A Novel Biomarker of Coronary Atherosclerosis: Serum DKK1 Concentration Correlates with Coronary Artery Calcification and Atherosclerotic Plaques
DKK1 modulates Wnt signaling, which is involved in the atherosclerosis. However, no data exist regarding the usefulness of measuring serum DKK1 concentration in predicting coronary atherosclerosis. A total of 270 consecutive patients (62.8 ± 11.2 yr; 70% male) were included. A contrast-enhanced 64-slice coronary MDCT was performed to identify the presence of atherosclerotic plaques. Agatston calcium scores (CS) were calculated to quantify the coronary artery calcification (CAC). DKK1 concentrations were measured by enzyme-linked immunosorbent assay. For each subsequent DKK1 quartile, there was a significant increase in CAC (P = 0.004) and the number of segments with coronary atherosclerosis (P < 0.001). In addition, DKK1 concentration was significantly higher in patients with atherosclerotic plaques, regardless of plaque composition (P = 0.01).
Multivariate analysis identified DKK1 as an independent risk factor for the presence of coronary atherosclerotic plaque. The adjusted odds ratio for coronary atherosclerotic plaque was 4.88 (95% CI, 1.67 to 14.25) for highest versus lowest quartile of the DKK1 levels. Furthermore, patients with DKK1 concentrations ≥ 68.6 pg/mL demonstrated coronary atherosclerotic plaques even when they had low CS. Serum DKK1 concentrations correlate with the coronary atherosclerosis and play an independent role in predicting the presence of coronary atherosclerosis.
Key Words: Dickkopf-1; Atherosclerosis; Vascular calcification; Biomarker Kwang-Il Kim1, Kyoung Un Park2,
Eun Ju Chun3, Sang Il Choi3, Young-Seok Cho1, Tae-Jin Youn1, Goo-Yeong Cho1, In-Ho Chae1, Junghan Song2, Dong-Ju Choi1 and Cheol-Ho Kim1
Departments of 1Internal Medicine, 2Laboratory Medicine and 3Radiology, Seoul National University College of Medicine, Bundang Hospital, Seongnam, Korea
Received: 25 April 2011 Accepted: 14 July 2011 Address for Correspondence:
Cheol-Ho Kim, MD
Department of Internal Medicine, Seoul National University College of Medicine Bundang Hospital, 166 Gumi-ro, Bundang-gu, Seongnam 463-707, Korea Tel: +82.31-787-7001, Fax: +82.31-787-4052 E-mail: cheolkim@snu.ac.kr
This work was supported by the Korea Research Foundation Grant, funded by the Korean Government (MOEHRD, Basic Research Promotion Fund) (KRF-2008-331-E00106) and by the Basic Science Research Program through the National Research Foundation of Korea (NRF), funded by the Ministry of Education, Science and Technology (2009-0063258).
http://dx.doi.org/10.3346/jkms.2011.26.9.1178 • J Korean Med Sci 2011; 26: 1178-1184 Cardiovascular Disorders
INTRODUCTION
Coronary artery calcium is a marker of subclinical coronary ath- erosclerotic disease and predicts coronary events. As a result, there has been considerable interest in the potential use of the coronary artery calcium score (CACS) using computed tomog- raphy (CT) in models of risk prediction (1). Furthermore, with the advance of technology, contrast-enhanced CT angiography can identify both calcified and non-calcified coronary athero- sclerotic plaques. The clinical usefulness of CACS and coronary CT angiography (CCTA) is well known and their use has recent- ly increased (2, 3). However, the concern regarding radiation ex- posure from CCTA has also increased (4).
A clinical risk score such as the Framingham risk score is help- ful in identifying the high-risk group. However, more than half of the cardiac events develop in low-risk patients (5). Accord- ingly, a more sophisticated method to stratify the cardiovascu- lar risk needs to be developed. Finding new biomarkers that can
identify and quantify the severity of coronary artery calcification (CAC) and atherosclerosis would be less expensive, avoid expo- sure to radiation, and be more accessible than imaging based methods.
The Wnt signaling pathways are involved in diverse develop- mental and physiological processes, including cell differentia- tion and tissue/organ morphogenesis (6). Recent evidence points to an important role of the Wnt signaling pathways in the regu- lation of inflammation (7). In addition, Wnt pathway activation enhances monocyte adhesion and regulates trans-endothelial migration of monocytes. As a result, the Wnt signaling pathway is involved in the process of atherosclerosis (8). Moreover, the Wnt signaling pathway plays an important role in the vascular calcification (9, 10).
The canonical Wnt pathway is regulated by multiple families of secreted antagonists such as the soluble frizzled related re- ceptors and dickkopf-1 (DKK1). DKK1 regulates Wnt signaling by binding to the Wnt co-receptor, LRP 5/6. Recently, enhanced
DKK1 expression was observed within advanced carotid plaques, suggesting that a DKK1-driven inflammatory loop could be op- erating within the atherosclerotic lesion (11). However, it has not been clearly demonstrated whether the serum concentration of DKK1 may be useful for predicting the extent of atherosclerosis or vascular calcification.
