = 161 ) 10 1 (63 ) 4 3 (27 ) 8 7 (54 ) 4 9 (30 ) 2 5 (16 ) 4 9 (30 ) 67. 6 ± 10. 3 8 0 (50 ) 16 (10 ) 10(6 ) 3 3 (21 ) 5 3 (33 ) 6 9 (43 ) 2 1 (13 ) 6(4 ) 6 9 (43 ) 7 2 (45 ) 2 0 (12 ) Al l arthroplastie s N o SS I (N = 6,687 ) 3,82 8 (57 ) 3,31 1 (50 ) 4,10 1 (61 ) 2,037 (30 ) 54 9 (8 ) 1,73 5 (26 ) 66. 9 ± 12. 7 2,16 4 (32 ) 55 9 (8 ) 75(1 ) 84 4 (13 ) 1,37 8 (21 ) 2,98 5 (45 ) 71 2 (11 ) 25 9 (4 ) 4,34 4 (65 ) 2,15 4 (32 ) 18 9 (3 ) Univariat e O R (95 % CI ) 1.2 6 (0.91-1.74 ) 0.3 7 (0.26-0.53 ) Referenc e 1.1 3 (0.80-1.62 ) 2.1 5 (1.36-3.38 ) 1.2 5 (0.89-1.76 ) 1.0 4 (0.91-1.17 ) 2.0 6 (1.51-2.82 ) 1.2 1 (0.72-2.04 ) 5.8 4 (2.96-11.52 ) 1.7 8 (1.21-2.64 ) 1.8 9 (1.35-2.64 ) 0.9 3 (0.68-1.28 ) 1.2 6 (0.79-2.00 ) 0.9 6 (0.42-2.20 ) Referenc e 2.1 0 (1.51-2.94 ) 6.6 6 (3.97-11.19 ) SS I (N = 78 ) 4 8 (62 ) 2 7 (35 ) 5 0 (64 ) 2 0 (26 ) 8(10 ) 2 6 (33 ) 67. 8 ± 11. 8 5 0 (64 ) K D 5(6 ) 2 2 (28 ) 2 9 (37 ) 1 9 (24 ) 1 5 (19 ) 4(5 ) 2 7 (35 ) 3 9 (50 ) 1 2 (15 ) Tota l hi p arthroplast y N o SS I (N = 3,344 ) 1,90 1 (57 ) 1,55 8 (47 ) 1,98 7 (59 ) 1,12 9 (34 ) 22 8 (7 ) 1,38 0 (41 ) 65. 2 ± 16. 2 1,27 9 (38 ) 55(2 ) 42(1 ) 62 4 (19 ) 61 0 (18 ) 86 4 (26 ) 57 2 (17 ) 16 1 (5 ) 1,99 0 (60 ) 1,24 7 (37 ) 10 7 (3 ) Univariat e O R (95 % CI ) 1.2 2 (0.77-1.93 ) 0.6 1 (0.38-0.97 ) Referenc e 0.7 0 (0.42-1.19 ) 1.3 9 (0.65-2.98 ) 0.7 1 (0.44-1.15 ) 1.1 0 (0.96-1.25 ) 2.8 8 (1.81^.60 ) 0.7 8 (0.11-5.69 ) 5.3 9 (2.07-14.01 ) 1.7 1 (1.04-2.83 ) 2.6 5 (1.66-4.23 ) 0.9 3 (0.55-1.56 ) 1.1 5 (0.65-2.04 ) 1.0 7 (0.39-2.96 ) Referenc e 2.3 1 (1.40-3.78 ) 8.2 7 (4.08-16.77 ) SS I (N = 83 ) 5 3 (64 ) 1 6 (19 ) 3 7 (45 ) 2 9 (35 ) 1 7 (20 ) 2 3 (28 ) 67. 4 ± 8. 8 3 0 (36 ) 1 5 (18 ) 5(6 ) 1 1 (B ) 2 4 (29 ) 5 0 (60 ) 6(7 ) 2(2 ) 4 2 (51 ) 3 3 (40 ) 8(10 ) Tota l kne e arthroplast y N o SS I (N = 3,343 ) 1,92 7 (58 ) 1,75 3 (52 ) 2,11 4 (63 ) 90 8 (27 ) 32 1 (10 ) 35 5 (11 ) 68. 6 ± 7. 5 88 5 (26 ) 50 4 (15 ) 33(1 ) 22 0 (7 ) 76 8 (23 ) 2,12 1 (63 ) 14 0 (4 ) 9 8 (3 ) 2,35 4 (70 ) 90 7 (27 ) 8 2 (2 ) Univariat e O R (95 % CI ) 1.3 0 (0.83-2.04 ) 0.2 2 (0.13-0.38 ) Referenc e 1.8 3 (1.12-2.99 ) 3.0 3 (1.68-5.44 ) 3.2 3 (1.97-5.28 ) 0.7 9 (0.53-1.06 ) 1.5 7 (1.00-2.48 ) 1.2 4 (0.71-2.19 ) 6.4 3 (2.45-16.91 ) 2.1 7 (1.13-4.15 ) 1.3 6 (0.84-2.21 ) 0.8 7 (0.56-1.36 ) 1.7 8 (0.76-4.16 ) 0.8 2 (0.20-3.37 ) Referenc e 2.0 4 (1.28-3.24 ) 5.4 7 (2.49-12.02 )Extrinsic , procedure-relate d (perioper -ative ) factor s Genera l anesthesi a Revisio n surger y Emergenc y surger y Duratio n o f surger y i n minutes , mea n ± SD b Duratio n o f surger y > 75t h