Cutaneous Biophysical Characteristics of
Melasma
by
Dong Jun Lee
Major in Medicine
Department of Medical Sciences
The Graduate School, Ajou University
Cutaneous Biophysical Characteristics of
Melasma
by
Dong Jun Lee
A Dissertation Submitted to The Graduate School of Ajou
University in Partial Fulfillment of the Requirements for the
Degree of Master of Medicine
Supervised by
Hee Young Kang, M.D., Ph.D.
Major in Medicine
Department of Medical Sciences
The Graduate School, Ajou University
This certifies that the dissertation
of Dong Jun Lee is approved.
SUPERVISORY COMMITTEE
Hee Young Kang
Eun-So Lee
You Chan Kim
The Graduate School, Ajou University
June 23rd, 2011
감사의 글
본 논문의 시작에서 끝까지 물심 양면으로 도움을 주시고 지도와 조언을 아끼지 않으셨던 지도 교수이신 강희영 교수님께 깊은 감사를 드립니다. 또한 좋은 연구를 할 수 있도록 부족한 제가 많은 가르침을 주시고 격려를 주신 이은소 교수님과 김유찬 교수님께도 깊은 감사의 마음을 전합니다. 그리고 연구 기간 동안 도움을 주신 피부 과학 교실의 모든 선생님들과 실험 여러 과정을 도와주신 IEC Korea Skin Research Center 하재현 선생님, 이정옥 선생님과 조직 염색과 분석을 도와주신 김영배 선생님께 감사 드립니다. 언제나 아낌 없는 사랑으로 지원해 주시는 부모님, 가족들에게도 감사의 마음을 전합니다.2011 년 6 월 저자씀
i
- ABSTRACT-
Cutaneous Biophysical Characteristics of Melasma
Background: Melasma is characterized by increased pigmentation and photodamaged
skin. These features suggest that melasma patients might have a significant impact on cutaneous biophysical characteristics.
Objective: The cutaneous biophysical characteristics in melasma were investigated. Methods: A total of 16 Korean volunteers with melasma were enrolled. The melanin
index/erythema index, stratum corneum (SC) hydration, sebum content, and transepidermal water loss (TEWL) were measured and compared between lesional and perilesional normal skin. The TEWL was re-measured immediately and 5 hours after tape stripping to investigate SC integrity and barrier recovery rate. The sebum content was measured at 30 minutes and 5 hours after degreasing by facial washing to estimate the sebum excretion rate. Skin biopsy was performed in 11 volunteers to measure the SC thickness and to study the expression of lipid metabolism associated genes such as
peroxisome proliferator-activated receptor alpha (PPAR-α), and arachidonate 15-lipoxygenase, type B (ALOX15B).
Results: The melanin index, erythema index, and SC hydration were significantly higher
in lesional skin compared to nonlesional skin, whereas the measurement of basal TEWL showed no significant difference. However, the increased rate of TEWL after tape-stripping was significant higher in lesional skin compared to nonlesional skin. Also,
barrier recovery rate of lesional skin was significant delayed. The melanin index was found to be inversely correlated with the barrier recovery rate. There was no significant difference between the basal sebum content and the sebum excretion rate. The expression between PPAR-α and ALOX15B was not significantly different, whereas SC thickness was reduced in lesional skin, which showed correlation with the barrier recovery rate.
Conclusions: Melasma skin showed a normal hydration state and sebaceous gland
activity. However, the SC integrity and barrier function were impaired in lesional skin of melasma. The SC thickness was reduced in lesional skin, and it positively correlated with the barrier recovery rate. These results suggest that improving SC function should be considered in treating melasma.
Keywords: Melasma, Stratum corneum, Barrier function, TEWL
iii
TABLE OF CONTENTS
ABSTARCT ··· i
TABLE OF CONTENTS ··· iii
LIST OF FIGURES ··· iv
LIST OF TABLES ··· v
I. INTRODUCTION ··· 1
II. MATERIALS AND METHODS ··· 3
A. Subjects ··· 3
B. Measurement of biophysical properties ··· 5
C. Measurement of stratum corneum thickness and immunohistochemistry ··· 5
D. Statistical analysis ··· 6
III. RESULTS ··· 8
A. Melanin index and erythema index ··· 8
B. Basal stratum corneum properties ··· 10
C. Epidermal permeability barrier function ··· 11
D. Sebum content ··· 13
E. Expressions of PPAR-α and ALOX15B and SC thickness ··· 14
IV. DISCUSSION ··· 17
V. CONCLUSION ··· 22
REFERENCES ··· 23
LIST OF FIGURES
Fig. 1. Melanin/Erythema index ··· 8
Fig. 2. Stratum corneum capacitance ··· 10
Fig. 3. Basal TEWL ··· 11
Fig. 4. Barrier recovery rate ··· 12
Fig. 5. Correlation between melanin index and barrier recovery rate ··· 13
Fig. 6. Sebum contents ··· 14
Fig. 7. Expressions of PPAR-α and ALOX15B and stratum corneum thickness ··· 15
v
LIST OF TABLES
I. INTRODUCTION
Melasma is a common acquired hyperpigmentary disorder characterized by irregular light to dark brown macules and patches on sun-exposed skin.(Kang et al., 2002) A major histopathological feature of melasma is an increased epidermal pigmentation. Melanin is concentrated in the basal layer but also distributed throughout the epidermis. It has been thought that skin pigmentation is associated with multiple cutaneous functions. Stratum corneum (SC) in black skin contains more cell layers and greater electrical resistance and requires more tape strips to remove it than that of white skin, suggesting better intercellular cohesion in black skin.(Berardesca and Maibach, 1996) Moreover, epidermal barrier function is different between blacks and white skin, although the results are inconclusive. Darker skin has been shown to recover faster after barrier damage.(Reed et al., 1995) Whereas, Kompaore et al.(Kompaore et al., 1993) found significant higher transepidermal water loss (TEWL) after stripping in blacks and Asians than in whites. These findings suggest that lesional skin of melasma may have different biophysical characteristics compare to non-lesional skin.