In this study, we aimed to evaluate the clinical significance of serum DKK1 concentration for predicting CAC and the presence of coronary atherosclerotic plaques.
MATERIALS AND METHODS Study population
We studied 270 consecutive subjects who visited Seoul National University Bundang Hospital complaining of chest pain from July 2006 through July 2008. The exclusion criteria were acute myocardial infarction, uncontrolled arrhythmia (ventricular tachycardia/fibrillation, atrial flutter/fibrillation, or atrioventric- ular block greater than second degree), contrast allergy, and re- nal dysfunction (serum creatinine > 2.0 mg/dL). Clinical infor- mation was gathered by personal interview and a physical ex- amination was performed by physicians. A biochemical evalu- ation and full medical examination were also performed.
The estimated pretest probability for coronary artery disease was estimated using the Duke clinical score, which includes type of chest discomfort, age, gender, and traditional risk factors. Sub- jects were categorized into a low (1% to 30%), intermediate (31%
to 70%), or high (71% to 99%) risk group of having coronary ar- tery disease (12).
Coronary multidetector computed tomography (MDCT) and coronary artery calcium scoring
All subjects were examined using the same CT unit and scanning protocols. All CT scans were performed using a 64-slice CCTA scanner (Brilliance 64, Philips Medical Systems, Best, The Neth- erlands) with 64 × 0.625-mm section collimation, 420-ms rota- tion time, 120-kV tube voltage, and 800-mA tube current under electrocardiographic-gated dose modulation. Before CCTA, all patients with a baseline heart rate > 70 beats/min received an intravenous esmolol of 10 to 30 mg (Jeil Pharm, Seoul, Korea).
Nitroglycerin 0.6 mg was administered sublingually immediate- ly before contrast injection (13). During CCTA acquisition, a bo- lus of 80 mL iomeprol (Iomeron 400, Bracco, Milan, Italy) was in- jected intravenously (4 mL/s) followed by a 50-mL saline chaser.
Coronary MDCT scans were analyzed independently by two experienced radiologists who were unaware of the clinical infor- mation and used a three-dimensional workstation (Brilliance, Philips Medical Systems). Agatston calcium scores (CS) were calculated to quantify the extent of CAC (14). The presence of coronary atherosclerotic plaque was evaluated according to the modified American Heart Association classification (15). The
contrast-enhanced portion of the coronary lumen was semi- automatically traced at the maximal stenotic site and compared with the mean value of the proximal and distal reference sites.
Structures that were > 1 mm2 within and/or adjacent to the ves- sel lumen were defined as plaques. Three groups of plaques were classified: lesions in which > 50% of the plaque area was occu- pied by calcified tissue (density > 130 Hounsfield unit in native scans) were classified as calcified, lesions with < 50% calcium as mixed, and lesions without any calcium were classified as non- calcified (16).
Measurement of serum DKK1 concentration
DKK1 concentrations were measured by enzyme-linked immu- nosorbent assay according to the manufacturer’s instructions (DuoSet ELISA development kit, R&D Systems Inc., Minneapo- lis, MN, USA).
Definitions
Hypertension was defined as blood pressure ≥ 140/90 mmHg or taking any antihypertensive medications. Diabetes mellitus was defined by a fasting blood glucose ≥ 126 mg/dL or a history of or treatment for hyperglycemia. Hypercholesterolemia was defined by a total cholesterol ≥ 200 mg/dL or treatment for hyper- cholesterolemia. Ischemic heart disease was defined by a histo- ry of angina, myocardial infarction, or previous treatment with coronary medications or intervention for heart disease. Smok- ing status was classified into current smokers (smoked within the last month), ex-smokers (given up for more than one month), and non-smokers.
Statistical analysis
Statistical analyses were performed using SPSS (version 15.0, SPSS Inc., Chicago, IL, USA) or MedCalc (version 11.0, MedCalc software, Mariakerke, Belgium). Continuous variables are ex- pressed as mean ± SD. Because serum DKK1 levels and CACS were not normally distributed, the values are also reported as median and interquartile range (IQR). Continuous variables were compared by either the unpaired Student’s t-test or analy- sis of variance (ANOVA) followed by post-hoc comparison with the Scheffe test. Discrete variables are expressed as counts and percentages, and the chi-squared or Fisher’s exact test was used to compare proportions. Correlation analyses were performed using the Pearson and Spearman coefficients of correlation for parametric and nonparametric variables, respectively. Multiple logistic regressions were employed to assess the independent association of DKK1 concentration and CACS with the presence of coronary atherosclerotic plaque. Differences in the predicted value were estimated by comparing the area under the receiver- operating characteristic curve (AUC), taking the correlation be- tween the areas into account. We also calculated the c-statistic for models with conventional risk factors with and without CACS
or DKK1. All statistical analyses were two-tailed, and P values <
0.05 were considered statistically significant.