percentil e Traum a Transfusio n o f packe d RB C Cemen t insertio n Non e Simpl e Antibioti c impregnate d Infection s a t othe r anatomica l site s AMP-relate d factors c Typ e o f antibioti c selecte d First-generatio n cephalospori n Glycopeptid e Other 1 1 Timin g o f administratio n o f firs t dos e Appropriat e timing 1 Duratio n o f AM P < 2 day s 8 1 (50 ) 3 4 (21 ) 6(4 ) 6 6 ± 9 4 7 0 (44 ) 4 1 (26 ) 9 5 (59 ) 6 9 (43 ) 4 6 (29 ) 4 6 (29 ) 1 6 (10 ) N = 12 7 6 3 (50 ) 3(2 ) 6 1 (48 ) 12 5 (98 ) 14(11 ) 2,49 5 (37 ) 52 9 (8 ) 12 7 (2 ) 12 9 ± 6 5 1,62 0 (24 ) 1,22 4 (18 ) 3,30 0 (49 ) 2,72 8 (41 ) 1,74 0 (26 ) 2,21 9 (33 ) 21 3 (3 ) N = 6,21 4 3,62 5 (58 ) 95(2 ) 2,49 4 (40 ) 5,96 5 (96 ) 1,21 6 (20 ) 1.7 0 (1.24-2.33 ) 3.1 2 (2.11-1.60 ) 2.0 0 (0.87-4.61 ) 1.0 3 (1.02-1.04 ) 2.4 1 (1.75-3.30 ) 1.5 3 (1.06-2.19 ) 1.4 8 (1.08-2.03 ) Referenc e 1.0 5 (0.72-1.53 ) 0.8 2 (0.56-1.20 ) 3.3 5 (1.97-5.72 ) Referenc e 1.9 1 (0.59-6.19 ) 1.4 1 (0.99-2.01 ) 2.6 1 (0.64-10.61 ) 0.5 1 (0.29-0.89 ) 4 2 (54 ) 2 2 (28 ) 5(6 ) 17 1 ± 10 1 3 7 (47 ) 3 8 (49 ) 5 4 (69 ) 6 0 (77 ) 9(12 ) 9(12 ) 1 0 (13 ) N = 5 7 2 4 (42 ) 0 33 (58 ) 5 5 (96 ) 1(2 ) 1,42 9 (43 ) 38 9 (12 ) 11 7 (4 ) 12 7 ± 6 7 79 9 (24 ) 1,17 1 (35 ) 1,98 8 (59 ) 2,53 0 (76 ) 33 4 (10 ) 48 0 (14 ) 14 9 (4 ) N = 3,03 0 1,66 0 (55 ) 10(0 ) 1,36 0 (45 ) 2,90 3 (96 ) 10 7 (4 ) 1.5 6 (1.00-2.45 ) 2.9 8 (1.80-4.94 ) 1.8 9 (0.75-4.76 ) 1.0 4 (1.02-1.05 ) 2.8 7 (1.83-4.52 ) 1.7 6 (1.12-2.76 ) 1.5 4 (0.94-2.50 ) Referenc e 1.1 4 (0.56-2.31 ) 0.7 9 (0.39-1.60 ) 3.1 5 (1.59-6.25 ) Referenc e 1.6 8 (0.99-2.85 ) 1.2 0 (0.29-1.99 ) 0.4 9 (0.07-3.56 ) 3 9 (47 ) 1 2 (15 ) K D 16 1 ± 8 7 3 3 (40 ) 3(4 ) 4 1 (49 ) 9(11 ) 3 7 (45 ) 3 7 (45 ) 6(7 ) N = 7 0 3 9 (56 ) 3(4 ) 2 8 (40 ) 7 0 (100 ) 1 3 (19 ) 1,06 6 (32 ) 14 0 (4 ) 10(0 ) 13 1 ± 6 2 82 1 (25 ) 53(2 ) 1,31 2 (39 ) 19 8 (6 ) 1,40 6 (42 ) 1,73 9 (52 ) 64(2 ) N = 3,18 4 1,96 5 (62 ) 85(3 ) 1,13 4 (36 ) 3,06 2 (96 ) 1,10 9 (35 ) 1.8 9 (1.22-2.93 ) 3.8 7 (2.06-7.30 ) 4.0 7 (0.51-32.12 ) 1.0 3 (1.02-1.04 ) 2.0 3 (1.30-3.17 ) 2.3 3 (0.71-7.61 ) 1.5 1 (0.98-2.34 ) Referenc e 0.5 8 (0.28-1.22 ) 0.4 7 (0.22-0.98 ) 3.9 9 (1.68-9.50 ) Referenc e 1.9 3 (0.58-6.38 ) 1.2 4 (0.76-2.03 ) 5.6 4 (0.35-91.59 ) 0.4 3 (0.23-0.78 ) NOTE . Dat a ar e fro m th e Korea n Nosocomia l Infection s Surveillanc e System , 2006-2009 . Dat a ar e no . (% ) o f cases , unles s otherwis e indicated . Bol d indicate s a statisticall y significan t odd s rati o (OR ) in univariat e analysi s (P < .10) . AMP , antimicrobia l prophylaxis ; ASA , America n Societ y o f