Additional distinguishing histological characteristics of melasma are the features of photodamaged skin. It is reported that Melasma lesions show a higher degree of UV-induced damage, like solar elastosis and increased vascularity.(Kang et al., 2002; Kim et al., 2007; Hernandez-Barrera et al., 2008) Photodamaged skin has been thought to have modified cutaneous functions. Barrier recovery is delayed in photoaged skin as compared to chronologically aged skin.(Reed et al., 1997) Moreover, recently we found that most lipid
2
-metabolism-associated genes such as peroxisome proliferator-activated receptor alpha
(PPARA) and arachidonate 15-lipoxygenase, type B (ALOX15B) were down-regulated,
accompanying a delayed barrier recovery rate in lesional skin.(Kang et al., 2011) These findings suggest that cutaneous biophysical characteristics may have a significant impact on melasma patients.
Therefore, in this study, I measured the cutaneous biophysical characteristics of melasma including SC hydration, sebum content, and TEWL and made comparisons between lesional and perilesional normal skin.
II. MATERIALS AND METHODS
A. Subjects
A total of 16 female Korean volunteers with melasma were recruited. The mean age was 44.2±5.36 years old (31-55 years old), and the average of disease duration was 12.9±7.2 years. All subjects have Fitzpatrick skin type III or IV. All subjects had a washout period of at least one month from a bleaching agent or steroid containing triple agents and a washout period of at least one year from lasers, dermabrasion, and chemical peeling. No skin care products had been applied to the measured sites 24 hours prior to the measurements, and the measured sites had not been washed with soaps or surfactants for at least two hours prior to the study. A two-millimeter punch biopsy from lesional and perilesional skin of melasma was performed in 11 of 16 volunteers. Informed written consent was obtained. This study was approved by the institutional review board of Ajou University Hospital (IRB number: AJIRB-MED-DEO-10-152).
4
-Table 1. General characteristics of volunteers Age Skin type Disease duration
(yrs)
Previous Medical history Skin biopsy
1 42 IV 30 None O 2 31 IV 2.3 None O 3 44 IV 5 None O 4 55 IV 20 None O 5 46 IV 23 None O 6 42 III 10 None X 7 46 III 15 None O 8 47 III 7 None X 9 51 III 18 None O 10 39 III 15 None X 11 44 III 20 None O
12 44 III 7 Anemia, Thyroid nodule X
13 43 III 10 None X
14 48 III 20 Diabetes mellitus O
15 46 IV 14 None O
B. Measurements of biophysical characteristics
The melanin/erythema index, SC hydration capacitance, TEWL and amount of sebum were measured on lesional and perilesional skin by respective probes (Mexameter: MX16®; Corneometer: CM825®; Tewameter: TM210®; Sebumeter: SM810®) connected to MPA-5® (Courage+Khazaka electronic GmbH, Köln, Germany). SC capacitance and melanin/erythema index were measured on the right side of the face, and the final value was expressed as the mean of three readings. TEWL was assessed on the left side of the face. After baseline measurement of TEWL, barrier perturbation was performed by 5 times repeated tape stripping (D-squame®) for barrier recovery rate measurement. TEWL was measured immediately and 5 hours after tape stripping. Sebum amount was measured at 30 minutes after facial washing and at 5 hours after degreasing to evaluate sebum excretion rate. All measurements were performed in an environmentally controlled research facility that maintained an ambient temperature at 22-24 and relative humidity of 50℃ -55%. All volunteers were allowed to acclimatize for 30 minutes prior to the test in order to adapt to the room conditions.
