969
for Stress Urinary Incontinence in Aged Patients
Won Seok Sim, Kwang Yeom Lee, Khae Hawn Kim, Han Jung, Sang Jin Yoon
From the Department of Urology, Gachon University Gil Hospital, Incheon, Korea Purpose: There are few reports describing objective and subjective outcomes in aged patients undergoing distal urethral polypropylene sling (DUPS) and canal transobturator tape (canal TOT) placement, which make the submucosal mesh ‘tension-free’ state in the operating room. We evaluated surgical outcomes and subjective satisfaction in patients over 70 years of age who underwent DUPS and canal TOT for the treatment of stress urinary incontinence (SUI).
Materials and Methods: We studied 29 consecutive patients over 70 years of age who underwent DUPS and canal TOT for genuine SUI between January 2006 and April 2008. Surgical outcomes were determined on the basis of hemoglobin change, operative time, hospital stay, and complications.
Subjective satisfaction was determined on the basis of disease-specific quality of life, measured via the Incontinence Impact Questionnaire-short form (IIQ-7) and the Urogenital Distress Inventory-short form (UDI-6).
Results: No intraoperative or major postoperative complications were reported. No concomitant procedures were performed, including cystocele repair (n=0) or rectocele repair (n=0). The mean IIQ-7 and UDI-6 scores both decreased significantly after DUPS and canal TOT. Moreover, 82%
of patients reported no SUI symptoms under any circumstances, and 91%
of patients reported being rarely or never bothered by SUI symptoms.
Conclusions: The surgical outcomes and subjective satisfaction seen with DUPS and canal TOT in this study were superior to those seen in other studies. However, it is possible that this study overestimated the effects of DUPS and canal TOT in aged women because of the small study sample.
Therefore, additional studies are needed. (Korean J Urol 2009;50:969-975)
Key Words: Stress urinary incontinence, Questionnaires, Aged, Suburethral slings
Korean Journal of Urology Vol. 50 No. 10: 969-975, October 2009
DOI: 10.4111/kju.2009.50.10.969
Received:May 22, 2009 Accepted:September 23, 2009 Correspondence to: Khae Hawn Kim
Department of Urology, Gachon University Gil Hospital,1198, Guwol-dong, Namdong-gu, Incheon 405-760, Korea TEL: 032-460-8209 FAX: 032-460-8340
E-mail: kimcho99@gilhospital.com
Ⓒ The Korean Urological Association, 2009
INTRODUCTION
Stress urinary incontinence (SUI) is defined as involuntary urine leakage on effort, exertion, sneezing, or coughing without a rise in detrusor pressure [1]. The first sling procedure was developed in 1910 using the pyramidalis to form a muscular sling beneath the urethra. In 1942, newer sling procedure using the rectus fascia emerged; this procedure is considered to be the predecessor of modern sling techniques. The tension-free vaginal tape (TVT) procedure, first described by Ulmsten and Petros [2], is the most widely documented minimally invasive
surgical procedure for the treatment of female SUI. Recent studies have shown that despite a high associated success rate of 84-95% [3,4], TVT is not without complications. The most common complications related to the TVT procedure include voiding difficulties (8-17%), bladder perforation (2.7-17%), and symptoms of urgency (5-15%), all of which are complications normally associated with incontinence surgery [5-7]. Bowel perforation, necrotizing fasciitis, and large blood vessel injury are rare, but they have been reported [8,9]. To avoid these major complications, Delorme developed a procedure by which the tape is passed from a lateral approach through the obturator foramen on each side to support the mid-urethra [10]. This
method theoretically avoids some complications, such as bladder perforation and retropubic hematoma formation. The risks of bladder injury and voiding difficulty are lower, but the risks of vaginal erosion and groin pain are higher with the tension-free vaginal tape obturator route (TVTO)/transobturator tape (TOT) than with TVT [11].
Various surgical procedures have evolved for the treatment of female SUI, including distal urethral polypropylene sling [12] (DUPS, a modified TVT) [13] and canal TOT (modified TOT), which we intend to describe. Thus far, there have been few reports concerning the surgical results of similar procedures that adjust the tension of the mesh through the two lateral incisions made in the anterior vaginal wall at the level of the distal urethra. The purpose of our study was to evaluate the surgical efficacy and subjective satisfaction associated with DUPS and canal TOT in the treatment of SUI in elderly patients.
