Clinical Pediatric Hematology-Oncology
Volume 23ㆍNumber 1ㆍApril 2016 CASE REPORT57
침습성 진균감염이 있는 중증재생불량빈혈 환자의 동종조혈모세포이식 1예
서유리ㆍ김혜리ㆍ고경남ㆍ임호준ㆍ서종진
울산대학교 의과대학 소아과학교실
Successful Allogeneic Hematopoietic Stem Cell Transplantation for a Patient with Very Severe Aplastic Anemia During Active Invasive Fungal Infection
Euri Seo, M.D., Hyeri Kim, M.D., Ph.D., Kyung-Nam Koh, M.D., Ph.D., Ho Joon Im, M.D., Ph.D. and Jong Jin Seo, M.D., Ph.D.
Department of Pediatrics, Asan Medical Center Children’s Hospital, University of Ulsan College of Medicine, Seoul, Korea
Allogeneic hematopoietic stem cell transplantation (HSCT) may not be considered fea- sible in a patient with active fungal infection due to transplant-related mortality. We re- port a case of HSCT performed on a 6-month-old girl, who was diagnosed with very severe aplastic anemia (vSAA) at the age of 2 months, during active invasive pulmonary aspergillosis (IPA). Despite receiving continuous antifungal treatment and multiple gran- ulocyte infusions, her IPA was aggravated. She underwent allogeneic HSCT from a matched sibling donor using conditioning regimen of fludarabine, reduced dose of cyclo- phosphamide, and anti-thymocyte globulin (ATG) during IPA. After neutrophil engraft- ment, fever subsided and IPA improved. She was continued on voriconazole for 7 months after HSCT. She is alive with normal hematopoiesis 4 years post-transplant. Our report suggests that allogeneic HSCT using conditioning regimen of fludarabine, reduced dose of cyclophosphamide, and ATG can be a feasible option for the patients with vSAA even during active fungal infection.
pISSN 2233-5250 / eISSN 2233-4580 http://dx.doi.org/10.15264/cpho.2016.23.1.57 Clin Pediatr Hematol Oncol 2016;23:57∼60
Received on April 9, 2016 Revised on April 12, 2016 Accepted on April 14, 2016
Corresponding Author: Kyung-Nam Koh Department of Pediatrics, Asan Medical Center Children’s Hospital, University of Ulsan College of Medicine, 88 Olympic-ro 43-gil, Songpa-gu, Seoul 05505, Korea Tel: +82-2-3010-3386
Fax: +82-2-473-3725 E-mail: pedkkn@gmail.com
Key Words: Aplastic anemia, Hematopoietic stem cell transplantation, Invasive pulmo- nary aspergillosis
Introduction
Allogeneic hematopoietic stem cell transplantation (HSCT) is the treatment of choice for severe aplastic anemia (SAA). Active fungal infection is considered as a contra- indication for allogeneic HSCT due to high trans- plant-related mortality. However, patients with SAA (especially, very severe aplastic anemia [vSAA]), who have
active fungal infection, are difficult to be salvaged with an-
ti-fungal treatment alone, and allogeneic HSCT can be the
only treatment option for them. Here, we report a patient
who underwent successful allogeneic HSCT during severe
active invasive pulmonary aspergillosis (IPA) using con-
ditioning regimen of fludarabine, reduced dose of cyclo-
phosphamide, and anti-thymocyte globulin (ATG).
Euri Seo, et al
58 Vol. 23, No. 1, April 2016
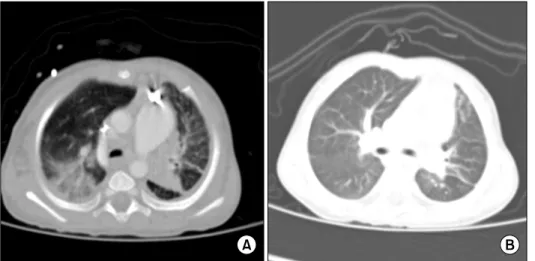
Fig. 1. (A) Chest CT, suggested invasive pulmonary aspergillosis, before allogeneic HSCT. HSCT, hematopoietic stem cell transplan- tation. (B) Significant improvement could be seen after allogeneic HSCT. HSCT, hematopoietic stem cell transplantation.