Anesthesiologists ; BMI , bod y mas s index ; CI , confidenc e interval ; HEPA , high-efficienc y particulat e air ; NNIS , Nationa l Nosocomia l Infectio n Surveillance ; RBC , re d bloo d cells ; SD , standar d deviation . a Pe r 10-yea r increase . b Pe r 1-hou r increase . c A tota l o f 36 5 case s wer e exclude d (25 0 tota l hi p arthroplastie s an d 11 5 tota l kne e arthroplasties ) becaus e antibiotic s wer e use d t o trea t preoperativ e infections . A tota l o f 14 2 case s wer e als o exclude d (8 5 tota l hi p arthroplastie s an d 5 7 tota l kne e arthroplasties ) fro m th e analysi s o f AMP-relate d factor s becaus e o f missin g data . d Second-generatio n cephalosporin s wer e use d i n 1,88 3 case s (74%) , third-generatio n cephalosporin s wer e use d i n 49 4 (19%) , quinolone s wer e use d i n 9 1 (4%) , an d othe r antibiotic s wer e use d i n 8 7 (3%) . ' Define d a s parentera l antimicrobia l prophylaxi s initiate d withi n 1 hou r befor e incisio n fo r cephalosporin s o r withi n 2 hour s fo r vancomyci n o r fluoroquinolones .
1 0 9 0 I N F E C T I O N C O N T R O L AND H O S P I T A L E P I D E M I O L O G Y N O V E M B E R 2 0 1 2 , V O L . 3 3 , N O . 11
R E S U L T S
Characteristics of Surveillance
All 26 participating hospitals had 300 or more beds. Of these hospitals, 9 (35%) had 900 or more beds. Nine hospitals had operating rooms with HEPA-filtered laminar air flow (group 1), 12 had operating rooms with HEPA-filtered turbulent air flow (group 2), and 1 had operating rooms without artificial ventilation (group 3). Two hospitals had operating rooms in group 1 and group 2, 1 had operating rooms in group 1 and group 3, and the remaining hospital had operating rooms in group 2 and group 3.
The total duration of surveillance was 396 months. During that period, a total of 6,961 arthroplasties were performed. A total of 113 patients (1.6%) who did not complete the 1-year surveillance period were excluded. Thus, 6,848 patients who had undergone arthroplasty were enrolled in the study (representing 3,422 cases of THA from 26 hospitals and 3,426 cases of TKA from 25 hospitals). The majority of these pa-tients were followed up as scheduled; telephone contact was required with only 255 patients (3.7%).
Cases involving THA ranged from 11 to 824 in the par-ticipating hospitals; the average frequency of THA was 8.1 per month (median, 7.6; range, 1.8-27.5). Cases involving TKA ranged from 5 to 959 in the participating hospitals; the average frequency of TKA was 8.7 per month (median, 6.1; range, 0.8-32.0).