We conducted this prospective study based on patient symptoms, which were assessed by using the Korean translation of the Incontinence Impact Questionnaire-short form (IIQ-7) and the Urogenital Distress Inventory-short form (UDI-6) in Korean women over 70 years of age [14].
PATIENTS AND METHODS
We performed a prospective study of 29 consecutive patients over 70 years of age who underwent DUPS or canal TOT for genuine SUI between January 2006 and April 2008. During a 16-month period, 29 women with SUI were randomly assigned to receive either the DUPS or canal TOT procedure. DUPS or canal TOT was performed under spinal or general anesthesia with prophylactic antibiotics.
Early ambulation was encouraged to all patients posto- peratively. Exclusion criteria included age below 70 years, urge or mixed urinary incontinence, history of prior anti- incon- tinence surgery, urogenital organ prolapse of more than second degree severity (Baden-Walker), post-void residual urine volume greater than 100 ml, lower urinary tract anomalies, current urinary tract infection (UTI), more than three UTI episodes within the past year, previous radiation therapy to the pelvis, active malignancy, neurogenic disease (which can be associated with bladder disorders), inability to understand the purpose of the trial, and state of immobility. All patients completed at least 2 months of follow-up. Preoperatively, patients were evaluated with detailed medical histories and
physical assessments including pelvic examination, urinalysis, urine culture, voiding diary, cough stress test, post-void residual urine assessment, urodynamic studies, and standardized symptom questionnaires, which all patients had also completed before the most recent evaluation. All patients were asked to complete self-assessment questionnaires both preoperatively and postoperatively. The average follow-up period was 13 months (range, 2-28 months). We performed no concomitant surgeries or procedures such as cystocele repair, rectocele repair, or vaginal hysterectomy. A single surgeon performed all procedures. Postoperatively, the patients were evaluated at 2-month intervals with history, uroflowmetry, and post-void residual urine assessment. At each follow-up visit, the patients completed self-assessment questionnaires (IIQ-7 and UDI-6) without assistance from medical personnel. Surgical outcomes were determined on the basis of hemoglobin change, operative time, hospital stay, and complications. Subjective satisfaction was determined on the basis of disease-specific quality of life as indicated by the UDI-6 and IIQ-7. The institutional review board and ethics committee of the Gachon University Gil Hospital approved the study, and all patients gave written informed consent before participation.
1. Surgical technique
1) DUPS: In this procedure, a thermally bonded polypro- pylene tape is prepared, and a 0 polyglactin suture is placed at each end. Two oblique lateral incisions are made in the anterior vaginal wall. A small window is made in the retropubic space at the mid to distal urethra. A suburethral tunnel is created in the anterior vaginal wall 1.5 cm from the urethral meatus by using a fine tip right angle clamp. The sling is then transferred beneath the suburethral tunnel. A small puncture is made suprapubically, and a double-pronged needle is passed under finger control through the fascia and retropubic space.
The previously placed polyglactin sutures from the polypro- pylene mesh are transferred to the suprapubic incision.
Cystoscopy is then performed to rule out bladder or urethral perforation. An Allis clamp is placed through each vaginal incision to firmly hold the sling in the horizontal position, while the assistant ties the polyglactin sutures suprapubically. Finally, the vaginal and suprapubic incisions are closed.
