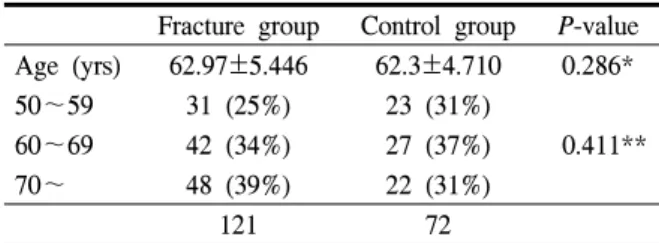
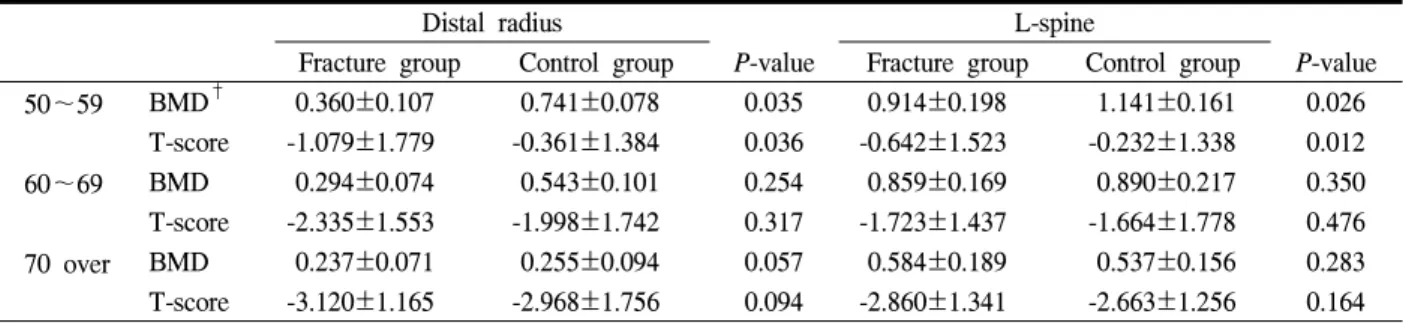
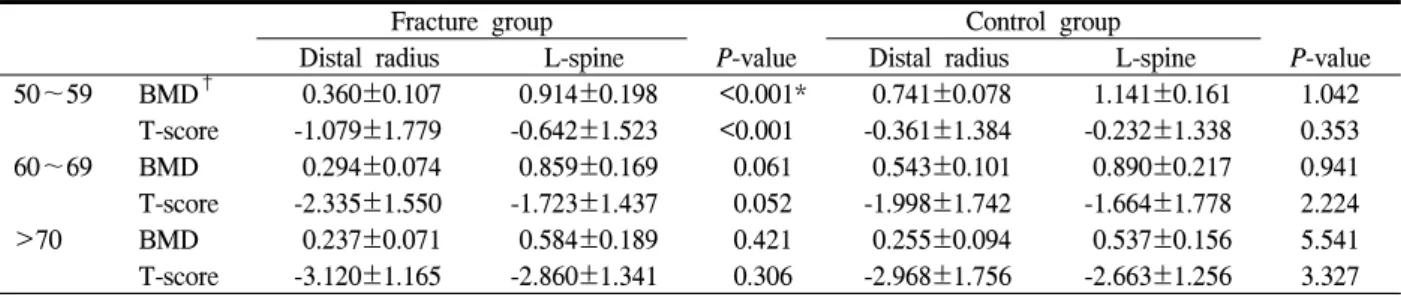
Regional Bone Loss as a Risk Factor for Distal Radius Fracture in Women under 60 Years Old
전체 글
수치
관련 문서
: Bone response to unloaded titanium implants with a sandblasted and acid-etched surface : A histomorphometric study in the canine mandible.. : Early
Bone transplants, autogenous bones, allogenic bones, xenogenic bones, and synthetic bone substitutes have all been used as bone graft materials.. However,
Result of patients’indirect markers reflecting bone quantity and quality (CTX : C-terminal cross-linking telopeptide of type 1 collagen, FRAX : Fracture Risk
Bone is a common site of distant metastasis in prostate cancer. Association of bone and metastatic cancer cells are important in this site-specific manifestation
Bone mineral content (BMC) and bone mineral density (BMD) of the lumbar spine, total hip, and proximal femur were measured before and after exercise... Results : 1) Body
In 4-week group, the group filled with bone graft with decortication revealed larger new bone formation area than shown in the group that had a defect area
It might also act in conjunction with a growth factor, such as bone morphogenic protein (BMP), insulin-like growth factor, or platelet-derived growth factor.
High complication rate in locking plate fixation of lower periprosthetic distal femur fractures in patients with total knee arthroplasties.. Management and