The mean age of the 6,848 patients was 67 years (median, 69; range, 15-107), and 1,784 (26%) of the patients were male. The 75th-percentile cutoff values for duration of sur-gery were 155 and 152 minutes for THA and TKA, respectively.
Rates and Characteristics of SSIs
SSI occurred in 161 cases (2.35%). All of these were diagnosed in person and not by telephone interview. When stratified by the NNIS risk index, rates of total SSI were 1.56 (69 of 4,413), 3.23 (72 of 2,226), and 9.57 (20 of 209) for risk categories 0, 1, and 2-3, respectively. For THA and TKA, rates of total SSI were 2.28 (95% confidence interval [CI], 1.83-2.84) and 2.42 (95% CI, 1.93-2.99), respectively. There was no differ-ence in rates of overall SSI between patients who underwent THA and patients who underwent TKA (P = .696). The rate of severe SSI after THA was 1.61 (95% CI, 1.23-2.09), and after TKA it was 1.87 (95% CI, 1.46-2.38). Pooled means and key percentiles of the rates of total SSI according to arthroplasty site are listed in Table 1.
Of the 161 SSIs, 42 (26%) were classified as superficial-incisional SSIs, 24 (15%) were deep-superficial-incisional SSIs, and 95 (59%) were organ/space SSIs. Severe SSI accounted for 74% (119 cases) of total SSI. For SSIs that occurred after THA, 23 (30%) were superficial-incisional SSI, 11 (14%) were deep-incisional SSI, and 44 (56%) were organ/space SSI. For SSIs that occurred after TKA, 19 (23%) were superficial-incisional
SSIs, 13 (16%) were deep-incisional SSIs, and 51 (61%) were organ/space SSIs.
Most cases of total (146; 91%) and severe SSI (105; 88%) were early-onset infections (developing within 3 months after surgery). Median time between surgery and SSI diagnosis was 15 days (interquartile range [IQR], 10-29 days). Median time between surgery and diagnosis for SSI after THA (median interval, 15 days; IQR, 10-24 days) did not differ from that for SSI after TKA (median interval, 15 days; IQR, 10-35 days). The pathogen responsible for the SSI was identified in 93 (58%) of the 161 cases. Pathogen identification was more successful for SSI after THA (54/78; 69%) than for SSI after TKA (39/83; 47%; P = .004). Gram-positive cocci such as coagulase-negative staphylococci (44/93; 47%) and
Staphy-lococcus aureus (25/93; 27%) were most frequent, and in 84%
(58/69) of these cases the staphylococci were methicillin re-sistant. Gram-negative rods were more frequent in SSI after THA (9/54; 17%) than in SSI after TKA (3/39; 8%), although the difference was not statistically significant.
Risk Factors Associated with SSI
The results of univariate analysis of risk factors for total SSI after arthroplasty are presented in Table 2. Significant risk factors for total and severe SSI identified by multivariate anal-ysis are listed by the arthroplasty site in Table 3.
Multivariate analysis of total SSIs (Table 3) showed that the significant risk factors were different according to the site of arthroplasty. For THA, these factors were diabetes mellitus, revision surgery, prolonged duration of surgery, and trauma. For TKA, on the other hand, a larger volume of surgeries (>10 per month) decreased the risk of total SSI, whereas male sex and operating rooms without artificial ventilation (com-pared with those that had HEPA-filtered laminar air flow) increased the risk of total SSI. A long duration of preoperative hospital stay (>3 days) was an independent risk factor for both arthroplasty sites.
In univariate analysis, type of antibiotic and duration of AMP were associated with total SSI (P < .10). However, when AMP-related factors were included in the multivariate anal-ysis, they were not revealed to be independent risk factors for total SSI at either arthroplasty site. In addition, after in-cluding AMP-related factors in the multivariate analysis, pro-longed duration of surgery was revealed to be a risk factor for SSI after TKA (odds ratio [OR], 1.89; 95% CI, 1.08-3.31), and revision surgery lost its significance as a risk factor for total SSI after THA.
Multivariate analysis for severe SSI (Table 3) produced sim-ilar results to that for total SSI, except that presence of in-fections at other anatomical sites was a significant risk factor and surgery under general anesthesia was not significant for either site. For THA, significant risk factors for severe and total SSI were identical. However, for TKA, although a large volume of surgery, male sex, and ORs without artificial ven-tilation were independent protective or risk factors for severe
D I F F E R E N T RISK FACTORS FOR SSI B E T W E E N THA AND TKA 1 0 9 1
SSI and total SSI, a long duration of preoperative hospital stay (>3 days) was not a risk factor for severe SSI. Because AMP-related factors were not statistically significant for severe SSI in the univariate analysis, these factors were not consid-ered in the multivariate analysis.