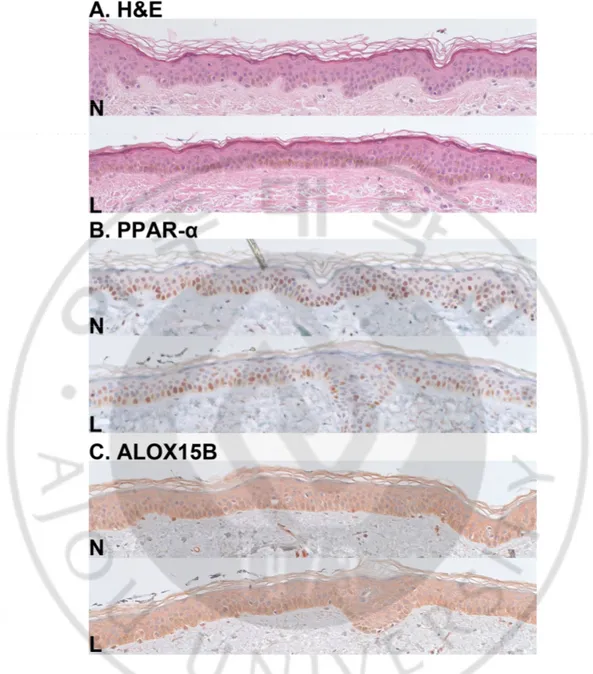
C. Measurement of stratum corneum thickness and immunohistochemistry
Hematoxylin and eosin staining was performed using standard protocols. Under H&E stain, digital images were captured (SPOT Flex®, SPOT Imaging Solutions, Sterling Heights, MI, USA) for estimating the area of SC and length of SC baseline. SC thickness was measured by the ratio of area and length of SC baseline.
6
-serial sectioned at 4.5μm and deparaffinized and rehydrated by sequential immersion in xylene, graded concentrations of ethanol. The deparaffinized tissue sections were incubated for 30 minutes at room temperature in a solution of 0.5% hydrogen peroxidase in methanol to quench endogenous peroxidase activity, followed by heated for 20 minutes with citrate buffer at pH 6.0 in a microwave or pretreated with trypsine for 10 minutes in 42 for ℃ antigen retrieval. After washing by Tris-buffered saline (TBS, 0.1mol/L, pH7.4, Dako, Carpinteria, CA), tissue sections were incubated with primary antibodies for 30 minutes at 38 . ℃ A monoclonal antibody to peroxisome proliferator-activated receptor-α (PPAR-α; Abcam, Cambridge, U.K.) and arachidonate 15-lipoxygenase, type B (ALOX15B, Lifespan Biosciences, Seattle, WA, USA) were used with 1:200 and 1:100 dilution respectively. After incubation with secondary antibody for 10 minutes, horseradish peroxidase (HRP) complex and AEC chromogen were added for 15 minutes and 20 minutes respectively, followed by, counterstaing was performed with hematoxylin. The image was analyzed using Image-Pro Plus Version 4.5 (Media Cybernetics co., Silver Spring, MD, USA).
D. Statistical analysis
The SPSS 14.0 statistics program (SPSS, Inc., Chicago, IL, USA) and the GraphPad Prism 5 software (GraphPad Software, Inc., La Jolla, CA, USA) was used for all statistical analysis. If the data showed normality distribution, the independent t-test was used to analyze the statistically significant difference between the melasma-involved and perilesional normal skin; if it does not, Mann-Whitney test was used. The relationship between each biophysical property was tested with Spearson correlation. A value of less than
0.05 was considered to be statistically significant. Data are expressed as mean ± standard deviation (SD).
8
-III. RESULTS
A. Melanin index and erythema index
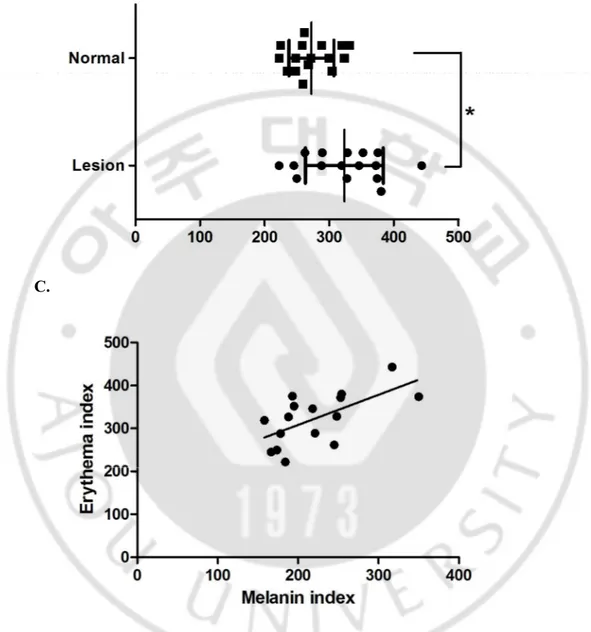
The melanin index was significantly higher in lesional skin than in perilesional normal skin (221.4±54.3 vs. 150.4±29.9, p<0.001; Fig 1A). The erythema index was significantly increased in lesional skin than perilesional normal skin (323.2±60.3 vs. 272.3±34.8, p<0.012; Fig 1B). The melanin and erythema index showed a positive correlation (Correlation coefficient: 0.703, p<0.01; Fig 1C).
B.
C.
