Journal of the Korean Glaucoma Society
Introduction
Management of systemic lupus erythematosus (SLE) includes long-term steroid therapy with dose-escalation or dose-reduction of drug according to severity of disease.1 Long-term medication of steroid could elevate intraocular pressure (IOP) in some people from reduction in facility of aqueous outflow, which leads to glaucomatous optic atrophy and loss of vision. Uncontrolled IOP with maximum medical treatment predisposes patients to
undergo glaucoma surgery.2 Intraocular bleeding after glaucoma surgery is not common complication in general.3 When hyphema or retinal hemorrhage involving macula does not resolved well or recurrent hemorrhage occurs, they became significant causing the failure of surgery. We report unexpected two cases with massive intraocular bleeding after glaucoma surgery in patients with SLE.
Case Report
Case 1
An 18-year old male was diagnosed with SLE and has been medicated with prednisolone for about 2 years. He was referred for ophthalmologic clinic with symptom of blurred vision in both eyes. IOP was elevated to about 30 mmHg with best-corrected visual acuity from 20/25 to 20/20 in both eyes. Slit-lamp biomicroscopy as well as gonioscopy
전신성 홍반성 루프스 환자에서 녹내장 수술 후 드문 안내출혈 발생 2예
Unusual Severe Intraocular Hemorrhage Following Glaucoma Surgery in Patients with Systemic Lupus Erythematous
정경인, 박찬기
Kyoung In Jung, MD, PhD, Chan Kee Park, MD, PhD
가톨릭대학교 의과대학 서울성모병원 안과
Department of Ophthalmology, Seoul St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
Purpose: Severe intraocular bleeding is not a common complication following glaucoma surgery in general. The authors report two cases with history of systemic lupus erythematous (SLE) developing severe intraocular bleeding in anterior segment or posterior segment after glaucoma surgery on diagnosis of steroid induced glaucoma.
Case summary: An 18-year-old male with a history of SLE and being medicated with prednisolone was referred for ophthalmologic clinic with elevated intraocular pressure (IOP). Laboratory examination presented no abnormality in coagulation profile and dilated fundus examination did not show lupus retinopathy preoperatively. After two each glaucoma surgery, slit-lamp biomicroscopy revealed persistent hyphema and severe subhyaloid hemorrhage, respectively. Following unresolved subhyaloid hemorrhage and retinal detachment, vitrectomy was performed. A 17-year-old female with SLE and long- term use of steroid underwent glaucoma surgery because of uncontrolled IOP. She also developed considerable hyphema postoperatively.
Conclusions: A rigorous analysis for bleeding risk preoperatively, and close attention for glaucoma surgery in SLE patients should be preceded although there is no high risk of hemorrhage in laboratory profile.
Key words: Glaucoma surgery, Intraocular hemorrhage, Systemic lupus erythematous
Received: 2019. 07. 19. Revised: 2019. 12. 17.
Accepted: 2019. 12. 23.
Corresponding Author: Chan Kee Park, MD, PhD
Department of Ophthalmology and Visual Science, Seoul St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, #202 Banpo-daero, Seocho-gu, Seoul 06591, Korea
Tel: +82-2-2258-6199, Fax: +82-2-599-7405 E-mail: ckpark@catholic.ac.kr
Journal of the Korean Glaucoma Society 2019;8(2):74-77
Case Report
www.koreanglaucoma.org
75
Jung KI, et al. : Unusual intraocular hemorrhage in patients with SLE
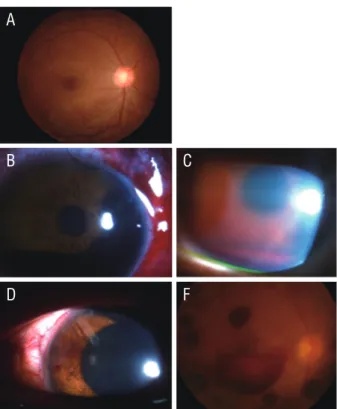
indicated no abnormal findings. There was no neovascu- larization of the iris (NVI) or the angle (NVA). Based on the Shaffer gonioscopy grading system, he was classified as grade 4. Dilated fundus examination displayed no lupus retinopathy such as vasculitis (Fig. 1). Elevated IOP was considered to arise from long-term use of steroid. One year after first visit, IOP in his right eye was uncontrolled to 25-40 mmHg under maximal medical therapy. After confirming preoperative laboratory examination presenting no abnormal coagulation profile, trabeculectomy was performed with no intraoperative complication. One day after glaucoma surgery, blood clot was found in anterior chamber (Fig. 1). Two days postoperatively, 4 mm- hyphema developed and bleb was filled with blood clot.