DISCUSSION
In this study, we found that significant risk factors for total and severe SSI differed between THA and TKA. Longer du-ration (>3 days) of preoperative hospital stay was the only risk factor for total SSI that was independent of the site of arthroplasty. Diabetes mellitus, revision surgery, prolonged duration of surgery (>75th percentile), and trauma as the reason for surgery were independent risk factors for total and severe SSI after THA, whereas male sex and an operating room without artificial ventilation were independent risk fac-tors for total and severe SSI after TKA. A large volume of surgery (>I0 procedures per month) protected against total and severe SSI, but only for TKA. This finding is consistent with a recent report suggesting that the risk factors for pros-thetic joint infection differ according to the joint being re-placed.6 Therefore, grouping all joint replacements in analysis may miss some relevant risk factors.6 In fact, in our study, although sex difference was associated with total and severe SSI after TKA, this association was not evident in multivariate analysis for all arthroplasties. In addition, surgery because of trauma was not an independent risk factor for severe SSI for all arthroplasties, but this factor was revealed to be associated with an increased risk of total and severe SSI after THA.
In this study, there were 365 cases in which antibiotics were used to treat active infection before surgery. A significant
number of cases (142) were missing data about AMP. Na-tionally, the majority (>80%) of patients receive AMP for more than 2 days, and in a large proportion (~40%) of cases, antibiotics other than first-generation cephalosporins and gly-copeptides are used after AMP. Hence, in Table 3 we present the results of a multivariate analysis in which AMP-related factors were excluded. When these factors were included, re-vision surgery was no longer a risk factor for SSI after either THA or TKA, and prolonged duration of surgery became a risk factor for SSI after both THA and TKA. Administration of AMP for more than 2 days was more common in patients undergoing revision surgery (441/476; 93%) than in those undergoing primary arthroplasty (4,670/5,865; 80%; P = .000). Revision surgery is a well-known risk factor for SSI; for this reason, AMP may have been used for longer durations in cases of revision surgery, which may have reduced the effect of revision surgery on the development of SSI. The reason for the significance of prolonged duration of surgery when AMP-related factors are included in the analysis is unclear, but the exclusion of cases of therapeutic AMP administration may reveal the effect of prolonged duration of surgery on the development of SSI.
Longer duration of preoperative hospital stay and longer duration of surgery are well-known risk factors for SSI in general, as our findings suggest.3'17 It is likely that trauma as a reason for surgery was only an independent risk factor for THA because trauma was the reason for arthroplasty in only 2% of cases of TKA (56/3,416), whereas it was 35% (1,209/ 3,422) in cases of THA. Diabetes mellitus and revision surgery are widely acknowledged risk factors for SSI after arthro-plasty.318 However, why we found those factors to be inde-TABLE 3. Significant Risk Factors for Total and Severe Surgical Site Infection (SSI) after Total Hip Arthroplasty and after Total Knee Arthroplasty Identified by Multivariate Analysis
Variable
Hospital-related characteristics
More than 10 surgeries performed per month
Operating room characteristics HEPA-filtered laminar air flow HEPA-filtered turbulent air flow Without artificial ventilation Intrinsic, patient-related (preoperative)
factors Male sex
Preoperative hospital stay > 3 days Diabetes mellitus
Extrinsic, procedure-related (perioperative) factors
General anesthesia Revision surgery
Duration of surgery > 75th percentile Trauma
Infections at other anatomical sites
All arthroplasties Total SSI 0.44 (0.30-0.65) Reference NS 2.07 (1.27-3.38) NI 1.68 (1.19-2.36) 1.56 (1.10-2.21) 1.48 (1.06-2.06) 2.03 (1.29-3.21) 1.99 (1.38-2.86) NS NS Severe SSI 0.36 (0.22-0,57) Reference NS 2.15 (1.21-3.84) NI 1.59 (1.06-2.37) 1.73 (1.16-2.58) NS 2.87 (1.76-4.70) 1.97 (1.29-3.02) NS 2.03 (1.09-3.77)
Total hip arthroplasty Total SSI NS NI NI NI 2.23 (1.33-3.74) 1.97 (1.20-3.22) NS 2.34 (1.26-4.35) 2.45 (1.47-4.10) 1.77 (1.07-2.93) NS Severe SSI NS NI NI NI 2.18 (1.17-4.09) 2.35 (1.32-4.19) NS 3.60 (1.78-7.28) 2.49 (1.35-4.59) 2.12 (1.15-3.90) NS Total knee Total SSI 0.24 (0.12-0.46) Reference NS 2.82 (1.45-5.49) 2.84 (1.71-4.74) 1.66 (1.02-2.72) NI NS NS NS NI NS arthroplasty Severe SSI 0.14 (0.06-0.33) Reference NS 2.81 (1.30-6.07) 3.14 (1.71-5.77) NS NI NS NS NS NI NS NOTE. Data are from the Korean Nosocomial Infections Surveillance System, 2006-2009. Data are odds ratio (95% confidence interval). Deep-incisional and organ/space SSIs are considered to be "severe" SSIs. HEPA, high-efficiency particulate air; NI, not included in the multivariate analysis; NS, not significant.