Ethics statement
All subjects provided informed consent and the study was ap- proved by the institutional review board at Seoul National Uni- versity Bundang Hospital (IRB number: B-0807/059-004).
RESULTS
Baseline characteristics of study subjects
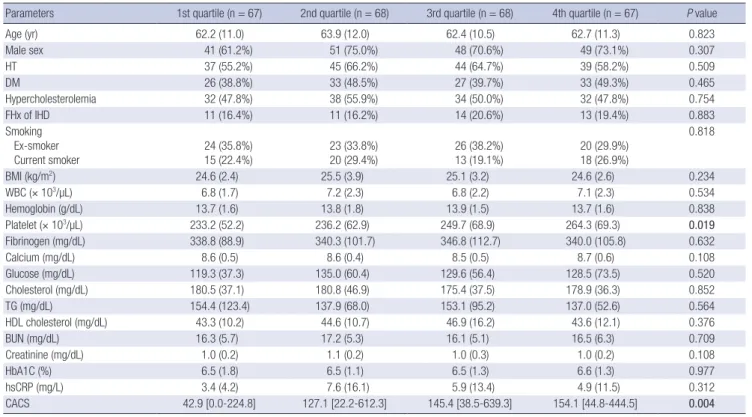
A total of 270 consecutive patients with chest pain were includ- ed. The mean age was 62.8 ± 11.2 yr (range: 31-92 yr), and males comprised 70% of subjects. Of the 270 patients, 41 (15%) patients showed no evidence of coronary artery calcium. The mean value of CACS was 338.1 ± 518.7 (median 112.9, IQR 16.9-450.6). The mean serum concentration of DKK1 was 134.5 ± 127.2 pg/mL (median 99.8, IQR 61.6-158.5). Both CACS and DKK1 concen- tration showed skewed distributions. Clinical and laboratory characteristics of the patients are presented in Table 1 accord- ing to the quartile of DKK1 concentration. A significant increase in platelet count that correlated with increasing quartiles of DKK1 concentration was identified. All other variables were not differ- ent among the DKK1 quartiles.
Association between DKK1 concentration and coronary atherosclerosis
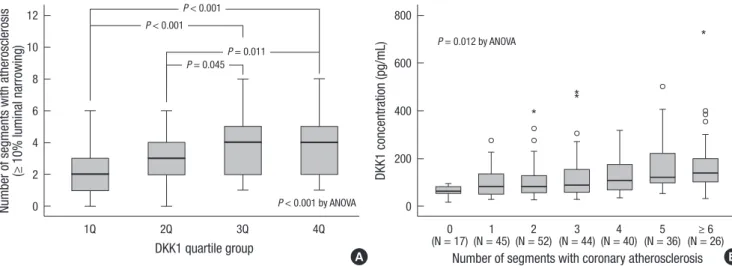
The serum concentration of DKK1 was positively but weakly cor- related with CACS (Spearman’s rho = 0.191, P = 0.002). CAC was significantly associated with the level of DKK1. The median (IQR) values of the CACS were 42.9 (0.0-224.8), 127.1 (22.2-612.3), 145.4 (38.5-639.3), and 154.1 (44.8-444.5) in the lowest, second, third, and highest quartiles of DKK1 level (P = 0.004). Also, the distri- bution of DKK1 and CACS quartiles were closely associated (P = 0.021). Overall, any coronary atherosclerotic plaque (≥ 10% lu- minal narrowing) was detected in 253 (94%) subjects, and the mean number of segments with coronary atherosclerotic plaques was 3.4 ± 1.8 per subjects. The number of segments with coro- nary atherosclerosis was significantly higher in groups with high- er DKK1 concentrations (P < 0.001) (Fig. 1A). In addition, DKK1 concentration was significantly elevated according to the global coronary atherosclerotic burden (Fig. 1B).