Prothrombic disorder such as antiphospholipid syndrome was excluded by negative result of laboratory profile.
Clinical symptom and blood test did not show evidence of lupus flare up. Following unresolved hyphema six days after surgery, anterior chamber was irrigated and tissue plasminogen activator was injected into anterior chamber.
With uncontrolled IOP with failed bleb despite resolved hyphema, glaucoma-drainage valve (Ahmed glaucoma valve®; New World Medical Inc., Rancho Cucamonga, CA, USA) was implanted. One day after second surgery, fundus examination demonstrated blot retinal hemorrhage and subhyaloid and vitreous hemorrhage as well as scattered blood clot in anterior chamber. His visual acuity reduced to 20/1,000 and IOP was 8 mmHg. Following resolution of vitreous hemorrhage, rhegmatogenous retinal detachment was disclosed and subhyaloid hemorrhage persisted.
Vitrectomy with endophotocoagulation applying to the area surrounding retinal hole was carried out, and retina was tamponated with silicone oil. No recurrence of retinal detachment was detected and IOP was well controlled until 3 months after surgery.
Case 2
The patient, a 17-year-old female with SLE visited glaucoma clinic because of uncontrolled IOP in her right eye. She was placed on prednisolone 20 mg and aspirin 100 mg since 14 years old. Her visual acuity was 20/20 in both eyes and IOP was 20-40 mmHg with glaucoma medication.
There was no NVI or NVA. According to the Shaffer goni-
Figure 1. Preoperative (A) and postoperative photograph (B-F, case 1). (A) Preoperative fundus photograph without any sign of lupus retinopathy. (B) Postoperative anterior segment photo of massive blood clot in anterior chamber one day after trabeculec- tomy. (C) Gross hyphema two days postoperatively. (D) Scattered blood clot in anterior chamber with well-positioned tube of glau- coma drainage valve and (E) subhyaloid hemorrhage and blot retinal hemorrhage and vitreous hemorrhage after Ahmed valve® implantation.
A
B C
D F
A B
Figure 2. Preoperative and postoperative photograph (case 2). (A) Preoperative fundus photograph without any sign of lupus reti- nopathy. (B) Postoperative anterior segment photo shows gross hyphema in the anterior chamber with prominent blood clot sur- rounding valve tip.
Journal of the Korean Glaucoma Society
Journal of The Korean Glaucoma SocieTy
76
Volume 8 | Number 2 2019oscopy grading system, she was classified as grade 4. With poorly controlled IOPs with reading as high as 40 mmHg despite maximum medical therapy and dose-reduction of steroid, selective laser trabeculoplasty was performed. Ini- tial postoperative response had been good, with IOPs in the mid-20s, but the IOP subsequently increased to 40 mmHg to 50 mmHg. Inferior retinal nerve fiber layer thickness decreased and glaucomatous visual field defect with nasal step progressed. She showed no sign of lupus retinopathy on fundus examination (Fig. 2). With diagnosis of steroid- induced glaucoma, placement of Ahmed glaucoma valve was performed after discontinuation of aspirin for 1 week.
Before surgery, laboratory examination presented no abnormal coagulation profile and slit-lamp examination did not displayed obvious source of bleeding and angle neovascularization. One day postoperatively, the right eye revealed a 1 mm-hyphema in the anterior chamber with prominent blood clot surrounding valve tip (Fig. 2). Visual acuity was 20/33 and IOP was 9 mmHg. The hyphema resolved over 2 weeks.
Discussion
In both cases with underlying SLE after glaucoma surgery, postoperative considerable hyphema or subhyaloid hemorrhage with retinal hemorrhage was unexpected because patients did not reveal lupus retinopathy or coagu- lation abnormality or laboratory profile which corresponded to antiphospholipid syndrome and discontinued medicine related to bleeding tendency. With regard to SLE, disease activity associated with SLE was not high, so it could not certainly account for bleeding tendency following glaucoma surgery. Especially with neovascular glaucoma, bleeding could occur commonly after glaucoma surgery from neovascularization in angle or iris. In our cases, however, slit-lamp examination revealed no neovascularization in angle or iris preoperatively.