1 0 9 2 I N F E C T I O N C O N T R O L AND H O S P I T A L E P I D E M I O L O G Y N O V E M B E R 2 0 1 2 , V O L . 3 3 , N O . 11
pendent risk factors for SSI only following THA, and not TKA, is unclear. In our study, the proportion of cases with an ASA score of 3 or more was higher for THA (19%) than for TKA (7%; P = .000; Table 2). Because ASA score rep-resents the severity of preexisting illness, diabetes mellitus and revision surgery may have a greater impact on the de-velopment of SSI in patients with severe preexisting illness than in patients with mild illness.17
Similar to the findings of Meyer et al,19 in our study a large volume of surgery (>10 procedures per month) was an in-dependent protective factor for SSI among patients under-going TKA. Katz et al20 observed a similar trend in patients undergoing THA, and our univariate analysis of THA re-vealed a large volume of surgery to be associated with reduced risk of total SSI (OR, 0.61; 95% CI, 0.38-0.97; Table 2). Thus, a low volume of surgery appears to be an independent risk factor for SSI, regardless of the arthroplasty site. However, a multivariate analysis of cases of THA suggests that the impact of the volume of surgery on the development of SSI may differ, depending on the arthroplasty site. The reasons un-derlying the association between volume of surgery and SSI are probably multifactorial and related both to hospital char-acteristics and to the experience of surgical teams as a whole (and not just the skill of the surgeons).
Recently, Brandt et al7 reported that ventilation with lam-inar airflow was not beneficial and was even associated with a higher risk of severe SSI after hip prosthesis surgery. In our study, presence in the operating room of laminar air flow compared with turbulent air flow was not associated with SSI, irrespective of arthroplasty site. However, for TKA, mul-tivariate analysis revealed that an operating room without artificial ventilation compared with an one that had HEPA-filtered laminar air flow was associated with increased risk of total SSI (OR, 2.82; 95% CI, 1.45-5.49; Table 3). This as-sociation was also significant in the multivariate analysis for severe SSI (OR, 2.81; 95% CI, 1.30-6.07; Table 3). Improper positioning of operating room personnel, uncontrolled (or unidentified) traffic control, and vertical airflow that, for ex-ample, induces lower local temperatures could all be reasons for the limited effect of ventilation system on reducing SSI. However, the exact reasons for this are unclear, as is the reason for the difference observed between arthroplasty sites. Further studies of these matters are needed, especially in relation to cost effectiveness.
In this study, we used the CDC criteria to diagnose and classify SSIs. However, a major concern of clinicians in terms of infection is the development of periprosthetic joint infec-tion (PJI) in patients who undergo arthroplasty.21,22 Thus, inclusion of PJI in the diagnosis and classification of SSI seems to be more appropriate than using the CDC definition of SSI for analyzing the risk factors for infection. However, the use of the CDC criteria is traditional, and they remain the most widely used and simplest definitions, even for prosthetic joint replacement.13,23 To reduce the limitations of the CDC criteria, we used 2 categories of SSI in the outcome assessment and
space SSI) and total SSI. Whereas detection bias associated with superficial-incisional SSI is widely acknowledged, severe SSI is difficult to miss, since it is usually serious and requires rehospitalization, return to surgery, and intravenous antibi-otic therapy.24 Superficial-incisional SSI may be one of the most important risk factors for PJI.21 Although we could not evaluate its impact on PJI in this study, we believe that severe SSI partially reflects PJI.
