저작자표시-비영리-동일조건변경허락 2.0 대한민국 이용자는 아래의 조건을 따르는 경우에 한하여 자유롭게 l 이 저작물을 복제, 배포, 전송, 전시, 공연 및 방송할 수 있습니다. l 이차적 저작물을 작성할 수 있습니다. 다음과 같은 조건을 따라야 합니다: l 귀하는, 이 저작물의 재이용이나 배포의 경우, 이 저작물에 적용된 이용허락조건 을 명확하게 나타내어야 합니다. l 저작권자로부터 별도의 허가를 받으면 이러한 조건들은 적용되지 않습니다. 저작권법에 따른 이용자의 권리는 위의 내용에 의하여 영향을 받지 않습니다. 이것은 이용허락규약(Legal Code)을 이해하기 쉽게 요약한 것입니다. Disclaimer 저작자표시. 귀하는 원저작자를 표시하여야 합니다. 비영리. 귀하는 이 저작물을 영리 목적으로 이용할 수 없습니다. 동일조건변경허락. 귀하가 이 저작물을 개작, 변형 또는 가공했을 경우 에는, 이 저작물과 동일한 이용허락조건하에서만 배포할 수 있습니다.
Effect of Vertebroplasty with Bone Filler Device and
Comparison with Balloon Kyphoplasty
by
DONG-HOON YANG
Major in Medicine
Department of Medical Sciences
The Graduate School, Ajou University
Effect of Vertebroplasty with Bone Filler Device and
Comparison with Balloon Kyphoplasty
by
DONG-HOON YANG
A Dissertation Submitted to
the Graduate School of Ajou University
in Partial Fulfillment of the Requirements of
the Degree of Master of Medicine
Supervised by
Ki Hong Cho, M.D., Ph.D.
Major in Medicine
Department of Medical Sciences
The Graduate School, Ajou University
This certifies that the dissertation of Dong-Hoon Yang
is approved.
SUPERVISORY COMMITTEE
________________________
Ki Hong Cho
________________________
Soo Han Yoon
________________________
Young Hwan Ahn
The Graduate School, Ajou University
December 13rd, 2013
- i -
- ABSTRACT -
Effect of Vertebroplasty with Bone Filler Device and Comparison
with Balloon Kyphoplasty
BACKGROUND CONTEXT: Vertebroplasty and kyphoplasty are popular procedures for
osteoporotic vertebral compression fractures. Although the kyphoplasty has a superior effect, it destroys normal vertebral trabecular structure and it has a higher cost.
PURPOSE: To analyze vertebroplasty with a bone filler device compared with conventional
kyphoplasty.
STUDY DESIGN: A cross-sectional study for comparison of two operation groups. PATIENT SAMPLE: Two-hundred twenty-two patients treated from January 2008 to
October 2012
OUTCOME MEASURES: Vertebral height, compression ratio, and segmental Cobb’s
angle were measured in preoperative and postoperative lateral X-rays.
METHODS: One hundred ninety-five patients were included after exclusion of 27 patients.
One level fractures numbered 169 (86.7%) cases and two level fractures numbered 26 (13.3%). A total of 221 vertebral levels were analyzed consequently. Statistical analysis was performed to identify significant differences between the two groups.
RESULTS: Vertebral height and compression ratio had stronger correlations than did
segmental Cobb’s angle. The compression ratio was the most influential parameter among the three variables. Adjusted postoperative compression ratio was not significantly different between the two operation groups, whereas adjusted postoperative vertebral height and
- ii -
segmental Cobb’s angle differed significantly (p < 0.05). Bone cement leakage rates did not differ (p < 0.05). Bone cement distribution was spongy type in the majority of the
vertebroplasty group (94.5%), but only spongy type in 42.0% of the kyphoplasty group. High bone densitometry (BMD) readings and long period from diagnosis to operation were
significant risk factors for bone cement leakage among preoperative conditions.
CONCLUSION: Compared with kyphoplasty, vertebroplasty with a bone filler device could
achieve equivalent compression reduction and bone cement leakage rate, as well as greater sponge-type bone cement distribution, which were advantages over conventional
vertebroplasty and kyphoplasty.