Fig. 1. Melanin/Erythema index; Comparison of melanin/erythema index between lesional
skin and perilesional normal skin; A. Melanin index, B. Erythema index, C. Correlation between melanin/erythema index; Melanin index and erythema index showed positive correlation. (*p< 0.05)
- 10 -
B. Basal stratum corneum properties
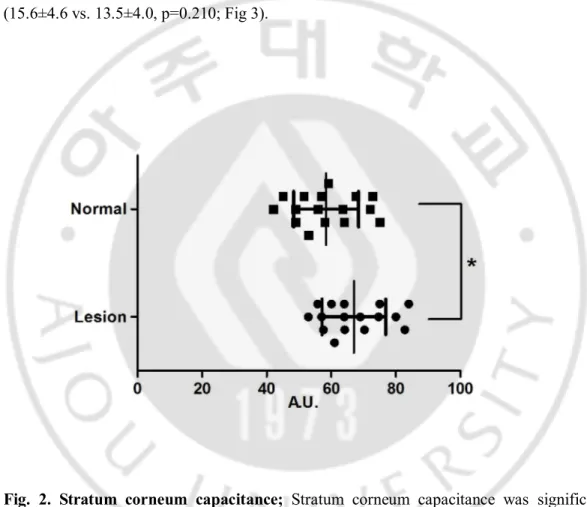
The SC hydration was significantly increased in lesional skin compared to perilesional normal skin (66.9±9.9 vs. 58.4±10.1; p<0.029; Fig.2). However, the basal TEWL showed no significant difference between lesional and perilesional normal skin (15.6±4.6 vs. 13.5±4.0, p=0.210; Fig 3).
Fig. 2. Stratum corneum capacitance; Stratum corneum capacitance was significantly
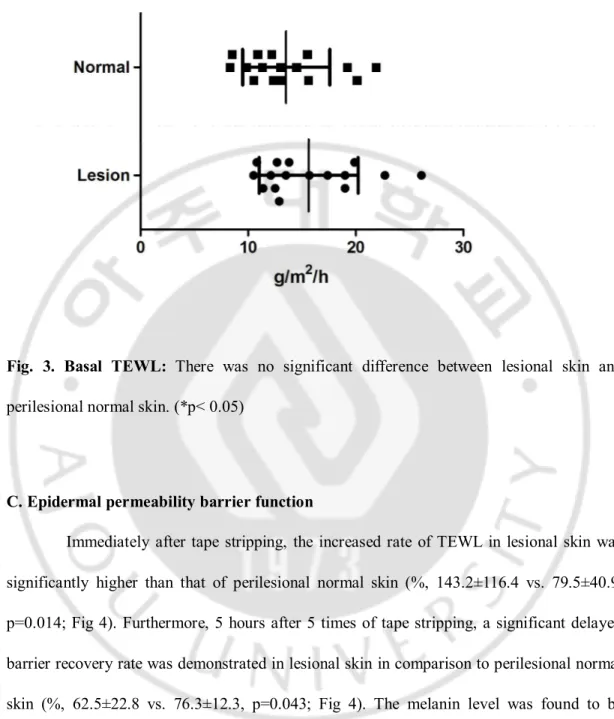
Fig. 3. Basal TEWL: There was no significant difference between lesional skin and
perilesional normal skin. (*p< 0.05)
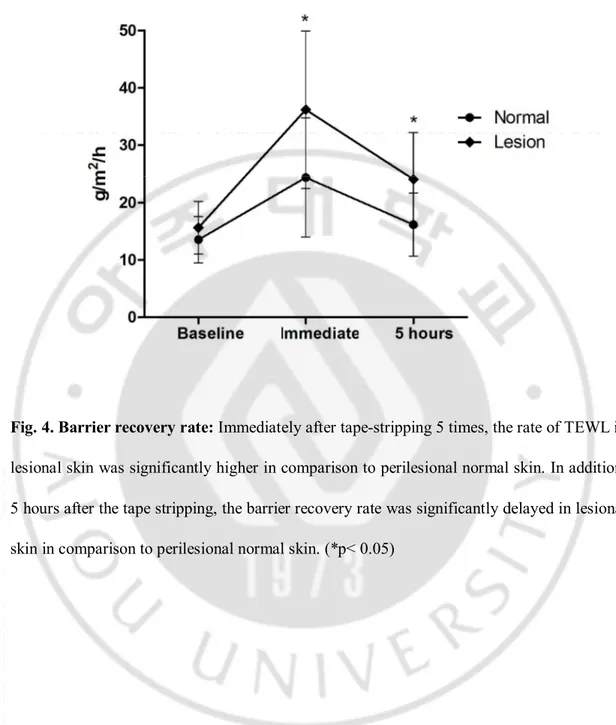
C. Epidermal permeability barrier function
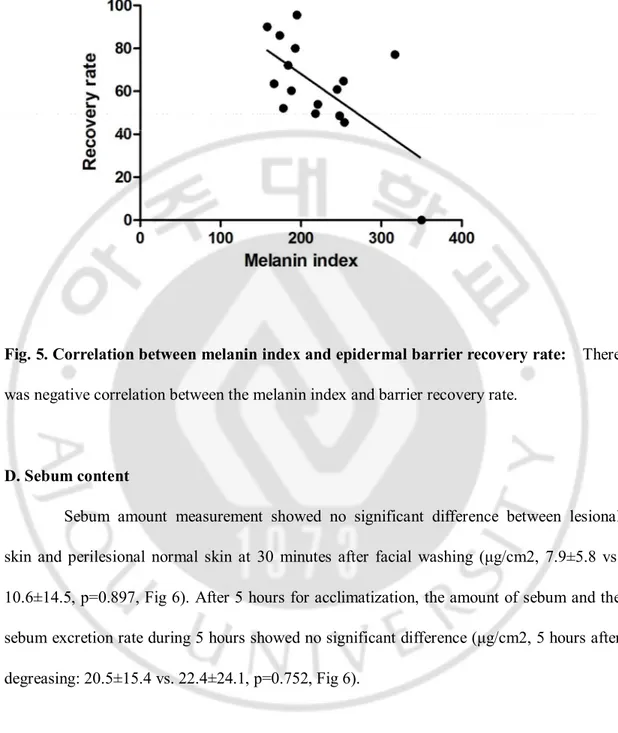
Immediately after tape stripping, the increased rate of TEWL in lesional skin was significantly higher than that of perilesional normal skin (%, 143.2±116.4 vs. 79.5±40.9, p=0.014; Fig 4). Furthermore, 5 hours after 5 times of tape stripping, a significant delayed barrier recovery rate was demonstrated in lesional skin in comparison to perilesional normal skin (%, 62.5±22.8 vs. 76.3±12.3, p=0.043; Fig 4). The melanin level was found to be inversely correlated with TEWL levels after tape stripping (Correlation coefficient: -0.503, p<0.05; Fig 5).
- 12 -
Fig. 4. Barrier recovery rate: Immediately after tape-stripping 5 times, the rate of TEWL in