Significant coronary atherosclerotic stenosis (≥ 50% luminal narrowing) was identified in 212 (79%) subjects. Among these patients, 79 subjects had exclusively non-calcified plaques, 25 subjects had exclusively calcified plaques, and 108 subjects had both and, thus, were classified as having mixed plaques. DKK1 was significantly elevated in patients with coronary atheroscle- rotic stenosis (median [IQR] with DKK1 concentrations of 63.2 [52.7-102.8] pg/mL, 105.2 [64.4-169.1] pg/mL, and 108.5 [72.0-
Table 1. Comparison of clinical and laboratory characteristics according to the DKK1 quartile group
Parameters 1st quartile (n = 67) 2nd quartile (n = 68) 3rd quartile (n = 68) 4th quartile (n = 67) P value
Age (yr) 62.2 (11.0) 63.9 (12.0) 62.4 (10.5) 62.7 (11.3) 0.823
Male sex 41 (61.2%) 51 (75.0%) 48 (70.6%) 49 (73.1%) 0.307
HT 37 (55.2%) 45 (66.2%) 44 (64.7%) 39 (58.2%) 0.509
DM 26 (38.8%) 33 (48.5%) 27 (39.7%) 33 (49.3%) 0.465
Hypercholesterolemia 32 (47.8%) 38 (55.9%) 34 (50.0%) 32 (47.8%) 0.754
FHx of IHD 11 (16.4%) 11 (16.2%) 14 (20.6%) 13 (19.4%) 0.883
Smoking Ex-smoker
Current smoker 24 (35.8%)
15 (22.4%) 23 (33.8%)
20 (29.4%) 26 (38.2%)
13 (19.1%) 20 (29.9%)
18 (26.9%)
0.818
BMI (kg/m2) 24.6 (2.4) 25.5 (3.9) 25.1 (3.2) 24.6 (2.6) 0.234
WBC (× 103/µL) 6.8 (1.7) 7.2 (2.3) 6.8 (2.2) 7.1 (2.3) 0.534
Hemoglobin (g/dL) 13.7 (1.6) 13.8 (1.8) 13.9 (1.5) 13.7 (1.6) 0.838
Platelet (× 103/µL) 233.2 (52.2) 236.2 (62.9) 249.7 (68.9) 264.3 (69.3) 0.019
Fibrinogen (mg/dL) 338.8 (88.9) 340.3 (101.7) 346.8 (112.7) 340.0 (105.8) 0.632
Calcium (mg/dL) 8.6 (0.5) 8.6 (0.4) 8.5 (0.5) 8.7 (0.6) 0.108
Glucose (mg/dL) 119.3 (37.3) 135.0 (60.4) 129.6 (56.4) 128.5 (73.5) 0.520
Cholesterol (mg/dL) 180.5 (37.1) 180.8 (46.9) 175.4 (37.5) 178.9 (36.3) 0.852
TG (mg/dL) 154.4 (123.4) 137.9 (68.0) 153.1 (95.2) 137.0 (52.6) 0.564
HDL cholesterol (mg/dL) 43.3 (10.2) 44.6 (10.7) 46.9 (16.2) 43.6 (12.1) 0.376
BUN (mg/dL) 16.3 (5.7) 17.2 (5.3) 16.1 (5.1) 16.5 (6.3) 0.709
Creatinine (mg/dL) 1.0 (0.2) 1.1 (0.2) 1.0 (0.3) 1.0 (0.2) 0.108
HbA1C (%) 6.5 (1.8) 6.5 (1.1) 6.5 (1.3) 6.6 (1.3) 0.977
hsCRP (mg/L) 3.4 (4.2) 7.6 (16.1) 5.9 (13.4) 4.9 (11.5) 0.312
CACS 42.9 [0.0-224.8] 127.1 [22.2-612.3] 145.4 [38.5-639.3] 154.1 [44.8-444.5] 0.004
Data are presented as mean (SD) or number (%). CACS are presented as median [IQR]. DKK1, dickkopf-1; HT, hypertension; DM, diabetes mellitus; FHx of IHD, family history of ischemic heart disease; BMI, body mass index; WBC, white blood cell; TG, triglyceride; HDL, high density lipoprotein; BUN, blood urea nitrogen; HbA1C, hemoglobin A1C; hsCRP, high sensitivity C-reactive protein; CACS, coronary artery calcium score. Cutoff values for DKK1 quartiles were 61.6 pg/mL, 99.8 pg/mL, and 158.5 pg/mL.
183.2] pg/mL in patients without plaque, with non-calcified plaque, and with mixed or calcified plaque, respectively) (P = 0.01) (Fig. 2).
The association between DKK1 concentration and coronary atherosclerotic stenosis was not different according to the pretest risk profile evaluated using the Duke clinical score. The frequen- cy of coronary atherosclerotic stenosis was significantly increased according to the level of DKK1, both in the low to intermediate- risk group (n = 72) and in the high-risk group (n = 198).
Comparison of CACS and DKK1 in predicting the presence of coronary atherosclerotic stenosis
The levels of CACS were significantly higher in patients with cal- cified or mixed plaque. However, the values were not different in patients with non-calcified plaque compared to patients with- out plaques (Fig. 3).
The AUC for the DKK1 concentration was 0.678 (95% CI: 0.619- 0.734), which was comparable to that of CACS (AUC 0.729, 95%
CI: 0.672-0.782) (P = 0.260). The sensitivity and specificity of DKK1 levels ≥ 68.6 pg/mL for the presence of coronary atherosclerotic plaques were 77% (71%-82%) and 55% (42%-68%), respectively.