- iii -
TABLE OF CONTENTS
ABSTRACT ... i
TABLE OF CONTENTS ...iii
LIST OF FIGURES ... iv
LIST OF TABLES ... v
I. INTRODUCTION ... 1
II. MATERIALS AND METHODS ... 3
A. Inclusion and Exclusion Criteria... 3
B. Subjects ... 3 C. Measurement ... 3 D. Surgical technique... 4 E. Statistical Analysis ... 4 III. RESULT ... 6 IV. DISCUSSION ... 16
A. Vertebral height, compression ratio, and segmental Cobb’s angle ... 16
B. Equality of preoperative variables and adjusted postoperative variables ... 16
C. Intravertebral cleft and bone cement distribution ... 17
D. Bone cement volume ... 18
E. Bone cement leakage rate ... 19
F. Leakage risk factors due to preoperative conditions ... 20
G. Limitations ... 20
V. CONCLUSION ... 21
REFERENCES ... 22
- iv -
LIST OF FIGURES
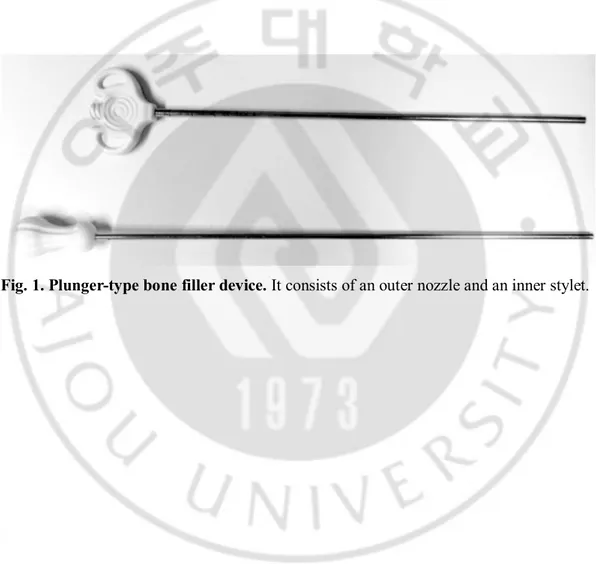
Fig. 1. Plunger-type bone filler device.. ... 2 Fig. 2. Different bone cement distributions ... 8 Fig. 3. Bone cement leakage after procedure ... 9 Fig. 4. Correlation relationship between vertebral height restoration, compression ratio
- v -
LIST OF TABLES
Table 1. Demographic data and comparison of preoperative condition.오류! 책갈피가 정의 되어 있지 않습니다.
Table 2. Comparison of vertebral height, compression ratio, Cobb’s angle, and bone cement. ... 오류! 책갈피가 정의되어 있지 않습니다. Table 3. Correlation of vertebral height, compression ratio, and Cobb’s angle.오류! 책갈피
가 정의되어 있지 않습니다.
Table 4. Comparison of postoperative values after correction of preoperative variables.오류! 책갈피가 정의되어 있지 않습니다.
Table 5. Risk factor assessments of bone cement leakage오류! 책갈피가 정의되어 있지 않습니다.
- 1 -
I.
INTRODUCTION
Osteoporotic vertebral compression fracture is a major health problem in the elderly. More than 1.4 million persons per year suffer from pain and morbidity related with this condition worldwide (Johnell and Kanis, 2006). Vertebroplasty and kyphoplasty for vertebral compression fracture have gained popularity over the past several years, and can overcome the disadvantages of non-surgical management with bed rest (Lyles et al., 1993). Although a recently published randomized controlled trial showed no superior advantage, subsequent meta-analysis study revealed that vertebroplasty and kyphoplasty provided greater pain relief and fewer subsequent fractures when compared to non-surgical management (Rousing et al., 2009; Ma et al., 2012; Papanastassiou et al., 2012). Class I evidence has been presented to support the advantages of vertebroplasty and kyphoplasty (Voormolen et al., 2007; Wardlaw et al., 2009; Berenson et al., 2011).
The effects of vertebroplasty and kyphoplasty extend beyond pain control to include vertebral height restoration, compression ratio reduction, and segmental Cobb’s angle reduction (Hiwatashi et al., 2003; Teng et al., 2003; Dublin et al., 2005; Pradhan et al., 2006; Hiwatashi et al., 2009).
