INTRODUCTION
Motor neuron diseases (MNDs) are rare neurologi-cal disorders caused by selective degeneration of motor neurons that manifest as progressive weakness of various muscles. MNDs are classified according to area affected by degeneration: upper motor neurons (UMNs), lower motor neurons (LMNs), or both. Loss of UMNs results in slowness of movement, incoordination, hyperreflexia,
and spasticity. Consequences of LMN degeneration in-clude weakness, usually accompanied by atrophy and fasciculation, caused by loss of LMNs in the brainstem and spinal cord [1,2].
The initial signs and symptoms of MNDs vary depend-ing on the patient, but typical symptoms include motor weakness and a combination of wasting of muscles, dys-phagia, and dyspnea. Most patients with MNDs display respiratory failure; however, it is extremely rare to find
Annals of Rehabilitation Medicine
Case Report
Ann Rehabil Med 2017;41(2):328-331 pISSN: 2234-0645 • eISSN: 2234-0653 https://doi.org/10.5535/arm.2017.41.2.328
Motor Neuron Disease Presenting With Acute
Respiratory Failure: A Case Study
Hyeonjun Oh, MD1,2, Seong Woong Kang, MD, PhD1,2, Won Ah Choi, MD, PhD1,2,
Jang Woo Lee, MD3, Miri Suh, MD1,2, Eun Young Kim, MD1,2
1
Department of Rehabilitation Medicine, Gangnam Severance Hospital, Seoul; 2
Rehabilitation Institute of Neuromuscular Disease, Yonsei University College of Medicine, Seoul; 3
Department of Rehabilitation Medicine, Chuncheon Sacred Heart Hospital, Hallym University College of Medicine, Chuncheon, Korea
Motor neuron diseases (MNDs) refer to a heterogeneous group of progressive neurologic disorders caused by degeneration of motor neurons. The diseases affect either the upper motor neurons, lower motor neurons, or both, and are characterized by weakness, atrophy, fasciculation, spasticity, and respiratory failure. We report a case of a 61-year-old male patient with no past history of cardiovascular or pulmonary disease, who presented with only dyspnea, and no indication of any other symptom such as muscle weakness, atrophy, or bulbar dysfunction. Neuromuscular conduction study, including a study of the phrenic nerve, confirmed the diagnosis of MND. The patient greatly improved giving respiratory assistance at night, using a noninvasive ventilator. This case indicates that MNDs should be considered as differential diagnoses for patients showing acute respiratory failure of unknown causes. This report will aid in the prompt diagnosis and treatment of MNDs.
Keywords Motor neuron disease, Respiratory insufficiency, Mechanical ventilation
Received May 2, 2016; Accepted June 24, 2016 Corresponding author: Eun Young Kim
Department of Rehabilitation Medicine, Gangnam Severance Hospital, 211 Eonju-ro, Gangnam-gu, Seoul 06273, Korea. Tel: +82-2-2019-3490, Fax: +82-2-3463-7585, E-mail: elope86@yuhs.ac
ORCID: Hyeonjun Oh (http://orcid.org/0000-0002-4464-9915); Seong Woong Kang (http://orcid.org/0000-0002-7279-3893); Won Ah Choi (http:// orcid.org/0000-0003-0403-8869); Jang Woo Lee (http://orcid.org/0000-0002-2634-0375); Miri Suh (http://orcid.org/0000-0003-1759-9198); Eun Young Kim (http://orcid.org/0000-0001-6622-219X).
This is an open-access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/ licenses/by-nc/4.0) which permits unrestricted noncommercial use, distribution, and reproduction in any medium, provided the original work is properly cited. Copyright © 2017 by Korean Academy of Rehabilitation Medicine
Motor Neuron Disease Presenting With Acute Respiratory Failure
329
www.e-arm.org
any patient who presents with only respiratory dysfunc-tion as the initial symptom [3-6]. Here, we report the case of a patient with MND who had dyspnea as the initial symptom, with no weakening of the muscles or muscular atrophy, which ruled out disuse-induced deconditioning.
CASE REPORT
In February 2014, a 61-year-old male with no medical history except for hypertension, showed signs of exer-tional dyspnea. On worsening of his cough and dyspnea, the patient visited the hospital, where he was treated for his symptoms. In December 2014, aggravation of dys-pnea, general weakness, and mild dizziness, in his being admitted to an emergency department, at which point carbon dioxide (CO2) narcosis was observed. Arterial
blood gas analysis showed a pH of 7.350, a pCO2 of 63.7
mmHg, and a pO2 of 257.9 mmHg. After intubation, he
was transferred to the intensive care unit and placed on a ventilator. Tracheostomy was done in January 2015. A chest X-ray and echocardiogram examination showed no evidence of cardiopulmonary problems. Brain magnetic resonance imaging study, nerve conduction study, and needle electromyography (including the lower cervical, thoracic and lumbar paraspinal muscles as well as bilat-eral upper and lower extremities) also revealed no abnor-malities.