Number of segments with atherosclerosis (≥ 10% luminal narrowing) DKK1 concentration (pg/mL)
DKK1 quartile group
Number of segments with coronary atherosclerosis
*
**
*
1Q 2Q 3Q 4Q 0 1 2 3 4 5 ≥ 6
(N = 17) (N = 45) (N = 52) (N = 44) (N = 40) (N = 36) (N = 26) 12
10 8 6 4 2 0
800
600
400
200
0
A B
P < 0.001
P < 0.001 by ANOVA
P = 0.012 by ANOVA P = 0.045P = 0.011
P < 0.001
Fig. 1. Association between DKK1 concentration and coronary atherosclerotic plaque. Number of coronary artery segments with any atherosclerotic plaque (≥ 10% luminal nar- rowing) was evaluated in all the subjects, and 253 (94%) subjects showed more than one coronary atherosclerotic plaque. The number of segments with coronary atheroscle- rosis was significantly increased with increasing DKK1 quartiles (A). In addition, DKK1 concentration was significantly elevated according to the number of coronary artery seg- ments with any atherosclerotic plaque (B). An outliers (open circles) are defined as a score that is between 1.5 and 3 box lengths away from the upper edge of the box. An ex- treme scores (asterisks) are defined as a score that is greater than 3 box lengths away from the upper edge of the box.
DKK1 concentration (pg/mL)
No plaque Non-calcified plaque Mixed or calcified plaque
(N = 58) (N = 79) (N = 133)
800
600
400
200
0
**
*
*
P = 0.020
P = 0.028
P = 0.01 by ANOVA
Fig. 2. Comparison of DKK1 concentration according to the type of coronary athero- sclerotic plaque. DKK1 was significantly elevated in patients with both calcium-con- taining and non-calcified coronary atherosclerotic plaques compared to the patients without plaque. The central line represents distribution median, the boxes span from 25th to 75th percentiles, and the error bars extend from 10th to 90th percentiles. An outliers (open circles) are defined as a score that is between 1.5 and 3 box lengths away from the upper edge of the box. An extreme scores (asterisks) are defined as a score that is greater than 3 box lengths away from the upper edge of the box.
Coronary artery calcium score
No plaque Non-calcified plaque Mixed or calcified plaque
(N = 58) (N = 79) (N = 133)
3,000 2,500 2,000 1,500 1,000 500 0
*
*
***
**
*
***
P < 0.001
P = 0.989
P < 0.001 by ANOVA
Fig. 3. CACS according to the coronary atherosclerotic plaque classification. CACS was only increased in patients with calcium-containing plaques compared to the pa- tients without plaque. This difference showed the clinical advantage of DKK1 over CACS in predicting the presence of coronary atherosclerotic plaques without calcium deposits. Shown are box plots representing median and interquartile range (equiva- lently the 25th and 75th percentiles). An outliers (open circles) are defined as a score that is between 1.5 and 3 box lengths away from the upper edge of the box. An ex- treme scores (asterisks) are defined as a score that is greater than 3 box lengths away from the upper edge of the box.
For the prediction of coronary atherosclerotic plaques, im- provement in discrimination compared with the model with con- ventional risk factors was observed with inclusion of CACS (c- statistic = 0.735) in the model and with DKK1 (c-statistic = 0.717).
Addition of both CACS and DKK1 resulted in a statistically signif- icant increase of the c-statistic compared with the model based on clinical risk factor or clinical risk factor plus either CACS or DKK1 (Fig. 4, Table 2).
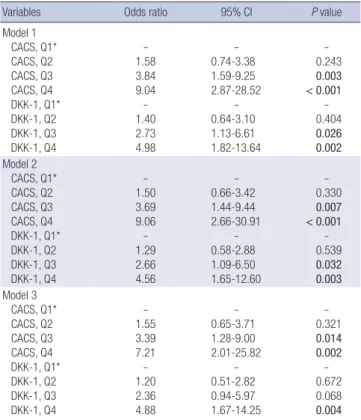
In multivariate analysis, CACS and DKK1 concentrations re- tained a strong association with the presence of coronary athero- sclerotic plaque after adjustment for age, gender, and other vari- ables (Table 3). Interestingly, the patients who had low CACS (Agatston CS < 154.1, cut-off value after the receiver-operating
Table 2. C-Statistics: Incremental prognostic value of CACS and DKK1 concentration regarding the presence of coronary atherosclerotic plaques
Model of plaques C-statistics P value* P value† P value‡
Model 1: Clinical risk indicator 0.634 (0.573-0.692)
Model 2: Clinical risk indicator + CACS 0.735 (0.678-0.787) 0.001
Model 3: Clinical risk indicator + DKK1 0.717 (0.659-0.770) 0.009 0.597
Model 4: Clinical risk indicator + CACS + DKK1 0.773 (0.719-0.822) < 0.001 0.05 0.01
Clinical risk indicator includes age, body mass index, hypertension, diabetes, and hypercholesterolemia. *P value comparing with model 1; †P value comparing with model 2; ‡P value comparing with model 3. DKK1, dickkopf-1; CACS, coronary artery calcium score.