2) Canal TOT: Two oblique lateral incisions are made in the anterior vaginal wall. A suburethral tunnel is created in the anterior vaginal wall 1.5 cm from the urethral meatus by using
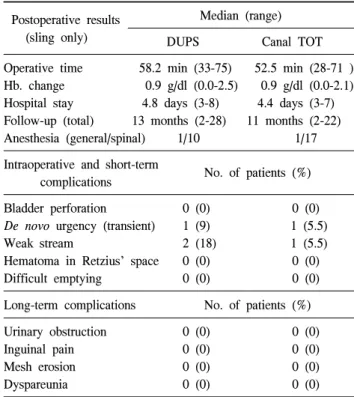
Table 2. Operative data Postoperative results
(sling only)
Median (range)
DUPS Canal TOT
Operative time 58.2 min (33-75) 52.5 min (28-71 ) Hb. change 0.9 g/dl (0.0-2.5) 0.9 g/dl (0.0-2.1) Hospital stay 4.8 days (3-8) 4.4 days (3-7) Follow-up (total) 13 months (2-28) 11 months (2-22)
Anesthesia (general/spinal) 1/10 1/17
Intraoperative and short-term
No. of patients (%) complications
Bladder perforation 0 (0) 0 (0)
De novo urgency (transient) 1 (9) 1 (5.5)
Weak stream 2 (18) 1 (5.5)
Hematoma in Retzius' space 0 (0) 0 (0)
Difficult emptying 0 (0) 0 (0)
Long-term complications No. of patients (%)
Urinary obstruction 0 (0) 0 (0)
Inguinal pain 0 (0) 0 (0)
Mesh erosion 0 (0) 0 (0)
Dyspareunia 0 (0) 0 (0)
DUPS: distal urethral polypropylene sling, TOT: transobturator tape Table 1. Preoperative patient characteristics
Patient characteristics DUPS (11)
Canal TOT (18) Median age (range)
No. with prior hysterectomy (%) No. with prior vaginal delivery (mean)
74 (70-81) 2/11 (18%) 3-6 (3.8)
73 (70-79) 3/18 (17%) 2-8 (4.2)
DUPS: distal urethral polypropylene sling, TOT: transobturator tape
a fine tip right angle clamp. The sling is transferred beneath the suburethral tunnel. Further stab incisions are made in the genito-crural fold at the level of the clitoris in both sides. The index finger guides the helical tunneller tip from the incision made at the genito-crural fold to the incision made at the anterior vaginal wall. Polypropylene tape is then attached to the tunneller and brought back through the created passage.
Cystoscopy is then performed to check the integrity of the urethra and the bladder.
2. Statistical analysis
Data are expressed as medians (range) or Means±SD. The paired t-test was used to compare the preoperative and postoperative scores on the IIQ-7 and UDI-6. p-values<0.05 were considered statistically significant. All statistical analyses were performed by using SAS Version 9.1 (SAS Institute Inc., Cary, NC, USA).
RESULTS
Eleven patients underwent the DUPS procedure, and 18 patients underwent the canal TOT procedure to treat SUI. Table 1 summarizes the preoperative demographic characteristics of the enrolled patients. There were no statistically significant differences between the groups. No patient had a history of prior anti-incontinence surgery. There were no significant differences in previous surgical history.
Table 2 lists the operative data, surgical outcomes, peri- operative complications, and long-term postoperative compli- cations. There were no major long-term complications after a minimum follow-up of 2 months (DUPS group: median 13 months, range 2-28 months; canal TOT group: median 11 months, range 2-22 months), including mesh erosion, urinary obstruction, or persistent suprapubic pain.
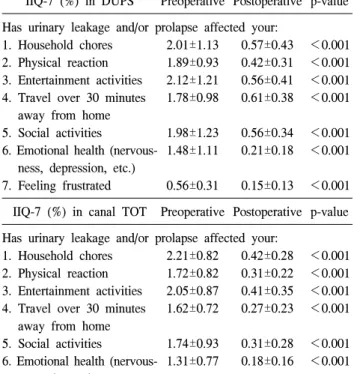
The median operative times were 58.2 min (range, 33-75 min) and 52.5 min (range, 28-72 min) in the DUPS and canal TOT groups, respectively. When assessing the perioperative complications, we evaluated all available patients who under- went the DUPS and canal TOT procedures. All reported complications appeared in the short term and ceased soon thereafter. No patients incurred bladder injury (one patient in each group had brief de novo urgency, which resolved after several days). Table 3 and 4 show the results of the pre- operative and postoperative UDI-6 and IIQ-7 assessments.
Postoperatively, the mean IIQ-7 urinary symptom scores in the DUPS and canal TOT groups were 0.44 and 0.30, respectively, compared with 1.69 and 1.59 preoperatively. The postoperative mean UDI-6 scores in the DUPS and canal TOT groups were 0.25 and 0.31, respectively, compared with 1.63 and 1.49 preoperatively. Regarding both questionnaires, 82% of patients reported no symptoms of SUI under any circumstances, and 91% of patients reported rarely or never being bothered by SUI.
The subjective patient satisfaction after surgery was rated as satisfactory, and there were no significant differences between the two groups in this regard.