Case Report
A 2-month-old girl presented with tachypnea. Complete blood count (CBC) showed pancytopenia with a hemoglo- bin (Hb) level of 5.0 g/dL, a reticulocyte count of 7,195/L, a white blood cell (WBC) count of 2,000/L, an absolute neutrophil count (ANC) of 90/L and a platelet count of 4,000/L. The peripheral blood smear revealed leukopenia, neutropenia, normocytic normochromic anemia with aniso- poikilocytosis and thrombocytopenia. She had no organo- megaly, hypo- or hyperpigmentation, facial anomaly or skeletal deformity. Her height and weight were 52.8 cm (5 percentile), 3.3 kg (3 percentile), respectively. Bone mar- row aspirates and trephine biopsy specimen confirmed se- vere hypocellularity (<10%) without dysplasia or infiltrates, which was consistent with SAA. Marrow cytogenetics was normal, and there was no evidence of paroxysmal noctur- nal hemoglobinuria clone or chromosome fragility. Echo- cardiography revealed that she had perimembranous ven- tricular septal defects (VSD) and patent foramen ovale.
After diagnosis of SAA, she developed five episodes of neu- ropenic fever, which were resolved with empirical antibiotics.
At 6 month of age, she was admitted due to neutropenic fever. The laboratory findings were as follows: WBC 400/L; ANC 12/L; Hb 9.3 g/dL; platelet 23,000/L; C-re- active protein 18.37 mg/dL; galactomannan>10.0 S/C ratio (Signal to Cutoff ratio, normal<0.5). Chest computed to-
mography (CT) scan revealed the consolidation in the lin- gular division of upper lobe of left lung and pleural effu- sion in the left hemithorax, which suggested invasive fungal pneumonia. There were no abnormal findings on abdomi- nal CT. Because IPA was suspected, she was started on am- photericin B (AmB), along with teicoplanin and mer- openem as an empirical treatment. After 3 days, AmB was switched to liposomal AmB because of a sustained fever.
Because fever did not subside and pulmonary lesions were aggravated, liposomal AmB was switched to voriconazole.
In addition, she received 8 courses of granulocyte in- fusions. During granulocyte infusion, fever subsided tran- siently without significant improvement of pulmonary lesions.
Caspofungin was added to previous medication. However, fever persisted and dyspnea developed, causing her to be dependent on oxygen supply. Chest CT scan showed that pulmonary lesions were aggravated with cavitary lesion, multiple ground-glass opacity, atelectasis, and pleural effu- sion (Fig. 1). Because her condition did not improve de- spite receiving multiple courses of granulocyte infusions, and continuous antifungal treatment, she proceeded to un- dergo allogeneic HSCT from an HLA full matched sibling donor during her active invasive fungal infection. The con- ditioning regimen was composed of cyclophosphamide (60 mg/kg once daily i.v. on days −8, and −7), fludarabine (30 mg/m
2once daily i.v. on days −6, −5, −4, −3, and
−2), and rabbit-antithymocyte globulin (Thymoglobulin
Ⓡ, r-ATG, 2.5 mg/kg once daily i.v. on days −4, −3, and
−2). The infused cell dose of CD34 positive cells was
HSCT in a Case of SAA with Active IPA
Clin Pediatr Hematol Oncol 59
2.23×10
6/kg. For graft-versus-host disease (GVHD) pro- phylaxis, cyclosporine and methotrexate (10 mg/m
2on days 1, 3, and 6) were used. Alprostadil (Eglandin
Ⓡ) was used to prevent veno-occluisve disease (VOD). Teicoplanin and meropenem were continued during transplant because of a sustained neutropenic fever. For viral prophylaxis, acy- clovir was used. Monitoring for cytomegalovirus (CMV) and Epstein-Barr virus (EBV) was performed weekly using a pp65 antigenemia test (CMV) and real-time polymerase chain reaction (CMV, EBV) once weekly in the first 3 months and monthly thereafter until 6 months post- transplant. The recovery of the ANC to more than 500/L occurred at 10 days after stem cell infusion. Fever subsided after WBC engraftment. We stopped administration of cas- pofungin and continued her on voriconazole. After HSCT, her galactomannan titer was gradually decreased. On day 28, a bone marrow examination revealed normocellular marrow with bilineage regeneration and short tandem re- peat (STR) revealed a complete donor chimerism. Acute GVHD, VOD, CMV reactivation as well as regimen related toxicity including hemorrhagic cystitis did not occur. Chest CT scan at 4 months after HSCT showed that pulmonary lesions were nearly resolved (Fig. 1). She was continued on voriconazole until 7 months after HSCT. The patient is alive for 4 years after HSCT with normal hematopoiesis and without evidence of any infection and chronic GVHD.