The most annoying problem of this procedure is bone cement leakage, although most leakage does not cause clinical symptoms. Balloon kyphoplasty is more recently developed, and generally has a superior effect compared to vertebroplasty (Belkoff et al., 2001; Phillips et al., 2002; Hiwatashi et al., 2005; Shindle et al., 2006; Kim et al., 2012a; Papanastassiou et al., 2012). Meta-analysis study indicated that the incidence of bone cement leakage was lower than with kyphoplasty (Ma et al., 2012; Papanastassiou et al., 2012).
The distribution of the injected bone cement can be classified as spongy (trabecular, inter-digitation) and lumped (solid, cleft) (Oka et al., 2005; Tanigawa et al., 2007; Kim et al., 2012b). The lumped distribution is related with vertebral re-collapse and new fractures of adjacent vertebra and tends to be associated with kyphoplasty (Tanigawa et al., 2007; Kim et al., 2012b). Another unavoidable disadvantage of kyphoplasty is its higher medical cost compared to vertebroplasty.
The advantages of vertebroplasty, in turn, are a greater extent of sponge-shaped bone cement distribution and a lower medical cost; however, kyphoplasty causes less bone cement
- 2 - leakage and gives a better compression reduction.
In the present study, we have combined the advantages of these two procedures by performing vertebroplasty using a bone filler device (a plunger system with a nozzle and a stylet) that is commonly used for bone cement insertion during kyphoplasty (Fig. 1). This device has a larger diameter than the conventional 10-gauge vertebroplasty needle and allows injection of a bone cement of a higher viscosity than is possible with a syringe (Heini and Orler, 2004). The purpose of the present study was to establish whether this
vertebroplasty with a bone filler device could accomplish an equivalent compression reduction and bone cement leakage rate to that seen with balloon kyphoplasty.
- 3 -
II. MATERIALS AND METHODS
A. Inclusion and Exclusion CriteriaInclusion criteria for patients were one or two level osteoporotic vertebral body fractures within two months after symptom onset. The diagnosis was based on preoperative magnetic resonance imaging (MRI), except when MRI was contraindicated such as in heart pacemaker patients. Exclusion criteria were three or more levels of fracture, re-fracture, more than two months after symptom onset, severe degeneration that could not be checked for exact value, non-osteoporotic fracture, and adjacent segment fracture at the fusion level.
B. Subjects
A total of 222 patients underwent operations from January 2008 to October 2012. One hundred ninety-five patients were included and 27 patients were excluded based on the exclusion criteria.
Female patients were 155 (79.5%) cases whereas males were 40 (20.5%). Mean age was 73.30 ± 8.4 years old, ranging from 44 to 104 years old. One level fractures numbered 169 (86.7%) cases and two level fractures numbered 26 (13.3%). A total of 221 vertebral levels were subsequently included.
Although vertebroplasty and kyphoplasty are simple procedures, a different operator could bias the results. The present study has included only the first author’s operations in order to maintain an identical operative technique. The first author had more than two years’ experience performing vertebroplasty and kyphoplasty prior to the present study.
The polymethylmetacrylate (PMMA) bone cements were Exolent spine bone cement (Elmdown Ltd. London, U.K.) and Biomet bone cement V (Biomet Inc. Indiana, USA). A Sewon balloon syringe pump and bone filler device (Sewon Medical Co., Ltd., Rep. of Korea) were used for ballooning and bone cement injection, respectively.
C. Measurement
Preoperative and postoperative values of vertebral height, compression ratio, and segmental Cobb’s angle were measured in lateral X-ray from a workstation display (Raypax Co. Ltd. Rep. of Korea). Checking the exact length and angle from the spine of an elderly
- 4 -
patient was difficult because of bony spurs and degenerative kyphoscoliosis. In order to minimize inter-rater measurement errors, the first author checked all the data.
The measurement standard followed Keynan’s method (Keynan et al., 2006). The vertebral height was checked at the anterior aspect of the vertebral body. The compression ratio was calculated by subtracting the height of compressed vertebra from an average height of two adjacent vertebrae. Segmental Cobb’s angle was measured from upper endplate of the upper vertebral body and the lower endplate of the lower vertebral body.