Table 3. Unadjusted and adjusted OR and 95% confidence intervals derived from logistic regression analysis for the association between CACS and DKK1 concentra- tion with the presence of coronary atherosclerotic plaques
Variables Odds ratio 95% CI P value
Model 1 CACS, Q1*
CACS, Q2 CACS, Q3 CACS, Q4 DKK-1, Q1*
DKK-1, Q2 DKK-1, Q3 DKK-1, Q4
- 1.58 3.84 9.04 - 1.40 2.73 4.98
- 0.74-3.38 1.59-9.25 2.87-28.52
- 0.64-3.10 1.13-6.61 1.82-13.64
- 0.243 0.003
< 0.001 - 0.404 0.026 0.002 Model 2
CACS, Q1*
CACS, Q2 CACS, Q3 CACS, Q4 DKK-1, Q1*
DKK-1, Q2 DKK-1, Q3 DKK-1, Q4
- 1.50 3.69 9.06 - 1.29 2.66 4.56
- 0.66-3.42 1.44-9.44 2.66-30.91
- 0.58-2.88 1.09-6.50 1.65-12.60
- 0.330 0.007
< 0.001 - 0.539 0.032 0.003 Model 3
CACS, Q1*
CACS, Q2 CACS, Q3 CACS, Q4 DKK-1, Q1*
DKK-1, Q2 DKK-1, Q3 DKK-1, Q4
- 1.55 3.39 7.21 - 1.20 2.36 4.88
- 0.65-3.71 1.28-9.00 2.01-25.82
- 0.51-2.82 0.94-5.97 1.67-14.25
- 0.321 0.014 0.002 - 0.672 0.068 0.004 The dependent variable was the presence of coronary atherosclerotic plaque causing more than 50% stenosis. *The first quartile (Q1) was used as the reference value. Cut- off values were 16.9, 112.9, and 450.6 for CACS quartiles and 61.6 pg/mL, 99.8 pg/
mL, and 158.5 pg/mL for DKK1 quartiles. Model 1, unadjusted; Model 2, age and gen- der adjusted; Model 3, age, gender, hypertension, diabetes mellitus, hypercholesterol- emia, smoking, calcium, creatinine, fibrinogen, hsCRP, and platelet count adjusted.
Sensitivity
100-Specificity
Clinical Clinical + CACS Clinical + DKK1 Clinical + CACS + DKK1
0 20 40 60 80 100
100
80
60
40
20
0
Fig. 4. Role of DKK1 in predicting the presence of coronary atherosclerotic plaque.
The receiver operating characteristic curves illustrate clinical risk indicator including age, body mass index, hypertension, diabetes, and dyslipidemia alone or plus CACS and/or DKK1 concentration. Areas under the curves are 0.634 for clinical risk indica- tor alone, 0.735 for clinical risk indicator plus CACS, 0.717 for clinical risk indicator plus DKK1, and 0.773 for clinical risk indicator plus CACS and DKK1. The area under the curve for the receiver operating characteristic curve for clinical risk indicator plus CACS or DKK1, and CACS & DKK1 are significantly greater than that of the clinical risk indicator alone.
Fig. 5. Complementary role of DKK1 and CACS in identifying coronary atherosclerotic plaque. Patients who had low CACS (Agatston CS < 154.1) but high DKK1 concen- tration (DKK1 ≥ 68.6 pg/mL) show a similar probability of having coronary athero- sclerotic plaque as patients with high CACS.
100 (%)
75 50 25
0
Prevalence of coronary atherosclerotic plaques
DKK1 < 68.6 pg/mL
DKK1 ≥ 68.6 pg/mL
CACS < 154.1 CACS ≥ 154.1
characteristic curve analysis) but DKK1 ≥ 68.6 pg/mL showed a similar probability of having coronary atherosclerotic plaque as patients with high CACS (Agatston CS ≥ 154.1) (Fig. 5).
DISCUSSION
In this study, we demonstrated that DKK1 concentration signif- icantly correlated with CAC and the presence of coronary ath- erosclerotic plaque. Furthermore, in patients with a low CACS, DKK1 concentration could be useful to identify the presence of coronary plaque.
CACS alone can rank the risk of coronary heart disease inde- pendently of the clinical risk profile and shows good correlation with calcified atherosclerotic plaque. However, the efficacy of CACS for predicting non-calcified coronary plaques has shown limited potential (17). Moreover, a zero CACS result does not ex- clude significant coronary artery stenosis or the need for coro- nary revascularization (18).
Contrary to CACS, DKK1 can identify non-calcified as well as calcium-containing plaques without radiation exposure. In ad- dition, DKK1 provides incremental information regarding the prediction of coronary atherosclerotic plaque beyond tradition- al risk factors. All of these results merit further investigation of DKK1 measurement in various clinical situations for identifying coronary atherosclerosis.