Discussion
Although supportive cares such as transfusion, G-CSF use, and prophylactic antibiotics use have been introduced, SAA has a high mortality rate with supportive care alone [1]. HSCT from an HLA full matched sibling donor is the treatment of choice for SAA. Because invasive fungal in- fections (IFI) are likely to be reactivated during condition- ing for HSCT and can be fatal, patients with active IFI have been excluded from transplant programs. Indeed, tissue damage resulting from IFI or its therapy can increase trans- plantation mortality rates [2,3]. However, HSCT may be necessary to provide the best chance for early neutrophil recovery to some patients [4]. For this reason, HSCT can be considered for the patients with an active IFI. Several
authors have reported successful outcomes for HSCT in pa- tients with active IFI [3,5-7]
In the report by Martino et al, three patients had under- gone HSCT during active IFI while receiving AmB treatment [6]. All of them died of progressive fungal infection. In the report by Avivi et al, five patients had undergone HSCT with active IFI [8]. Their patients were continued on AmB or liposomal AmB. Four of five patients did not survive the transplant. Two of these patients died of fulminant fungal infection. In the report by Aki et al., however, seven of thirteen patients with active IFI died of fungal infection re- lated causes after the transplantation [5]. Four patients sur- vived and remained free of infection and relapse with me- dian follow up of 306 days. In their cohort, five of thirteen patients treated with a combination of new antifungal drugs: liposomal AmB±caspofungin or voriconazole, cas- pofungin+voriconazole. Three of the five patients who had received a combination therapy survived. Aki et al.
claimed that remarkable improvements in survival rates are due to a new generation of antifungal drugs including cas- pofungin and voriconazole. Our case also received a com- bination of voriconazole and caspofungin as antifungal agents. Our report suggests that these more effective and/or less toxic antifungal agents contributed to successful trans- plantation during active IFI.
Introduction of effective conditioning regimen without increasing toxicity has been reported as another factor for successful outcomes after HSCT with active IFI [7,9-11].
One of the most important factors influencing the re- currence of the invasive fungal infection is duration of pro- found neutropenia [9,12,13]. Cyclophosphamide (200 mg/kg) and ATG have been commonly used as the conditioning regimen for allogeneic HSCT from a matched sibling donor.
In our case, we used the conditioning regimen composed
of cyclophosphamide (120 mg/kg), fludarabine (150
mg/m
2), and r-ATG (7.5 mg/kg) to decrease the risk of car-
diotoxicity associated with high-dose cyclophosphamide,
because the patient had large VSDs. Fludarabine has been
successfully incorporated into conditioning regimen for un-
related HSCT for SAA [14]. With the addition of fludarabine
and reduction of cyclophosphamide dose, we could ach-
ieve the same degree of immunosuppressive effect and en-
Euri Seo, et al
60 Vol. 23, No. 1, April 2016
graftment without graft failure, which is considered a sig- nificant problem in HSCT in SAA patients.