D. Surgical technique
Conventional 10-gauge vertebroplasty needles were inserted into both pedicles. A guide wire was inserted through the needle, and then the needle was removed. A working cannula was inserted through the guide wire. The anterior tip of the working cannula was located within 5 mm of the posterior vertebral body margin. A reamer was advanced toward the anterior margin of the vertebral body to make a hollow tract. The bone filler device (a
plunger system with a nozzle and a stylet) was then filled with liquefied bone cement (Fig. 1). A bone cement-filled bone filler device was inserted into each of the working cannulas, and both were injected at the same time. Although the tract was created close to anterior vertebral body margin, the bone filler device was placed at the center of the vertebral body, as this was considered to reduce bone cement leakage.
One bone filler device was filled with 1.8 cc of bone cement. Four bone filler devices were injected for thoracolumbar lesion unless the leakage was prominent. Two or three bone filler devices were used for small upper- to mid-thoracic level injections. Every procedure was performed under fluoroscopic guidance.
E. Statistical Analysis
Comparisons between the vertebroplasty and kyphoplasty groups were analyzed with independent t-test for continuous variables and Pearson chi-square test for categorical variables. Relationship between vertebral height, compression ratio, and segmental Cobb’s angle were examined by correlation analysis. The general linear model (ANCOVA) was used to adjust effects of preoperative conditions. Risk factors for bone cement leakage were analyzed with logistic regression analysis. For all analyses, a two-sided p < 0.05 was
- 5 -
considered statistically significant. Statistical analysis was performed using SPSS (version 15, SPSS Inc., Chicago, IL).
- 6 -
III. RESULT
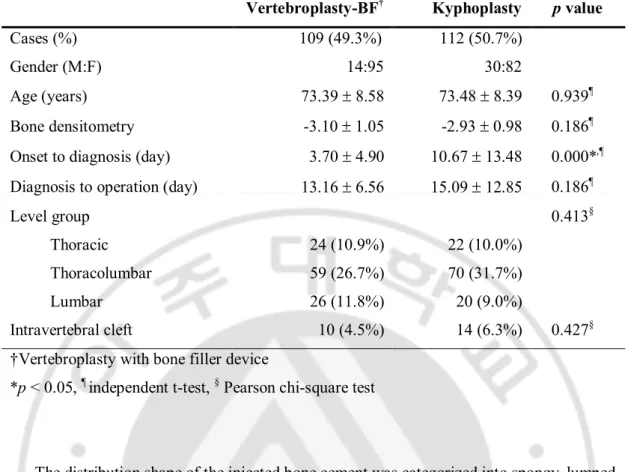
Vertebroplasty was performed for 109 (49.3%) levels and kyphoplasty for 112 (50.7%) (Table 1). The fracture level was categorized into three groups: thoracic spine fractures (T5-10) numbered 46 (20.8 %) levels, thoracolumbar (T11-L1) numbered 129 (58.4%), and lumbar (L2-5) numbered 46 (20.8%).
The preoperative period was divided into symptom-to-diagnosis and diagnosis-to-operation. The mean interval from pain onset to hospital arrival was 7.24 ± 10.8 days. The mean interval from diagnosis to operation was 14.14 ± 10.3 days.
The age, fracture level group, and BMD were not statistically different between the vertebroplasty and kyphoplasty groups (p > 0.05, Table 1).
Diagnosis to operation interval was not statistically different, whereas symptom onset to hospital arrival interval was significantly lower in the vertebroplasty group (3.70 ± 4.90 days) than in the kyphoplasty group (10.67 ± 13.48 days, p < 0.05, Table 1). Existence of an
- 7 -
Table 1. Demographic data and comparison of preoperative condition.