After 24 hours on the ventilator, the general condition of the patient improved; his dyspnea and CO2 narcosis
were ameliorated. In May 2015, he was transferred to our hospital for additional investigations to identify the cause of his symptoms, as well as for comprehensive rehabilitation including pulmonary rehabilitation. Mo-tor examination did not reveal any significant weakness, nor was there any indication of muscle atrophy. Sensory functions were intact in all extremities. On functional level evaluation, the patient was only able to sit, due to his dependence on the 24-hour mechanical ventilation via tracheostomy tube, and his muscles being in a state of disuse. Initial laboratory study revealed no
abnormali-ties. Arterial blood gas analysis was also within the nor-mal range with use of the ventilator.
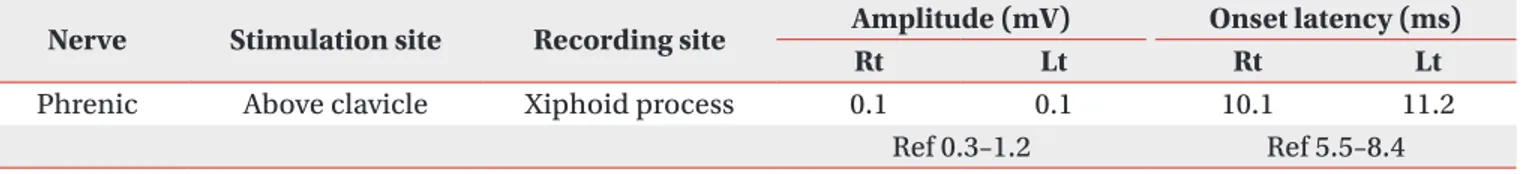
Even though physical examination showed nothing ex-cept muscle deconditioning, other examinations revealed prominent diaphragm. Pulmonary function test recorded his vital capacity at 420 mL (11.8% of the predicted value) when sitting, and 350 mL (9.8% of the predicted value) while in a supine position, as measured with a trache-ostomy tube. His peak cough flow was too low to be checked. When given a diaphragmatic movement evalu-ation through fluoroscopy, a 0.25 cm diaphragm move-ment was present on both sides while the patient was at rest, and there was no difference in maximal breathing from resting status. Also, an additional nerve conduc-tion study done on the bilateral phrenic nerves to check phrenic nerve-diaphragm function showed a prolonged latency and low amplitude of compound motor action potentials (Table 1). Needle electromyography on both sides of the diaphragm showed abnormal spontaneous activity and a partial interference pattern on full inspira-tion. Follow-up nerve conduction studies and needle electromyography revealed a widespread active neuro-genic process in the brain stem, and the cervical, tho-racic, and lumbar segments of the spinal cord.
Although his initial symptom was simple respiratory muscle weakness, the patient was diagnosed with MND. A genetic study was conducted to ensure an accurate di-agnosis. However, nothing unusual was found, such as superoxide dismutase 1 (SOD1) mutation, a spinal and bulbar muscular atrophy (SBMA) triplet repeat, or a sur-vival motor neuron 1 (SMN1) gene mutation.
Although speech evaluation showed a mild degree of dysarthria, his articulation was nearly perfect; he scored a 93.0% in phonation accuracy. Mild penetration without definite laryngeal aspiration, evaluated with small and large liquid, was observed on videofluoroscopic swallow-ing studies, thus concludswallow-ing that the patient did not have bulbar muscle dysfunction.
The non-fenestrated cuffed tracheostomy tube was changed to a fenestrated cuffless tracheostomy tube, and
Table 1. Results of the nerve conduction studies
Nerve Stimulation site Recording site Amplitude (mV) Onset latency (ms)
Rt Lt Rt Lt
Phrenic Above clavicle Xiphoid process 0.1 0.1 10.1 11.2
Hyeonjun Oh, et al.
330
www.e-arm.orgnoninvasive ventilation training through a nasal mask was conducted. There were no complaints of dyspnea or dizziness, and CO2 monitoring showed no retention
(Table 2). Therefore, a decannulation was conducted on April 13, 2015, as the patient was able to tolerate trache-ostomy tube capping and noninvasive ventilation. The patient no longer required ventilation during the day-time, but noninvasive ventilation was continued at night to alleviate nocturnal respiratory problems.
Discontinuation of ventilator during daytime, along with comprehensive pulmonary rehabilitation, contrib-uted to recovery in general and respiratory functions. Upon discharge, the patient had recovered extensively, performing nearly independent activities of daily living such as hand writing, using chopsticks and walking with minimal assistance. A follow-up fluoroscopy revealed a slight improvement, as the patient’s diaphragm move-ment was about 1 cm on both sides at rest, and 1.5 cm at both sides on maximal breathing; however, the dia-phragm weakness persisted and continued to cause noc-turnal hypercapnia, and hence respiratory assistance was continued by noninvasive ventilation at night.