In conclusion, our report suggests that allogeneic HSCT using conditioning regimen of fludarabine, reduced dose of cyclophosphamide, and r-ATG can be a feasible option for the patients with SAA even during active fungal infection.
References
1. Camitta BM, Thomas ED, Nathan DG, et al. A prospective study of androgens and bone marrow transplantation for treat- ment of severe aplastic anemia. Blood 1979;53:504-14.
2. Diaconescu R, Flowers CR, Storer B, et al. Morbidity and mor- tality with nonmyeloablative compared with myeloablative conditioning before hematopoietic cell transplantation from HLA-matched related donors. Blood 2004;104:1550-8.
3. Fukuda T, Boeckh M, Carter RA, et al. Risks and outcomes of invasive fungal infections in recipients of allogeneic hema- topoietic stem cell transplants after nonmyeloablative con- ditioning. Blood 2003;102:827-33.
4. Killick SB, Bown N, Cavenagh J, et al. Guidelines for the diag- nosis and management of adult aplastic anaemia. Br J Haematol 2016;172:187-207.
5. Aki ZS, Sucak GT, Yeğin ZA, Güzel O, Erbaş G, Senol E.
Hematopoietic stem cell transplantation in patients with active fungal infection: not a contraindication for transplantation.
Transplant Proc 2008;40:1579-85.
6. Martino R, Lopez R, Sureda A, Brunet S, Domingo-Albós A.
Risk of reactivation of a recent invasive fungal infection in pa- tients with hematological malignancies undergoing further in- tensive chemo-radiotherapy. A single-center experience and review of the literature. Haematologica 1997;82:297-304.
7. Singhal S, Safdar A, Chiang KY, et al. Non-myeloablative allo-
geneic transplantation ('microallograft') for refractory myeloma after two preceding autografts: feasibility and efficacy in a pa- tient with active aspergillosis. Bone Marrow Transplant 2000;26:1231-3.
8. Avivi I, Oren I, Haddad N, Rowe JM, Dann EJ. Stem cell trans- plantation post invasive fungal infection is a feasible task. Am J Hematol 2004;75:6-11.
9. Martino R, Parody R, Fukuda T, et al. Impact of the intensity of the pretransplantation conditioning regimen in patients with prior invasive aspergillosis undergoing allogeneic hema- topoietic stem cell transplantation: A retrospective survey of the Infectious Diseases Working Party of the European Group for Blood and Marrow Transplantation. Blood 2006;108:
2928-36.
10. Hermann S, Klein SA, Jacobi V, et al. Older patients with high-risk fungal infections can be successfully allografted us- ing non-myeloablative conditioning in combination with in- tensified supportive care regimens. Br J Haematol 2001;113:
446-54.
11. Fukuda T, Boeckh M, Guthrie KA, et al. Invasive aspergillosis before allogeneic hematopoietic stem cell transplantation:
10-year experience at a single transplant center. Biol Blood Marrow Transplant 2004;10:494-503.
12. Jantunen E, Ruutu P, Piilonen A, Volin L, Parkkali T, Ruutu T. Treatment and outcome of invasive Aspergillus infections in allogeneic BMT recipients. Bone Marrow Transplant 2000;
26:759-62.
13. Oren I, Haddad N, Finkelstein R, Rowe JM. Invasive pulmo- nary aspergillosis in neutropenic patients during hospital con- struction: before and after chemoprophylaxis and institution of HEPA filters. Am J Hematol 2001;66:257-62.
14. Kang HJ, Shin HY, Park JE, et al. Successful engraftment with fludarabine, cyclophosphamide, and thymoglobulin condition- ing regimen in unrelated transplantation for severe aplastic anemia: A phase II prospective multicenter study. Biol Blood Marrow Transplant 2010;16:1582-8.