Vertebroplasty-BF† Kyphoplasty p value
Cases (%) 109 (49.3%) 112 (50.7%) Gender (M:F) 14:95 30:82 Age (years) 73.39 ± 8.58 73.48 ± 8.39 0.939¶
Bone densitometry -3.10 ± 1.05 -2.93 ± 0.98 0.186¶
Onset to diagnosis (day) 3.70 ± 4.90 10.67 ± 13.48 0.000*,¶
Diagnosis to operation (day) 13.16 ± 6.56 15.09 ± 12.85 0.186¶
Level group 0.413§
Thoracic 24 (10.9%) 22 (10.0%) Thoracolumbar 59 (26.7%) 70 (31.7%) Lumbar 26 (11.8%) 20 (9.0%)
Intravertebral cleft 10 (4.5%) 14 (6.3%) 0.427§
†Vertebroplasty with bone filler device
*p < 0.05, ¶ independent t-test, § Pearson chi-square test
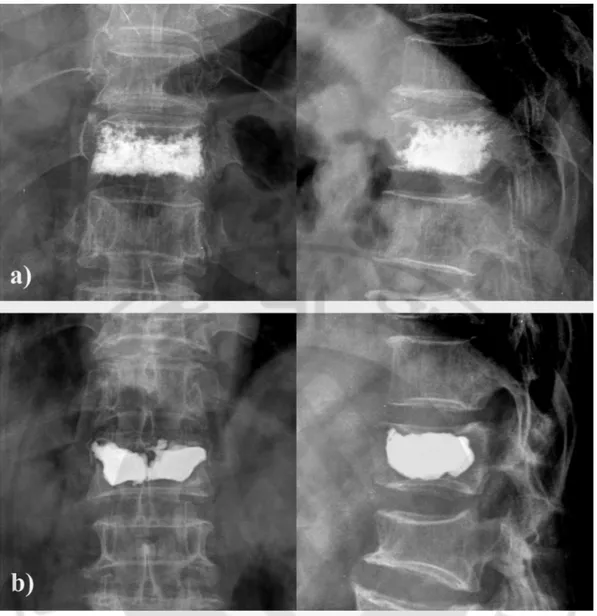
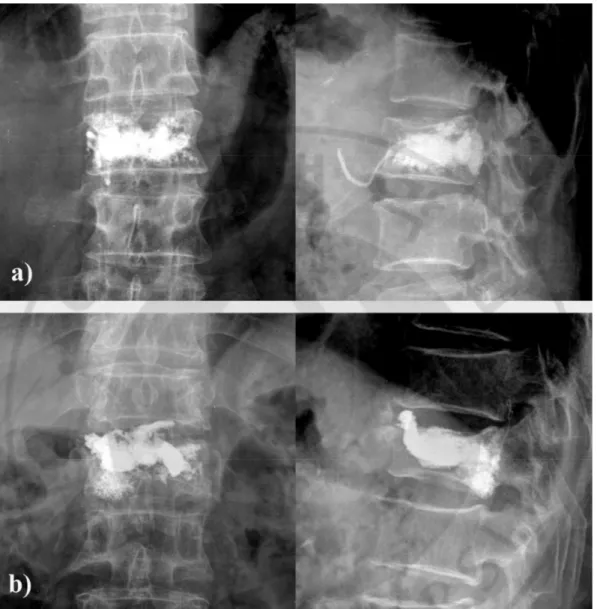
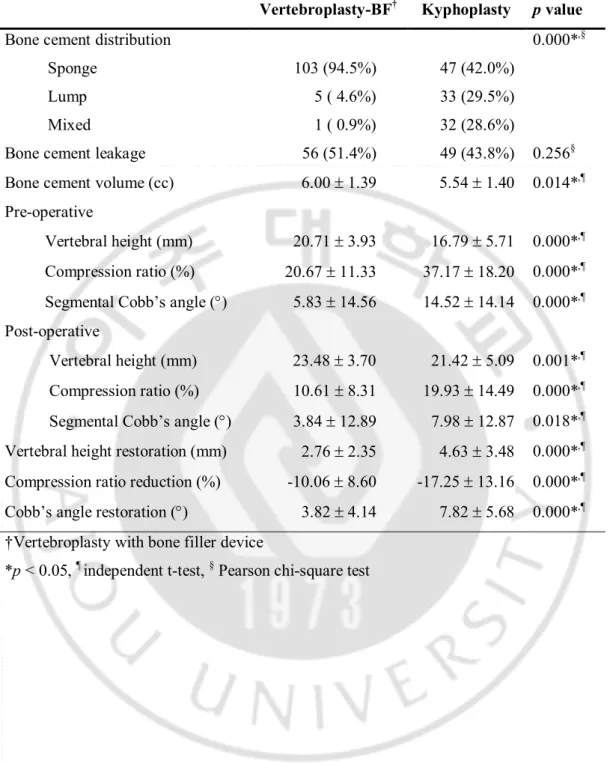
The distribution shape of the injected bone cement was categorized into spongy, lumped, and mixed type (Table 2) (Oka et al., 2005; Tanigawa et al., 2007; Kim et al., 2012b). Most vertebroplasty groups had the spongy type (103 cases, 94.5%) (Fig. 2-a). The kyphoplasty group numbered only 47 cases (42%); even if mixed type (32 cases, 28.6%) were included, the difference between the kyphoplasty and vertebroplasty groups was obvious. The lumped type accounted for 29.5% of the kyphoplasty group, which was much greater than the 4.6% observed in the vertebroplasty group (Fig. 2-b).