The strengths of this study include the fact that we eval-uated a large, nationwide surgical patient population over a 4-year period, using the same case-recording and detection-surveillance system, for THA and TKA. However, our study has several limitations. First, the results may be affected by selection bias, as we did not gather data from smaller (<300-bed) hospitals. TKA in particular is frequently performed in smaller hospitals. However, we did collect data from ap-proximately 10% of all hospitals in Korea with 300 or more beds, and these were distributed throughout the country. Therefore, we believe that the results of this study are at least partially representative of the national situation in Korea. Second, because our study was based on a national noso-comial infection surveillance system, we could not include all potential risk factors for SSI, such as the type of antiseptic agent used, presence of bacterial colonization, the difficulty of the procedure, the surgical technique used, traffic control, environmental surfaces, temperature control, postoperative hyperglycemia, wound problems other than infection, and so forth. Third, as mentioned above, inappropriate selection and duration of AMP were prevalent in the cases we examined. After implementing measurement of the clinical performance of AMP in 2007 as a part of the national hospital evaluation program, appropriate use of AMP at last improved perfor-mance in Korea.25 Thus, the effect of AMP-related factors should be taken into account when analyzing our data, al-though there was no significant relationship between AMP-related factors and SSI in multivariate analysis. Finally, there is a possibility that patients with delayed-onset SSI (>12 months) were missed, because we did not perform patient follow-up for long enough to identify these cases.
In summary, some risk factors for SSI such as prolonged duration of preoperative hospital stay and prolonged duration of surgery (when AMP-related factors are included in the analysis) were independent of the site of arthroplasty. How-ever, other important risk factors for SSI differed according to the arthroplasty site. Therefore, clinicians should consider the arthroplasty site in analyses of SSI and the development of strategies to reduce it.
A C K N O W L E D G M E N T S
We thank the participants in the Korean Nosocomial Infections Surveillance System (KONIS) and their associated staff for their cooperation in this study. The hospitals participating in KONIS were as follows (in alphabetical order): Ajou University Hospital, Bundang CHA Medical Center, Chonbuk National
D I F F E R E N T RISK FACTORS FOR SSI B E T W E E N THA AND TKA 1093
Mokdong Hospital, Gachon University Gil Hospital, Gangnam Severance Hospital, Hanil General Hospital, Hanyang University Medical Center, Inha University Hospital, Inje University Ilsan Paik Hospital, Inje University Sang-gye Paik Hospital, Keimyung University Dongsan Medical Center, Konyang University Hospital, Korea University Anam Hospital, Kwangju Christian Hospital, Kyungpook National University Hospital, Seoul National University Bundang Hospital, Severance Hospital, SMG-SNU Boramae Medical Center, Soon Chun Hyang University Hospital Bucheon, Soon Chun Hyang Uni-versity Hospital Cheonan, Soon Chun Hyang UniUni-versity Hospital Seoul, and Wonju Christian Hospital. This study was approved by the institutional re-view board of Seoul National University Bundang Hospital.
Financial support. The Korean Nosocomial Infections Surveillance
Sys-tem was supported by a grant from the Korea Centers for Disease Control and Prevention.
Potential conflicts of interest. All authors report no potential conflicts of
interest relevant to this article. All authors submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest, and the conflicts that the editors consider relevant to this article are disclosed here.
Address correspondence to Hong Bin Kim, MD, Department of Internal Medicine, Seoul National University Bundang Hospital, 166 Gumi-ro, Bun-dang-gu, Seongnam, Republic of Korea, 463-707 (hbkimmd@snu.ac.kr).
Presented in part: 51st annual meeting of the Interscience Conference on Antimicrobial Agents and Chemotherapy; Chicago, Illinois; 2011 (Pre-sentation No. K-1567).
R E F E R E N C E S
1. Statistics on major surgical procedures in Korea, 2009. National Health Insurance Corporation website, http://www.nhic.or.kr. Accessed December 8, 2011.
2. Zimmerii W, Trampuz A, Ochsner PE. Prosthetic-joint infec-tions. N Engl J Med 2004;351(16):1645-1654.
3. Matthews PC, Berendt AR, McNally MA, Byren I. Diagnosis and management of prosthetic joint infection. BM/2009;338:bl773. 4. Steckelberg JM, Osmon DR. Prosthetic joint infections. In:
Waldvogel FA, Bisno AL, eds. Infections Associated with
Indwell-ing Medical Devices. 3rd ed. WashIndwell-ington, DC: ASM, 2000:
173-209.
5. Gaynes RP. Surveillance of nosocomial infections: a fundamental ingredient for quality. Infect Control Hosp Epidemiol 1997;18(7): 475-478.