lesional skin was significantly higher in comparison to perilesional normal skin. In addition, 5 hours after the tape stripping, the barrier recovery rate was significantly delayed in lesional skin in comparison to perilesional normal skin. (*p< 0.05)
Fig. 5. Correlation between melanin index and epidermal barrier recovery rate: There
was negative correlation between the melanin index and barrier recovery rate.
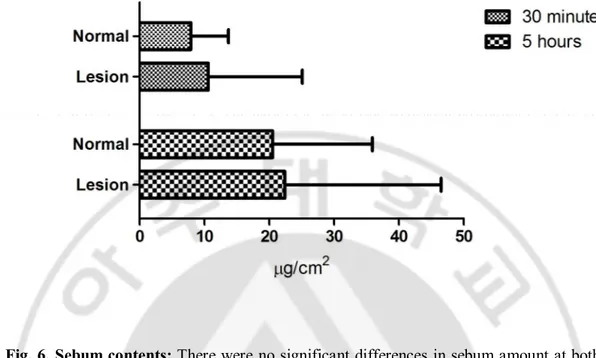
D. Sebum content
Sebum amount measurement showed no significant difference between lesional skin and perilesional normal skin at 30 minutes after facial washing (μg/cm2, 7.9±5.8 vs. 10.6±14.5, p=0.897, Fig 6). After 5 hours for acclimatization, the amount of sebum and the sebum excretion rate during 5 hours showed no significant difference (μg/cm2, 5 hours after degreasing: 20.5±15.4 vs. 22.4±24.1, p=0.752, Fig 6).
- 14 -
Fig. 6. Sebum contents: There were no significant differences in sebum amount at both 30
minutes and 5 hours after facial degreasing.
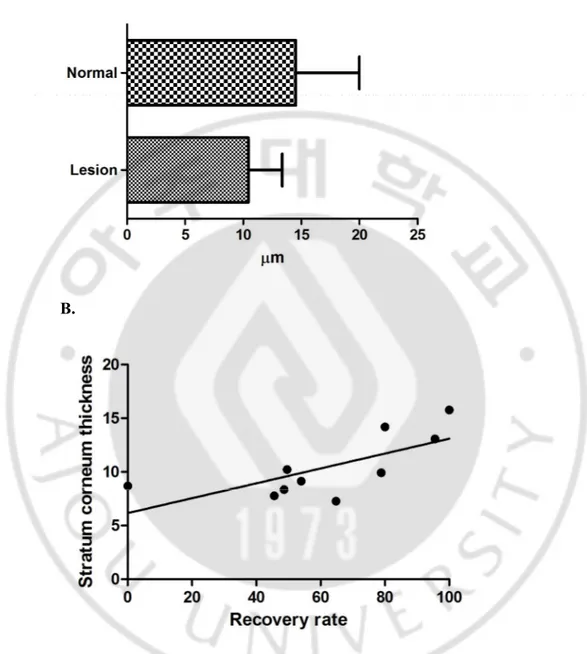
E. Expressions of PPAR-α and ALOX15B and SC thickness
Because lipid metabolism related genes, such as PPARA and ALOX15B were found to be down-regulated in melasma, we examined their protein levels.(Kang et al., 2011) There was no significant difference in immunoreactivity of PPAR-α and ALOX15B between lesional and perilesional normal skin (Fig 7). However, we found that the SC thickness was reduced in the lesional skin of melasma in comparison with perilesional normal skin (µm, 10.4±2.9 vs. 14.5±5.5, p=0.052, Fig 7, 8A). The SC thickness showed positive correlation with epidermal barrier recovery rate (Correlation coefficient: 0.721, p=0.02; Fig 8B)
Fig. 7. Expressions of PPAR-α and ALOX15B and stratum corneum thickness: A.