Table 3. Results of preoperative and postoperative Incontinence Impact Questionnaire (IIQ)-7 in patients undergoing DUPS and canal TOT
IIQ-7 (%) in DUPS Preoperative Postoperative p-value Has urinary leakage and/or prolapse affected your:
1. Household chores 2. Physical reaction 3. Entertainment activities 4. Travel over 30 minutes
away from home 5. Social activities
6. Emotional health (nervous- ness, depression, etc.) 7. Feeling frustrated
2.01±1.13 1.89±0.93 2.12±1.21 1.78±0.98 1.98±1.23 1.48±1.11 0.56±0.31
0.57±0.43 0.42±0.31 0.56±0.41 0.61±0.38 0.56±0.34 0.21±0.18 0.15±0.13
<0.001
<0.001
<0.001
<0.001
<0.001
<0.001
<0.001 IIQ-7 (%) in canal TOT Preoperative Postoperative p-value Has urinary leakage and/or prolapse affected your:
1. Household chores 2. Physical reaction 3. Entertainment activities 4. Travel over 30 minutes
away from home 5. Social activities
6. Emotional health (nervous- ness, depression, etc.) 7. Feeling frustrated
2.21±0.82 1.72±0.82 2.05±0.87 1.62±0.72 1.74±0.93 1.31±0.77 0.52±0.47
0.42±0.28 0.31±0.22 0.41±0.35 0.27±0.23 0.31±0.28 0.18±0.16 0.21±0.08
<0.001
<0.001
<0.001
<0.001
<0.001
<0.001
<0.001 DUPS: distal urethral polypropylene sling, TOT: transobturator tape
Table 4. Results of preoperative and postoperative Urogenital Distress Inventory (UDI)-6 in patients undergoing DUPS and canal TOT
UDI-6 (%) in DUPS Preoperative Postoperative p-value Do you experience, and, if so, how much are you bothered by:
1. Frequent urination 2. Leakage related to feeling
of urgency
3. Leakage related to activity, coughing, or sneezing 4. Small amounts of leakage
(drops)
5. Difficulty emptying bladder 6. Pain or discomfort in lower
abdominal or genital area
1.78±1.12 0.62±0.48 2.89±0.82 1.92±1.01 1.75±0.92 0.81±0.52
0.37±0.33 0.35±0.28 0.21±0.14 0.20±0.18 0.23±0.21 0.14±0.12
<0.001
<0.001
<0.001
<0.001
<0.001
<0.001
IIQ-7 (%) in canal TOT Preoperative Postoperative p-value Do you experience, and, if so, how much are you bothered by:
1. Frequent urination 2. Leakage related to feeling
of urgency
3. Leakage related to activity, coughing, or sneezing 4. Small amounts of leakage
(drops)
5. Difficulty emptying bladder 6. Pain or discomfort in lower
abdominal or genital area
1.72±1.03 0.63±0.57 2.54±0.55 1.75±1.15 1.62±0.97 0.71±0.65
0.43±0.22 0.35±0.28 0.28±0.07 0.41±0.40 0.26±0.21 0.12±0.10
<0.001
<0.001
<0.001
<0.001
<0.001
<0.001
DUPS: distal urethral polypropylene sling, TOT: transobturator tape
DISCUSSION
The etiology of SUI is still not completely understood.
Therefore, its treatment remains controversial. In the past, bladder neck suspension was widely performed to correct anatomical abnormalities of the bladder neck and urethral hypermobility [15]. These procedures were initially appealing because of their simplicity, low morbidity, and excellent early success [16]. However, in the long term, the success of these procedures proved to wane, and the need for alternative surgical procedures arose [17]. Pubovaginal slings have gained worldwide popularity because of their effectiveness, with an associated cure rate of 83% after 4 years [18]. Nevertheless, pubovaginal slings are associated with higher morbidity and longer convalescence compared with other vaginal procedures [19]. In addition, they are associated with a higher rate of postoperative voiding dysfunction [18]. For these reasons, surgeons continue to search for less invasive procedures that can provide similar or superior outcomes with lower morbidity.
Past surgical procedures have targeted the proximal urethra and bladder neck by elevating the bladder neck to an intra-abdominal position, fixing the proximal urethra to the pubic bone, or increasing proximal urethral resistance. How- ever, Minaglia et al found that correction of proximal urethra mobility was not required to cure SUI [20]. The use of slings in the mid-urethra has broadened our understanding of urethral support and the mechanism of continence. The TVT procedure has been shown to be effective for SUI [4]. However, the TVT technique is a blind approach without finger guidance, which creates an elevated risk for bladder perforation, bowel injury, major vessel injury, and even death [6]. Therefore, several modifications of the original TVT procedure have been developed.
