REVIEW ARTICLE
*Equal contribution
Received: April 20, 2020, Revised: May 8, 2020, Accepted: May 19, 2020
Corresponding author: Wah Yang, 613 Huangpu Avenue, Guangzhou 510630, China
Department of Metabolic and Bariatric Surgery, The First Affiliated Hospital of Jinan University Tel: +86-20-38688735, E-mail: yangwah@qq.com; yangwah@connect.hku.hk
Corresponding author: Xiaomei Chen, 613 Huangpu Avenue, Guangzhou 510630, China
Department of Metabolic and Bariatric Surgery, The First Affiliated Hospital of Jinan University Tel: +86-20-38688735, E-mail: 749818530@qq.com
CC
This is an open access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
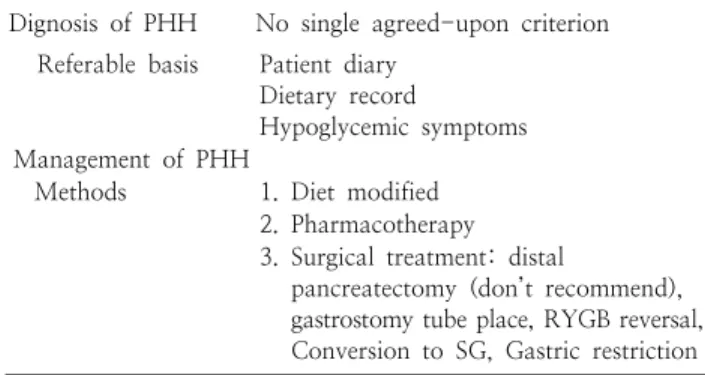
Hyperinsulinemic Hypoglycemia after Bariatric Surgery
1