Stratum corneum thickness was lower in lesional skin compared to perilesional normal skin. B, C. There was no significant difference of PPAR-α and ALOX15B expression between lesional and perilesional normal skin. (N: perilesional normal skin, L: Lesional skin. original magnification x200)
- 16 -
A.
B.
Fig. 8. Stratum corneum thickness and correlation with barrier recovery rate; A. SC of
lesional skin showed reduced tendency in comparison with perilesional normal skin. B. SC thickness showed positive correlation between epidermal barrier recovery rate.
IV. DISCUSSION
The present study demonstrated that melasma skin showed a normal hydration state and sebaceous gland activity. However, the SC integrity and barrier function were impaired in the lesional skin of melasma. The SC thickness was reduced in lesional skin, and it correlated with the barrier recovery rate. The melanin index was also significantly related with delayed barrier recovery.
The mechanisms underlying abnormal barrier function in melasma are unclear, but there are possible explanations. Recently, we found the lipid metabolism-associated genes such as peroxisome proliferator-activated receptor alpha (PPARA), arachidonate
15-lipoxygenase, and type B (ALOX15B) were down-regulated in the lesional skin of melasma
(Kang et al., 2011). It is well known that the lipids of SC play an important role in maintaining cutaneous barrier homeostasis. PPAR-α is an important regulator of lipid catabolism, mediating fatty acid oxidation, fatty acid uptake, and lipoprotein assembly and transport.(Mao-Qiang et al., 2004) Therefore, down-regulated lipid metabolism-associated genes may be a causal factor of the impairment of epidermal barrier function in melasma, although we could not confirm the down-regulation of these proteins by
- 18 -
immnohistochemical staining. The reduced SC thickness may play another role in barrier impairment in lesional skin. In our study, reduced SC thickness was significantly related with delayed barrier recovery. SC thickness is correlated linearly to the 1/TEWL value (Weigmann et al., 2005). Furthermore, it has been reported that SC thickness is significantly correlated with the objective score of atopic dermatitis (Nemoto-Hasebe et al., 2009). Also, SC thickness is significantly decreased in acute eczematous atopic skin compared to non-lesional and control healthy skin (Voegeli et al., 2009). That means that SC thickness may influence the epidermal barrier homeostasis. Taken together, it is speculated that reduced SC thickness and down-regulation of lipid metabolism related genes in melasma affect the barrier function in melasma.
Chronic UV exposure may be another possible explanation for impaired barrier function in melasma. UV exposure is a major triggering or aggravating factor for melasma development. Indeed, previous studies have indicated that melasma lesions show a higher degree of UV-induced damage. Increased solar elastosis in lesional skin has been shown. It has also been shown that melasma is characterized by increased vasculature in the lesional skin both clinically and histologically (Voegeli et al., 2009). Expression of VEGF, a major
angiogenic factor of UV irradiated skin, is upregulated in melasma lesions compared to perilesional normal skin. In literature, chronic UV exposure influences cutaneous fatty acid metabolism and barrier function (Merle et al., 2010). Also, chronic UV irradiation reduces the epidermal free fatty acid and triglyceride synthesis that has an important role in epidermal barrier homeostasis (Kim et al., 2010). In addition, UVB exposure is detrimental to the epidermal permeability barrier in a dose- and time- dependent manner (Haratake et al., 1997). In photo-aged skin, barrier recovery is known to be significantly delayed (Reed et al., 1997). Therefore, an altered barrier function in melasma might be a result of the chronic UV exposure and accompanying epidermal hyperpigmentation. Interestingly, we found a negative correlation between melanin index and barrier recovery rate. It means that patients with severe melasma may have poor SC.
Very recently, it has been suggested that barrier function is influenced by pigmentation in the SC (Elias et al., 2009). Gunathilake et al. (Gunathilake et al., 2009) reported that skin type IV-V subjects have more acidic SC due to more melanosomes than pale-skinned subjects, and these acidic conditions were attributed to enhanced SC integrity and accelerated barrier recovery in darker skins (Bhatnagar et al., 1993; Puri et al., 2000).
- 20 -
Unfortunately, we did not measure the skin surface pH but the present study does not reveal a positive relationship between melanin index and barrier recovery rate. Rather, there was a negative correlation. These difference might be explained by the fact that molecules of melanin in melasma are different from normal melanin (Moncada et al., 2009). Especially, Raman skin spectroscopy measurements showed that melasma patients have degraded melanin in the SC of lesional skin. Of course, there are inter-individual differences in subjects’ race and geographic location.