DISCUSSION
Although dyspnea is a result of severe respiratory mus-cle weakness, and is an advanced-stage complication of MNDs and major cause of fatality, it is seldom an initial symptom. Very rarely does a patient require mechanical ventilation due to acute respiratory failure before being diagnosed with MND. Respiratory failure for amyotrophic lateral sclerosis (ALS), the most common type of MND, is also a late complication. However, with adequate
as-sistance for breathing using noninvasive ventilation, patients with respiratory onset ALS may not show a rapid progressive course [7]. Broadly, this could be similar in MNDs with respiratory onset.
Due to bilateral phrenic failure, most patients present with dyspnea, orthopnea, and hypercapnia [3-6], and it is extremely uncommon for the neurological examination to reveal any other conditions [6,8]. There have been no reports in Korean patients presenting with dyspnea in the absence of other characteristic symptoms of MND, such as limb weakness, muscle atrophy, dysarthria, or dyspha-gia.
Most physicians will not consider a diagnosis of MND until its characteristic clinical features are evident. Many patients experience respiratory failure in conjunction with increased muscle tension, muscle weakness, mus-cular atrophy, and fasciculation, and cases involving only acute respiratory failure are extremely rare [8]. Our patient had no muscular atrophy or bulbar dysfunction, and the results of an initial neuromuscular conductivity test were normal; he only had a prior history of requiring a ventilator to treat dyspnea, orthopnea, and hypercap-nia, making it difficult to diagnose MND.
In a previous case, a Korean patient diagnosed with MND was applied to mechanical ventilation through a tracheostomy site [9]. However, there are many disadvan-tages of tracheostomy, including limitation in swallowing and conversation, and consequently a low quality of life. Therefore, if necessary, mechanical ventilation by nonin-vasive method should be considered.
In conclusion, in the absence of limb or bulbar involve-ment, when diaphragmatic weakness appears as the initial symptom in patients with acute respiratory failure
Table 2. Overnight continuous monitoring data from the transcutaneous blood gas monitoring device
HD 1 HD 4 HD 12 HD 20 HD 24 HD 26 HD 30 Average SpO2 (%) 100 99 98 100 95 96 95 pO2 range (%) 96–100 100 100 99 100 36 71 69 90–95 0 0 0 0 58 29 31 Max CO2 (%) 37.8 35.0 35.2 40.6 42.4 43.8 44.6 Mean CO2 (%) 32.6 30.2 27.1 33.9 35.2 36.7 38.7 Route of ventilation T T T M M M M Etc. O2 2 L - - - Decannulation -
-HD, hospital days; SpO2, saturation of partial pressure of oxygen; pO2, partial pressure of oxygen; T, tracheostomy
Motor Neuron Disease Presenting With Acute Respiratory Failure
331
www.e-arm.org
of unknown cause, MNDs should be considered and be investigated with a neuromuscular conductivity test that includes assessment of the phrenic nerve. Patients thus diagnosed will exhibit notable improvement after being given appropriate respiratory assistance.
CONFLICT OF INTEREST
No potential conflict of interest relevant to this article was reported.
REFERENCES
1. Francis K, Bach JR, DeLisa JA. Evaluation and reha-bilitation of patients with adult motor neuron disease. Arch Phys Med Rehabil 1999;80:951-63.
2. Norris F, Shepherd R, Denys E, U K, Mukai E, Elias L, et al. Onset, natural history and outcome in idiopathic adult motor neuron disease. J Neurol Sci 1993;118:48-55.
3. Similowski T, Attali V, Bensimon G, Salachas F, Mehiri S, Arnulf I, et al. Diaphragmatic dysfunction and dys-pnoea in amyotrophic lateral sclerosis. Eur Respir J
2000;15:332-7.
4. Czaplinski A, Strobel W, Gobbi C, Steck AJ, Fuhr P, Leppert D. Respiratory failure due to bilateral dia-phragm palsy as an early manifestation of ALS. Med Sci Monit 2003;9:CS34-6.
5. Chen R, Grand’Maison F, Strong MJ, Ramsay DA, Bolton CF. Motor neuron disease presenting as acute respiratory failure: a clinical and pathological study. J Neurol Neurosurg Psychiatry 1996;60:455-8.
6. Al-Shaikh B, Kinnear W, Higenbottam TW, Smith HS, Shneerson JM, Wilkinson I. Motor neurone disease presenting as respiratory failure. Br Med J (Clin Res Ed) 1986;292:1325-6.
7. Shoesmith CL, Findlater K, Rowe A, Strong MJ. Prog-nosis of amyotrophic lateral sclerosis with respiratory onset. J Neurol Neurosurg Psychiatry 2007;78:629-31. 8. de Carvalho M, Matias T, Coelho F, Evangelista T,
Pin-to A, Luis ML. MoPin-tor neuron disease presenting with respiratory failure. J Neurol Sci 1996;139 Suppl:117-22. 9. Park HS. A case of motor neuron disease presenting as
dyspnea in the emergency department. Korean J Fam Med 2012;33:110-3.