We speculated that hemorrhagic tendency after surgery might result from subclinical endothelial dysfunction, fragile vessel from chronic steroid use. Zardi and Afeltra4 reported that SLE patients may have endothelial dysfunction
and vascular stiffness expressing structural changes in arterial walls subclinically even before atherosclerotic lesions arise. In addition, arterial stiffness is greater in adolescent and young SLE patients than in matched popu- lations.5 Our patients were diagnosed with SLE at the age of 16 and 14 years, respectively. Secondly, glucocorticoids are well known to have a severe negative effect on collagen formation, connective tissue strength, and wound healing.6 This effect on collagen could result in vessel wall weakness and increased susceptibility to massive intraocular hemor- rhage after glaucoma surgery. Acute lowering of IOP after glaucoma surgery may reduce resistance to blood flow, and the increased blood flow may overwhelm mechanical stability of the capillaries, resulting in multiple retinal hem- orrhages which are referred to decompression retinopathy.
In our first case, retinal hemorrhage with subhyaloid hemorrhage is not common type of decompression retinopathy, but very severe form of that. It was presumed to be deteriorated by subclinical endothelial dysfunction in SLE and fragile vessel by chronic use of steroid. It is advisable to carefully assess the potential risks of bleeding, and pay close attention for glaucoma surgery in SLE patients, even though there is no definite risk of bleeding in laboratory profile.
Conflicts of Interest
None of the authors has any financial or proprietary inter- est in any material or method mentioned.
References
1. Badsha H, Teh CL, Kong KO, et al. Pulmonary hemor- rhage in systemic lupus erythematosus. Semin Arthritis Rheum 2004;33:414-21.
2. Allingham RR, Damji KF, Freedman SF, et al. Shields textbook of glaucoma, 6th ed. Philadelphia: LWW, 2011;
344-5.
3. Gedde SJ, Schiffman JC, Feuer WJ, et al. Three-year follow-up of the tube versus trabeculectomy study. Am J Ophthalmol 2009;148:670-84.
4. Zardi EM, Afeltra A. Endothelial dysfunction and vascular stiffness in systemic lupus erythematosus: are they early
www.koreanglaucoma.org
77
Jung KI, et al. : Unusual intraocular hemorrhage in patients with SLE
markers of subclinical atherosclerosis? Autoimmun Rev 2010;9:684-6.
5. Chow PC, Ho MH, Lee TL, et al. Relation of arterial stiff- ness to left ventricular structure and function in adoles-
cents and young adults with pediatric-onset systemic lupus erythematosus. J Rheumatol 2007;34:1345-52.
6. Baxter JD, Forsham PH. Tissue effects of glucocorticoids.
Am J Med 1972;53:573-89.
국문초록
전신성 홍반성 루프스 환자에서 녹내장 수술 후 드문 안내출혈 발생 2예
목적: 녹내장 수술 후 일반적으로 심한 안내 출혈은 흔한 합병증은 아니다. 저자들은 전신성 홍반성 루프스 환자에서 스테로이드 유발 녹내장을 진단받고 녹내장 수술을 받은 후 안내 출혈이 발생한 증례 2예를 보고한다.
증례요약: 루푸스를 진단받고 스테로이드를 복용 중인 18세 남자 환자가 안압이 상승하여 본원에 내원하였다. 혈청학적 검사상 응고인자에 이상이 없었고 안저검사에서 루푸스 관련 망막병증은 관찰되지 않았다. 2번의 녹내장 수술 후 세극등현미경검사상 전방출혈과 심한 유리체하출혈이 각각 발생하였다. 유리체하출혈이 지속되고 망막박리가 발생하여 유리체절제술을 시행하였다. 두 번째 증례는 17세 여자 환자로 루푸스로 장기간 스테로이드 복용 과거력이 있었으며, 안압이 약물치료로도 조절되지 않아 녹내장 수술을 받았으나 술 후 심한 전방출혈이 발생하였다.
결론: 루프스 환자에서 녹내장 수술을 시행할 때 혈청학적 검사에서 높은 출혈 위험을 시사하는 소견이 없어도 출혈 가능성을 염두해두고 술 후 세심한 주의가 필요하겠다.