- 8 -
Fig. 2. Different bone cement distributions. a) Spongy shape after vertebroplasty with
bone filler device. b) Lumped shape after kyphoplasty.
Bone cement leakage was defined as cement leakage to the paravertebral area, disc space, vein, or lung. The leakage was verified at postoperative X-ray. Most leakage was minimal and none of the leakage had clinical importance. Leakage occurred in 56 cases (51.4%) of vertebroplasty and 49 cases (43.8%) of kyphoplasty (Fig. 3). However, these values were not statistically different (p > 0.05, Table 2).
- 9 -
A greater amount of bone cement was used in the vertebroplasty group (6.00 ± 1.39 cc) than in the kyphoplasty group (5.54 ± 1.40 cc, p < 0.05, Table 2).
Fig. 3. Bone cement leakage after procedure. a) Venous leakage after vertebroplasty with
- 10 -
Table 2. Comparison of vertebral height, compression ratio, Cobb’s angle, and bone cement.
Vertebroplasty-BF† Kyphoplasty p value
Bone cement distribution 0.000*,§
Sponge 103 (94.5%) 47 (42.0%) Lump 5 ( 4.6%) 33 (29.5%) Mixed 1 ( 0.9%) 32 (28.6%) Bone cement leakage 56 (51.4%) 49 (43.8%) 0.256§
Bone cement volume (cc) 6.00 ± 1.39 5.54 ± 1.40 0.014*,¶
Pre-operative
Vertebral height (mm) 20.71 ± 3.93 16.79 ± 5.71 0.000*,¶
Compression ratio (%) 20.67 ± 11.33 37.17 ± 18.20 0.000*,¶
Segmental Cobb’s angle (°) 5.83 ± 14.56 14.52 ± 14.14 0.000*,¶
Post-operative
Vertebral height (mm) 23.48 ± 3.70 21.42 ± 5.09 0.001*,¶
Compression ratio (%) 10.61 ± 8.31 19.93 ± 14.49 0.000*,¶
Segmental Cobb’s angle (°) 3.84 ± 12.89 7.98 ± 12.87 0.018*,¶
Vertebral height restoration (mm) 2.76 ± 2.35 4.63 ± 3.48 0.000*,¶
Compression ratio reduction (%) -10.06 ± 8.60 -17.25 ± 13.16 0.000*,¶
Cobb’s angle restoration (°) 3.82 ± 4.14 7.82 ± 5.68 0.000*,¶
†Vertebroplasty with bone filler device
- 11 -
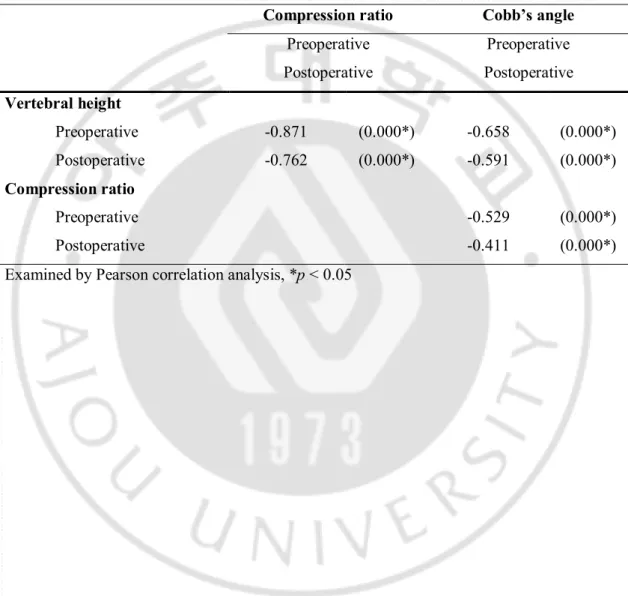
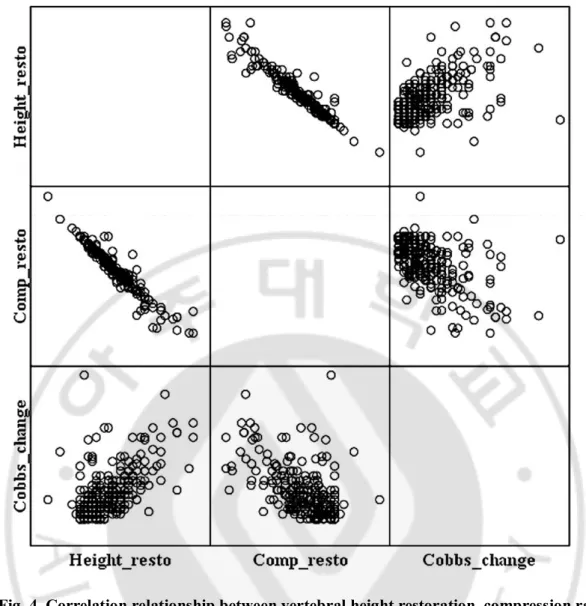