The hallmark of the DKK family is its ability to modulate Wnt signaling. The founding member of the family, DKK1, was dis- covered by its ability to block Wnt signaling (19, 20). The Wnt sig- naling pathway is involved in inflammation and atherosclero- sis. In addition, the role of Wnt signaling during vascular calcifi- cation has been established. Aicher et al. have shown that DKK1 induces the osteoclast differentiation factor RANKL, which has an important role in vascular calcification (21, 22). Moreover, Ueland et al. (11) have demonstrated that DKK1 expression is enhanced in advanced carotid plaques and that DKK1 is a novel mediator in platelet-mediated endothelial cell activation, which could occur within the atherosclerotic lesions. All of these find- ings suggest that DKK1 may modulate vascular calcification and atherosclerosis. However, until now there was no concrete evi- dence showing the clinical implication of measuring serum DKK1 concentrations in the patients.
In this study, we observed a positive correlation between the serum concentration of DKK1 and CAC. Furthermore, the DKK1 concentration was significantly increased in patients with CAC and atherosclerotic plaques. Interestingly, DKK1 concentration was significantly different between patients without plaque and with non-calcified plaque; however, CACS showed no difference between these patients.
With the advance of technological improvement, CCTA could characterize coronary atherosclerotic plaques. New technologies enable us to identify non-calcified coronary plaques, but there
are concerns about the associated radiation exposure. Accord- ingly, a new method to identify both non-calcified and calcium- containing plaques needs to be developed. From this point of view, the measurement of DKK1 concentration in addition to CACS would be beneficial for the prediction of coronary artery disease in patients with chest pain. However, it is not obvious whether this result could also be applied to other populations, such as asymptomatic individuals or other ethnic backgrounds.
Furthermore, it is not clear whether DKK1 is also useful to pre- dict systemic atherosclerosis other than coronary atherosclero- sis. Accordingly, the association between DKK1 concentration and systemic atherosclerosis in carotid, aorta, and peripheral vessels need to be evaluated.
We observed a significant increase in platelet count that cor- related with increasing quartiles of DKK1 concentration. Previ- ous report demonstrated that DKK1 is a mediator in platelet-de- pendent endothelial activation (11). However, the association between DKK1 and coronary atherosclerotic plaques remained significant after adjustment for platelet count in multivariate analysis.
In conclusion, serum DKK1 concentrations correlate with the presence of CAC and play a role in predicting the presence of coronary atherosclerotic plaques. The measurement of DKK1 merits further investigation as a simple test for identifying coro- nary atherosclerosis without the risk of radiation exposure.
REFERENCES
1. Detrano R, Guerci AD, Carr JJ, Bild DE, Burke G, Folsom AR, Liu K, Shea S, Szklo M, Bluemke DA, O’Leary DH, Tracy R, Watson K, Wong ND, Kronmal RA. Coronary calcium as a predictor of coronary events in four racial or ethnic groups. N Engl J Med 2008; 358: 1336-45.
2. Rubinshtein R, Halon DA, Gaspar T, Jaffe R, Karkabi B, Flugelman MY, Kogan A, Shapira R, Peled N, Lewis BS. Usefulness of 64-slice cardiac com- puted tomographic angiography for diagnosing acute coronary syndromes and predicting clinical outcome in emergency department patients with chest pain of uncertain origin. Circulation 2007; 115: 1762-8.
3. Greenland P, LaBree L, Azen SP, Doherty TM, Detrano RC. Coronary artery calcium score combined with Framingham score for risk predic- tion in asymptomatic individuals. JAMA 2004; 291: 210-5.
4. Einstein AJ, Henzlova MJ, Rajagopalan S. Estimating risk of cancer asso- ciated with radiation exposure from 64-slice computed tomography cor- onary angiography. JAMA 2007; 298: 317-23.
5. Bamberg F, Dannemann N, Shapiro MD, Seneviratne SK, Ferencik M, Butler J, Koenig W, Nasir K, Cury RC, Tawakol A, Achenbach S, Brady TJ, Hoffmann U. Association between cardiovascular risk profiles and the presence and extent of different types of coronary atherosclerotic plaque as detected by multidetector computed tomography. Arterioscler Thromb Vasc Biol 2008; 28: 568-74.
6. Peifer M, Polakis P. Wnt signaling in oncogenesis and embryogenesis: a look outside the nucleus. Science 2000; 287: 1606-9.
7. Sen M, Ghosh G. Transcriptional outcome of Wnt-Frizzled signal transduc- tion in inflammation: evolving concepts. J Immunol 2008; 181: 4441-5.
8. Christman MA 2nd, Goetz DJ, Dickerson E, McCall KD, Lewis CJ, Benen- cia F, Silver MJ, Kohn LD, Malgor R. Wnt5a is expressed in murine and human atherosclerotic lesions. Am J Physiol Heart Circ Physiol 2008; 294:
H2864-70.
9. Shao JS, Cheng SL, Pingsterhaus JM, Charlton-Kachigian N, Loewy AP, Towler DA. Msx2 promotes cardiovascular calcification by activating paracrine Wnt signals. J Clin Invest 2005; 115: 1210-20.
10. Kirton JP, Crofts NJ, George SJ, Brennan K, Canfield AE. Wnt/beta-catenin signaling stimulates chondrogenic and inhibits adipogenic differentia- tion of pericytes: potential relevance to vascular disease? Circ Res 2007;
101: 581-9.