6. Peel TN, Dowsey MM, Daffy JR, et al. Risk factors for prosthetic hip and knee infections according to arthroplasty site. / Hosp
Infect 2011;79(2):129-133.
7. Brandt C, Hott U, Sohr D, et al. Operating room ventilation with laminar airflow shows no protective effect on the surgical site infection rate in orthopedic and abdominal surgery. Ann
Surg 2008;248(5):695-700.
8. Kwak YG, Lee SO, Kim HY, et al. Risk factors for device-associated infection related to organisational characteristics of intensive care units: findings from the Korean Nosocomial In-fections Surveillance System. } Hosp Infect 2010;75(3):195-199. 9. Choi HJ. Multicenter surgical site infection surveillance study about prosthetic joint replacement surgery in 2006. Korean J
Nosocom Infect Control 2008;13(1):42-50.
10. Kim ES, Kim HB, Song KH, et al. Prospective nationwide sur-veillance of surgical site infections after gastric surgery and risk
factor analysis in the Korean Nosocomial Infections Surveillance System (KONIS). Infect Control Hosp Epidemiol 2012;33(6): 572-580.
11. Horan TC, Gaynes RP, Martone WJ, et al. CDC definitions of nosocomial surgical site infections, 1992: a modification of CDC definitions of surgical wound infections. Am } Infect Control 1992;20(5):271-274.
12. Song KH, Kang YM, Sin HY, et al. Outcome of cefazolin pro-phylaxis for total knee arthroplasty at an institution with high prevalence of methicillin-resistant Staphylococcus aureus infec-tion. Int J Infect Dis 2011;15(12):e867-e870.
13. Breier AC, Brandt C, Sohr D, et al. Laminar airflow ceiling size: no impact on infection rates following hip and knee prosthesis.
Infect Control Hosp Epidemiol 2011;32(11):1097-1102.
14. Altemeier WA. Manual on Control of Infection in Surgical
Pa-tients. 2nd ed. Philadelphia: Lippincott, 1984.
15. Owens W D , Felts JA, Spitznagel EL Jr. ASA physical status clas-sifications: a study of consistency of ratings. Anesthesiology 1978; 49(4):239-243.
16. Steinberg JP, Braun BI, Hellinger WC, et al. Timing of anti-microbial prophylaxis and the risk of surgical site infections: results from the Trial to Reduce Antimicrobial Prophylaxis Er-rors. Ann Surg 2009;250(1):10-16.
17. Urquhart DM, Hanna FS, Brennan SL, et al. Incidence and risk factors for deep surgical site infection after primary total hip arthroplasty: a systematic review. / Arthroplast 2010;25(8): 1216-1222, e l - e 3 .
18. Ridgeway S, Wilson J, Charlet A, et al. Infection of the surgical site after arthroplasty of the hip. } Bone Joint Surg 5r2005;87(6): 844-850.
19. Meyer E, Weitzel-Kage D, Sohr D, Gastmeier P. Impact of de-partment volume on surgical site infections following arthros-copy, knee replacement or hip replacement. BMJ Qua! Saf 2011; 20(12):1069-1074.
20. Katz JN, Losina E, Barrett J, et al. Association between hospital and surgeon procedure volume and outcomes of total hip re-placement in the United States medicare population. J Bone Joint
Surg Am 2001;83-A(11):1622-1629.
21. Berbari EF, Hanssen AD, Duffy MC, et al. Risk factors for pros-thetic joint infection: case-control study. Clin Infect Dis 1998; 27(5):1247-1254.
22. Laffer RR, Graber P, Ochsner PE, Zimmerii W. Outcome of prosthetic knee-associated infection: evaluation of 40 consecu-tive episodes at a single centre. Clin Microbiol Infect 2006;12(5): 4 3 3 ^ 3 9 .
23. Leekha S, Sampathkumar P, Berry DJ, Thompson RL. Should national standards for reporting surgical site infections distin-guish between primary and revision orthopedic surgeries? Infect
Control Hosp Epidemiol 2011;31(5):503-508.
24. Petrosillo N, Drapeau CM, Nicastri E, et al. Surgical site infec-tions in Italian hospitals: a prospective multicenter study. BMC
Infect Dis 2008;8:34.
25. Kim ES, Park SW, Lee CS, et al. Impact of a national hospital evaluation program using clinical performance indicators on the use of surgical antibiotic prophylaxis in Korea. Int J Infect Dis 2012;16(3):el87-el92.