The present study also demonstrated a significant increase of both the melanin and erythema index in melasma-involved skin. Also, a positive correlation appeared between the melanin index and the erythema index. The increased melanin index was reflected as the hallmark of melasma in histological studies such as epidermal hyperpigmentation (Kang et al., 2002). Furthermore, the increased erythema index in melasma-involved skin corresponded with the results of earlier studies, which reported that melasma patients showed higher erythema intensity and increased vascularity in the melasma lesions than that of perilesional normal skin (Kim et al., 2007). In a histopathologic study, the number of dermal vessels had a positive relationship with pigmentation in lesional skin (Kim et al.,
2007). These results have suggested that the connection between vessels and cutaneous pigmentation. It should be further studied on a large scale in the future.
- 22 -
V. CONCLUSION
In conclusion, in the present study, I have demonstrated that the melanin index, erythema index and SC hydration were significantly higher in lesional skin compared to perilesional normal skin. However, the basal TEWL and sebum excretion rate showed no significant difference. Interestingly, the epidermal barrier recovery in lesional skin is delayed, and SC integrity is decreased in lesional skin compared to perilesional normal skin. The melanin index showed to be inversely correlated with the barrier recovery rate. In histopathologically, SC thickness in lesional skin decreased than perilesional normal skin and correlated with the barrier recovery rate. These findings suggested that melasma skin have a normal hydration state and sebaceous gland activity, whereas the SC integrity and barrier function were impaired in melasma skin. Decreased SC integrity is one of major biophysical characteristic of melasma.
REFERENCES
1. Berardesca E, Maibach H: Racial differences in skin pathophysiology. J Am Acad
Dermatol 34: 667-672, 1996
2. Bhatnagar V, Anjaiah S, Puri N, Darshanam BN, Ramaiah A: pH of melanosomes of B 16 murine melanoma is acidic: its physiological importance in the regulation of melanin biosynthesis. Arch Biochem Biophys 307: 183-192, 1993
3. Elias PM, Menon G, Wetzel BK, Williams JJ: Evidence that stress to the epidermal barrier influenced the development of pigmentation in humans. Pigment Cell
Melanoma Res 22: 420-434, 2009
4. Gunathilake R, Schurer NY, Shoo BA, Celli A, Hachem JP, Crumrine D, Sirimanna G, Feingold KR, Mauro TM, Elias PM: pH-regulated mechanisms account for pigment-type differences in epidermal barrier function. J Invest Dermatol 129: 1719-1729, 2009
5. Haratake A, Uchida Y, Schmuth M, Tanno O, Yasuda R, Epstein JH, Elias PM, Holleran WM: UVB-induced alterations in permeability barrier function: roles for epidermal hyperproliferation and thymocyte-mediated response. J Invest Dermatol 108: 769-775, 1997
6. Hernandez-Barrera R, Torres-Alvarez B, Castanedo-Cazares JP, Oros-Ovalle C, Moncada B: Solar elastosis and presence of mast cells as key features in the pathogenesis of melasma. Clin Exp Dermatol 33: 305-308, 2008
- 24 -
7. Kang HY, Suzuki I, Lee DJ, Ha J, Reiniche P, Aubert J, Deret S, Zugaj D, Voegel JJ, Ortonne J-P: Transcriptional profiling shows altered expression of Wnt pathway- and lipid metabolism-related genes as well as melanogenesis-related genes in melasma. J Invest Dermatol in press, 2011
8. Kang WH, Yoon KH, Lee ES, Kim J, Lee KB, Yim H, Sohn S, Im S: Melasma: histopathological characteristics in 56 Korean patients. Br J Dermatol 146: 228-237, 2002
9. Kim EH, Kim YC, Lee ES, Kang HY: The vascular characteristics of melasma. J
Dermatol Sci 46: 111-116, 2007