The vertebral height and compression ratio had a strong correlation: r = -0.871 for preoperative, -0.762 for postoperative (p < 0.05, Table 3, Fig. 4). However, the segmental Cobb’s angle had relatively weak correlation with the vertebral height and compression ratio: r = -0.658, -0.591 for preoperative, r = -0.529, -0.411 for postoperative (p < 0.05, Table 3, Fig. 4).
Table 3. Correlation of vertebral height, compression ratio, and Cobb’s angle. Compression ratio Cobb’s angle
Preoperative Preoperative Postoperative Postoperative Vertebral height Preoperative -0.871 (0.000*) -0.658 (0.000*) Postoperative -0.762 (0.000*) -0.591 (0.000*) Compression ratio Preoperative -0.529 (0.000*) Postoperative -0.411 (0.000*) Examined by Pearson correlation analysis, *p < 0.05
- 12 -
Fig. 4. Correlation relationship between vertebral height restoration, compression ratio restoration, and segmental Cobb’s angle change.
- 13 -
Preoperative vertebral height was significantly larger in the vertebroplasty group; preoperative compression ratio and segmental Cobb’s angle were significantly larger in the kyphoplasty group (p < 0.05, Table 2). This meant that the kyphoplasty group had a more prominent preoperative compression when compared to the vertebroplasty group.
The postoperative vertebral height, compression ratio, and segmental Cobb’s angle showed the same statistically significant differences (p < 0.05, Table 2). The vertebral height restoration of the vertebroplasty group was 2.76 ± 2.35 mm, whereas the kyphoplasty group was 4.63 ± 3.48 mm (p < 0.05, Table 2). The compression ratio reduction of the
vertebroplasty group was 10.06 ± 8.60%, whereas it was 17.25 ± 13.16% in the kyphoplasty group (p < 0.05, Table 2). The segmental Cobb’s angle change was also lower in the
vertebroplasty group (3.82 ± 4.14°) than in the kyphoplasty group (7.82 ± 5.68°, p < 0.05, Table 2). Simple comparisons of changes of the three variables showed the kyphoplasty technique was more effective than vertebroplasty with the bone filler device.