Modified procedures support the distal urethra through a different mechanism. Anatomically, distally placed suburethral slings bring the urethra closer to the pubic bone and provide posterior support. The proximity of the urethra to the symphysis
pubis allows for more efficient impact of the levator mus- culature on the urethra at the time of increased intra-abdominal pressure. DUPS, originally described by Rodriguez and Raz, is a characteristic approach that re- establishes distal urethral support and does not carry the morbidity of autologous fascia harvesting or the expense of mid-urethral sling kits [21]. The distal suburethral sling brings the urethra closer to the pubic bone. Therefore, distal sling procedures leave the mid and proximal urethra and bladder neck as is. Lee et al performed another DUPS study in Korean women and showed that this procedure is safe and effective for treating SUI [12].
Even newer mid-urethral sling procedures have been introduced. The transobturator mid-urethral sling (TOMUS) was developed to avoid the potential vascular and bladder injury associated with blind retropubic passage of the TVT trocars [10,11]. There are two type of mesh insertion: outside-in and inside-out, which both method produce similar excellent treatment results [22]. Canal transobturator tape (Canal TOT) was developed to reduce the complications of TOT (especially de novo urgency) by modifying the sling procedure of TOT with using a distal urethral polypropylene sling [13]. Canal TOT makes two oblique lateral incisions in the anterior vaginal wall. Double incisions allow for easy manipulation of the mesh in the anterior vaginal submucosal tunnel; therefore, voiding dysfunction can be minimized postoperatively. De novo urgency is the most common long-term complication seen after SUI correction using existing surgical methods [23,26,27].
Bladder neck elevation is thought to be a contributing factor.
Our study proceeded on the assumption that postoperative voiding dysfunction was due to proximal migration of midurethral sling and bladder irritation by midurethral sling.
Therefore, our surgical techniques (DUPS and canal TOT) might help to explain the differences in the frequency of de novo urgency between patients undergoing our surgical pro- cedure (5.5-9%) and those undergoing TVT (15%) [23], although our study sample size and follow-up period were insufficient.
DUPS and canal TOT have several points of similarity. Both have double vaginal incisions, use the same material (woven polypropylene) for the sling mesh, entail suburethral tunnel formation, support the distal to mid urethra, do not require special instrumentation, and are simple to perform with an average operative time of about 50 minutes. The polypropylene synthetic mesh used for the urethral sling material is durable,
inert, resistant to infection, and flexible and has good tensile strength and does not soak up water. Recently, however, a few reports have noted a high vaginal erosion rate with ObTapeTM and UraTapeTM. Domingo et al found an unexpectedly high rate of erosion using the UraTape/ObTape transobturator system [24]. Yamada et al reported an erosion rate of 13.4% with ObTape compared with 0% reported for Monarc [25]. This increased rate of erosion is thought to occur secondary to the non-knitted, non-woven nature of the mesh material and not secondary to the transobturator technique. We used a knitted and woven type polypropylene mesh for our procedures.
Ultimately, the question is, how efficacious are the DUPS and canal TOT procedures in elderly SUI patients? Lee et al have already shown that Canal TOT procedure produced excellent treatment results with minimal postoperative complications regardless of age [13]. Reportedly, human aging causes gradual changes in bladder structure and behavior.
Specifically, there are modifications in urethral sphincteric innervation, with a gradual decrease in the maximum sphincteric closure pressure. Female senility is thought to be responsible for modifications in the vesical constrictor system level, resulting clinically in the bladder hyperactivity that is frequently associated with SUI and bladder hypocontractility.
Therefore, the aging process and subsequent modifications in bladder structure and urethral sphincter behavior suggest that the sling operation might have higher morbidity, post operative voiding dysfunction rateand lower efficiency when used in elderly women. In the Gordon’s study of tension-free vaginal tape outcomes, de novo urge incontinence was significantly more common in women aged 70 and older than in women younger than 70 (18% vs. 4%) [26]. The findings of Anger’s study are also similar to those of another study [13], which found that postoperative urgency symptoms after mid-urethral sling surgery were more prevalent in women aged 65 and older than in women aged 45 to 64 (25.0% vs. 6.3%) [27]. So it is generally accepted that aging is a factor predisposing to voiding dysfunction after anti- incontinence surgery. Several reports have shown slightly to moderately unfavorable treatment results and postoperative morbidities in very old women who have undergone TVT surgery for SUI [28-30]. Hellberg et al reported that the cure rate after TVT surgery performed for
“any” type of incontinence in patients over 75 years of age was 55.7% [28]. Sevestre et al reported that 67% of patients had no more incontinence episodes at the time of the final
follow-up visit [29]. Allahdin et al suggested that postoperative complications of urgency and vaginal wall erosion were more common in older patients [30].