10. Kim EJ, Jin XJ, Kim YK, Oh IK, Kim JE, Park CH, Chung JH: UV decreases the synthesis of free fatty acids and triglycerides in the epidermis of human skin in vivo, contributing to development of skin photoaging. J Dermatol Sci 57: 19-26, 2010 11. Kompaore F, Marty JP, Dupont C: In vivo evaluation of the stratum corneum barrier
function in blacks, Caucasians and Asians with two noninvasive methods. Skin
Pharmacol 6: 200-207, 1993
12. Mao-Qiang M, Fowler AJ, Schmuth M, Lau P, Chang S, Brown BE, Moser AH, Michalik L, Desvergne B, Wahli W, Li M, Metzger D, Chambon PH, Elias PM, Feingold KR: Peroxisome-proliferator-activated receptor (PPAR)-gamma activation stimulates keratinocyte differentiation. J Invest Dermatol 123: 305-312, 2004
13. Merle C, Laugel C, Baillet-Guffroy A: Effect of UVA or UVB irradiation on cutaneous lipids in films or in solution. Photochem Photobiol 86: 553-562, 2010
14. Moncada B, Sahagun-Sanchez LK, Torres-Alvarez B, Castanedo-Cazares JP, Martinez-Ramirez JD, Gonzalez FJ: Molecular structure and concentration of melanin in the stratum corneum of patients with melasma. Photodermatol
Photoimmunol Photomed 25: 159-160, 2009
15. Nemoto-Hasebe I, Akiyama M, Nomura T, Sandilands A, McLean WH, Shimizu H: Clinical severity correlates with impaired barrier in filaggrin-related eczema. J Invest
Dermatol 129: 682-689, 2009
16. Puri N, Gardner JM, Brilliant MH: Aberrant pH of melanosomes in pink-eyed dilution (p) mutant melanocytes. J Invest Dermatol 115: 607-613, 2000
17. Reed JT, Elias PM, Ghadially R: Integrity and permeability barrier function of photoaged human epidermis. Arch Dermatol 133: 395-396, 1997
18. Reed JT, Ghadially R, Elias PM: Skin type, but neither race nor gender, influence epidermal permeability barrier function. Arch Dermatol 131: 1134-1138, 1995 19. Voegeli R, Rawlings AV, Breternitz M, Doppler S, Schreier T, Fluhr JW: Increased
stratum corneum serine protease activity in acute eczematous atopic skin. Br J
Dermatol 161: 70-77, 2009
20. Weigmann HJ, Ulrich J, Schanzer S, Jacobi U, Schaefer H, Sterry W, Lademann J: Comparison of transepidermal water loss and spectroscopic absorbance to quantify changes of the stratum corneum after tape stripping. Skin Pharmacol Physiol 18: 180-185, 2005
- 26 - - 국문요약 -
기미의 피부 생물물리학적 특성
아주대학교 대학원의학과 이 동 준 (지도교수: 강 희 영) 연구배경: 기미는 피부 표피 색소 증가 및 광손상된 피부를 특징으로 하는 질환이다. 이런 기미의 조직학적 특징은 기미 환자에 있어서 피부 물리학적 특성의 변화를 야기시켰을 것으로 생각된다. 연구목적: 따라서 본 연구에서는 기미 병변에서의 피부 물리학적 특성을 인접 정상 피부와 비교하여 살펴보았다. 연구방법: 16 명 기미 환자를 모집하여 멜라닌 지수, 홍반 지수, 표피 수분량, 피지량, 경표피 수분 손실량을 기미 피부 병변과 인접 정상 피부에서 측정하였다. 경표피 수분 손실량의 경우 5 회 테이프 스트리핑 방법으로 피부 장벽에 손상을 가한 직후 및 5 시간 동안 피부 안정을 취한 후 재측정하여 각질층의 안정성 및 피부 장벽 회복 속도를 측정하였다. 피지량의 경우 물로 얼굴을 가볍게 세정한 이후 각각 30 분, 5 시간 동안 피부 안정을 취한 후 측정하였다. 11 명의 환자에서는 2mm punch 를 이용하여 병변 및 인접 정상 피부에서 피부 조직 검사를 시행하여 각질층 두게 및 지질 대사와 관련된 유전자인 peroxisomeproliferator-activated receptor alpha (PPAR-α), and arachidonate 15-lipoxygenase, type B (ALOX15B)의 면역조직화학염색을 시행하였다. 연구결과: 멜라닌 지수, 홍반 지수 및 피부 수분량은 인접 피부에 비해서 기미 병변에서 통계적으로 유의하게 증가한 반면 초기 경표피 수분 손실량은 기미와 정상 피부 사이에 통계적 유의한 차이는 보이지 않았다. 하지만 테이프 스트리핑 방법으로 피부 장벽에 손상을 가한 직후에 측정한 경표피 수분 손실량의 증가률은 기미 병변에서 인접 정상 피부에 피해 통계적 유의하게 증가되어 있었으며 5 시간 후 측정한 피부 장벽 회복률은 기미 병변이 인접 정상 피부에 비해 통계적 유의하게 감소하는 양상 관찰되었다. 또한 멜라닌 지수와 피부 장벽 회복 속도간에 음의 상관관계가 있는 것으로 나타났다. 기미 병변과 인접 정상 피부 사이에 피지량은 통계적 유의한 차이를 보이지 않았다. 피부 조직에서 PPAR-α 와 ALOX15B 의 발현은 기미와 정상 피부 사이에 차이를 보이지 않았으나 각질층의 두께는 기미 병변에서 감소되는 양상 관찰되었다. 또한 이 각질층의 두께는 장벽 회복 속도와 양의 상관관계가 있었다. 결론: 기미 병변은 정상적인 수분 함유량과 피지선 분비를 보였다. 하지만 각질층의 안정성 및 장벽 기능은 기미 병변이 인접 정상 피부에 비해 손상되어 있음을 확인할 수 있었다. 각질층의 두께는 기미 병변에서 감소되어 있었으며 이는 피부 장벽 회복 속도와 양의 상관관계가 있었다. 따라서 이 연구는 피부 장벽의 기능 회복 또한 기미의 치료에 있어서 고려해야 한다는 것을 제시하는 결과라 할 수 있다. 핵심어: 기미, 각질층, 피부 장벽 기능, 경표피 수분 손실량