11. Ueland T, Otterdal K, Lekva T, Halvorsen B, Gabrielsen A, Sandberg WJ, Paulsson-Berne G, Pedersen TM, Folkersen L, Gullestad L, Oie E, Hans- son GK, Aukrust P. Dickkopf-1 enhances inflammatory interaction be- tween platelets and endothelial cells and shows increased expression in atherosclerosis. Arterioscler Thromb Vasc Biol 2009; 29: 1228-34.
12. Pryor DB, Shaw L, McCants CB, Lee KL, Mark DB, Harrell FE Jr, Muhl- baier LH, Califf RM. Value of the history and physical in identifying pa- tients at increased risk for coronary artery disease. Ann Intern Med 1993;
118: 81-90.
13. Chun EJ, Lee W, Choi YH, Koo BK, Choi SI, Jae HJ, Kim HC, So YH, Chung JW, Park JH. Effects of nitroglycerin on the diagnostic accuracy of electro- cardiogram-gated coronary computed tomography angiography. J Com- put Assist Tomogr 2008; 32: 86-92.
14. Agatston AS, Janowitz WR, Hildner FJ, Zusmer NR, Viamonte M Jr, De- trano R. Quantification of coronary artery calcium using ultrafast com- puted tomography. J Am Coll Cardiol 1990; 15: 827-32.
15. Austen WG, Edwards JE, Frye RL, Gensini GG, Gott VL, Griffith LS, Mc- Goon DC, Murphy ML, Roe BB. A reporting system on patients evaluat- ed for coronary artery disease. Report of the Ad Hoc Committee for Grad- ing of Coronary Artery Disease, Council on Cardiovascular Surgery, Amer-
ican Heart Association. Circulation 1975; 51(4 Suppl): 5-40.
16. Choi EK, Chun EJ, Choi SI, Chang SA, Choi SH, Lim S, Rivera JJ, Nasir K, Blumenthal RS, Jang HC, Chang HJ. Assessment of subclinical coronary atherosclerosis in asymptomatic patients with type 2 diabetes mellitus with single photon emission computed tomography and coronary com- puted tomography angiography. Am J Cardiol 2009; 104: 890-6.
17. Scholte AJ, Schuijf JD, Kharagjitsingh AV, Jukema JW, Pundziute G, van der Wall EE, Bax JJ. Prevalence of coronary artery disease and plaque mor- phology assessed by multi-slice computed tomography coronary angiog- raphy and calcium scoring in asymptomatic patients with type 2 diabe- tes. Heart 2008; 94: 290-5.
18. Gottlieb I, Miller JM, Arbab-Zadeh A, Dewey M, Clouse ME, Sara L, Niinuma H, Bush DE, Paul N, Vavere AL, Texter J, Brinker J, Lima JA, Rochitte CE. The absence of coronary calcification does not exclude ob- structive coronary artery disease or the need for revascularization in pa- tients referred for conventional coronary angiography. J Am Coll Cardiol 2010; 55: 627-34.
19. Niehrs C. Function and biological roles of the Dickkopf family of Wnt modulators. Oncogene 2006; 25: 7469-81.
20. Glinka A, Wu W, Delius H, Monaghan AP, Blumenstock C, Niehrs C. Dick- kopf-1 is a member of a new family of secreted proteins and functions in head induction. Nature 1998; 391: 357-62.
21. Panizo S, Cardus A, Encinas M, Parisi E, Valcheva P, Lépez-Ongil S, Coll B, Fernandez E, Valdivielso JM. RANKL increases vascular smooth mus- cle cell calcification through a RANK-BMP4-dependent pathway. Circ Res 2009; 104: 1041-8.
22. Aicher A, Kollet O, Heeschen C, Liebner S, Urbich C, Ihling C, Orlandi A, Lapidot T, Zeiher AM, Dimmeler S. The Wnt antagonist Dickkopf-1 mo- bilizes vasculogenic progenitor cells via activation of the bone marrow endosteal stem cell niche. Circ Res 2008; 103: 796-803.
AUTHOR SUMMARY
A Novel Biomarker of Coronary Atherosclerosis: Serum DKK1 Concentration Correlates with Coronary Artery Calcification and Atherosclerotic Plaques
Kwang-Il Kim, Kyoung Un Park, Eun Ju Chun, Sang Il Choi, Young-Seok Cho, Tae-Jin Youn, Goo-Yeong Cho, In-Ho Chae, Junghan Song, Dong-Ju Choi and Cheol-Ho Kim
Here, we show that DKK1 concentration is significantly associated with coronary artery calcification and coronary atherosclerotic plaques. Furthermore, in patients with low calcium scores, DKK1 concentration is valuable in differentiating the presence of coronary plaques. Accordingly, measuring the serum DKK1 concentration is clinically useful for identifying coronary atherosclerosis.