We wanted to establish the efficacy of double incisions at the mid to distal urethral level with additional tension adjustment of the mesh. We also wanted to know the rate of satisfaction in patients over 70 years of age who underwent these procedures. We created a suburethral tunnel that had enough space for the mesh to pass through. We expected that the suburethral tunnel would contribute to the incorporation of the mesh into the surrounding tissue and would therefore diminish the rate of postoperative vaginal erosion by the mesh.
In our study, 82% of the patients had no symptoms of SUI under any circumstances, and 91% of the patients said that they were rarely or never bothered by SUI. There were no major long-term complications, including vaginal erosion, after a minimum follow-up period of 2 months (DUPS group: range, 2-28 months; canal TOT group: range, 2-22 months). Hence, we regard our modified procedure (DUPS and canal TOT) as safe and effective for the treatment of SUI in elderly women.
We have got much difficulties about suburethral tunneling and helical tunneller guidance through the genito-crural fold due to old women’s atrophied vaginal wall and hip joint contracture.
So our mean operation time for aged patients was comparatively longer (DUPS group: 74 min/Canal TOT group:
73 min) than other studys (Lee’s study [12] for DUPS: 29.4 min/Lee’s study [13] for Canal TOT: 22.4 min).
CONCLUSIONS
In this study, we showed that surgical outcomes and subjective assessments after DUPS and canal TOT are satisfactory in elderly patients being treated for SUI. The DUPS and canal TOT represent safe and effective alternative surgical techniques for treatment of SUI in elderly patients. We also showed that these procedures have lower associated morbidity than do other existing TVT or TOT procedures. Meanwhile, we are conscious of the fact that our series may be too small to detect such a low level of complications, and therefore further large-scale clinical trials are needed to prove the safety and durability of these procedures.
REFERENCES
1. Abrams P, Cardozo L, Fall M, Griffiths D, Rosier P, Ulmsten U, et al. The standardisation of terminology of lower urinary tract function: report from the Standardisation Sub-committee of the International Continence Society. Am J Obstet Gynecol 2002;187:116-26.
2. Ulmsten U, Petros P. Intravaginal slingplasty (IVS): an ambulatory surgical procedure for treatment of female urinary incontinence. Scand J Urol Nephrol 1995;29:75-82.
3. Olsson I, Kroon U. A three-year postoperative evaluation of tension-free vaginal tape. Gynecol Obstet Invest 1999;48:
267-9.
4. Nilsson CG, Kuuva N, Falconer C, Rezapour M, Ulmsten U.
Long-term results of the tension-free vaginal tape (TVT) procedure for surgical treatment of female stress urinary incontinence. Int Urogynecol J Pelvic Floor Dysfunct 2001;
12(Suppl 2):S5-8.
5. Meschia M, Pifarotti P, Bernasconi F, Guercio E, Maffiolini M, Magatti F, et al. Tension-free vaginal tape: analysis of outcomes and complications in 404 stress incontinent women.
Int Urogynecol J Pelvic Floor Dysfunct 2001;12(Suppl 2):
S24-7.
6. Kuuva N, Nilsson CG. A nationwide analysis of complications associated with the tension-free vaginal tape (TVT) procedure.
Acta Obstet Gynecol Scand 2002;81:72-7.
7. Moran P, Ward KL, Johnson D, Smirni WE, Hilton P, Bibby J. Tension-free vaginal tape for primary genuine stress incon- tinence: a two-centre follow-up study. BJU Int 2000;86:39-42.
8. Leboeuf L, Tellez CA, Ead D, Gousse AE. Complication of bowel perforation during insertion of tension-free vaginal tape.
J Urol 2003;170:1310.
9. Zilbert AW, Farrell SA. External iliac artery laceration during tension-free vaginal tape procedure. Int Urogynecol J Pelvic Floor Dysfunct 2001;12:141-3.
10. Delorme E. Transobturator urethral suspension: mini-invasive procedure in the treatment of stress urinary incontinence in women. Prog Urol 2001;11:1306-13.
11. Latthe PM, Foon R, Toozs-Hobson P. Transobturator and retropubic tape procedures in stress urinary incontinence: a systematic review and meta-analysis of effectiveness and complications. BJOG 2007;114:522-31.
12. Lee JH, Kim KH, Lee HW, Kim KH, Choi JS, Yoon SJ, et al. Distal urethral polypropylene sling surgical management for urodynamic stress incontinence in Korean women. Urol Int 2009;82:191-5.
13. Lee SH, Kim TB, Kim KH, Jung H, Lee MS, Yoon SJ.
Preliminary report on a modified surgical technique using canal transobturator tape for the treatment of female stress urinary incontinence. Korean J Urol 2008;49:1119-24.
14. Uebersax JS, Wyman JF, Shumaker SA, McClish DK, Fantl JA. Short forms to assess life quality and symptom distress for urinary incontinence in women: the Incontinence Impact Questionnaire and the Urogenital Distress Inventory. Continence Program for Women Research Group. Neurourol Urodyn 1995;14:131-9.
15. Marshall VF, Marchetti AA, Krantz KE. The correction of stress incontinence by simple vesicourethral suspension. Surg Gynecol Obstet 1949;88:509-18.
16. Ward KL, Hilton P. A prospective multicenter randomized trial of tension-free vaginal tape and colposuspension for primary urodynamic stress incontinence: two-year follow-up. Am J Obstet Gynecol 2004;190:324-31.
17. Glazener CM, Cooper K. Bladder neck needle suspension for urinary incontinence in women. Cochrane Database Syst Rev 2002;2:CD003636.
18. Leach GE, Dmochowski RR, Appell RA, Blaivas JG, Hadley HR, Luber KM, et al. Female Stress Urinary Incontinence Clinical Guidelines Panel summary report on surgical manage- ment of female stress urinary incontinence. The American Urological Association. J Urol 1997;158:875-80.
19. Tunuguntla HS, Gousse AE. Missed bilateral bladder per- foration during pubovaginal sling procedure. J Urol 2004;172:
189-90.
20. Minaglia S, Ozel B, Hurtado E, Klutke CG, Klutke JJ. Effect of transobturator tape procedure on proximal urethral mobility.
Urology 2005;65:55-9.
21. Rodriguez LV, Raz S. Polypropylene sling for the treatment of stress urinary incontinence. Urology 2001;58:783-5.
22. Houwert RM, Renes-Zijl C, Vos MC, Vervest HA. TVT-O
versus Monarc after a 2-4-year follow-up: a prospective comparative study. Int Urogynecol J Pelvic Floor Dysfunct 2009; Epub ahead of print
23. Levin I, Groutz A, Gold R, Pauzner D, Lessing JB, Gordon D. Surgical complications and medium-term outcome results of tension-free vaginal tape: a prospective study of 313 consecutive patients. Neurourol Urodyn 2004;23:7-9.
24. Domingo S, Alama P, Ruiz N, Perales A, Pellicer A.
Diagnosis, management and prognosis of vaginal erosion after transobturator suburethral tape procedure using a nonwoven thermally bonded polypropylene mesh. J Urol 2005;173:1627-30.
25. Yamada BS, Govier FE, Stefanovic KB, Kobashi KC. High rate of vaginal erosions associated with the mentor ObTape.
J Urol 2006;176:651-4.
26. Gordon D, Gold R, Pauzner D, Lessing JB, Groutz A.
Tension-free vaginal tape in the elderly: Is it a safe procedure?
Urology 2005;65:479-82.
27. Anger JT, Litwin MS, Wang Q, Pashos CL, Rodriguez LV.
The effect of age in outcomes of sling surgery for urinary incontinence. J Am Geriatr Soc 2007;55:1927-31.
28. Hellberg D, Holmgren C, Lanner L, Nilsson S. The very obese woman and the very old woman: tension-free vaginal tape for the treatment of stress urinary incontinence. Int Urogynecol J Pelvic Floor Dysfunct 2007;18:423-9.
29. Sevestre S, Ciofu C, Deval B, Traxer O, Amarenco G, Haab F. Results of the tension-free vaginal tape technique in the elderly. Eur Urol 2003;44:128-31.
30. Allahdin S, McKinley CA, Mahmood TA. Tension-free vaginal tape: a procedure for all ages. Acta Obstet Gynecol Scand 2004;83:937-40.