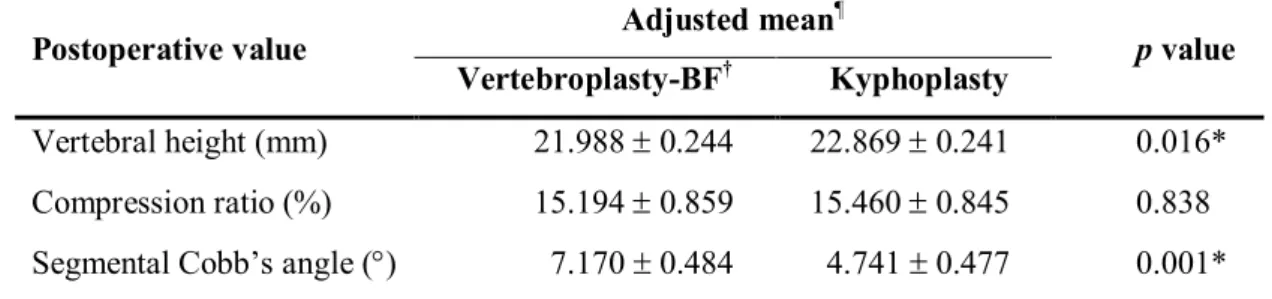
Postoperative values were adjusted with the general linear model using analysis of covariance (ANCOVA). Variables for adjustment included age, BMD, onset-to-diagnosis, diagnosis-to-operation, and bone cement volume. In addition, adjusted postoperative vertebral height included preoperative height, adjusted postoperative compression ratio included preoperative ratio, and adjusted postoperative segmental Cobb’s angle included preoperative angle. The adjusted postoperative vertebral height and segmental Cobb’s angle had statistically significant differences, whereas adjusted postoperative compression ratio failed to show statistical difference (15.194 ± 0.859 for vertebroplasty, 15.460 ± 0.845 for kyphoplasty, p < 0.05, Table 4).
- 14 -
Table 4. Comparison of postoperative values after correction of preoperative variables. Postoperative value Adjusted mean
¶
p value
Vertebroplasty-BF† Kyphoplasty
Vertebral height (mm) 21.988 ± 0.244 22.869 ± 0.241 0.016* Compression ratio (%) 15.194 ± 0.859 15.460 ± 0.845 0.838 Segmental Cobb’s angle (°) 7.170 ± 0.484 4.741 ± 0.477 0.001* †Vertebroplasty with bone filler device, *p < 0.05
¶ Examined by general linear model analysis (ANCOVA)
- Postoperative values were adjusted for age, BMD, onset to diagnosis interval, diagnosis to operation interval, and injected bone cement volume.
- Variables of each preoperative value were added to adjust each postoperative value.
Risk factors for bone cement leakage were analyzed by logistic regression analysis. Included factors were operation type, age, gender, level group, onset to admission interval, diagnosis to operation interval, injected bone cement volume, intravertebral cleft, BMD, bone cement distribution type, preoperative vertebral height, preoperative compression ratio, and preoperative segmental Cobb’s angle. The analysis indicated that BMD and diagnosis to operation interval were statistically significant risk factors for bone cement leakage (p < 0.05, Table 5). The odds ratio of leakage increased by 48.2% when BMD increased by one unit and increased by 3.4% when diagnosis to operation interval increased by one day.
- 15 -
Table 5. Risk factor assessments of bone cement leakage.
B p value Odds ratio 95.0% C.I.
Continuous variables
Age -0.016 0.398 0.984 0.949 - 1.021 Onset to admission 0.018 0.247 1.018 0.988 - 1.049 Diagnosis to operation 0.034 0.036 1.034 1.002 - 1.067 Bone densitometry 0.394 0.015 1.482 1.078 - 2.038 Bone cement volume -0.168 0.188 0.845 0.658 - 1.086 Preoperative height 0.066 0.489 1.068 0.886 - 1.288 Preoperative compression 0.002 0.936 1.002 0.954 - 1.052 Preoperative Cobb’s angle -0.004 0.812 0.996 0.966 - 1.027
Categorical variables Operation Vertebroplasty-BF† 1.000 Kyphoplasty -0.357 0.350 0.700 0.331 - 1.481 Gender Male 1.000 Female 0.309 0.424 1.362 0.638 - 2.905 Level group Thoracic 0.322 1.000 Thoracolumbar 0.042 0.932 1.043 0.397 - 2.744 Lumbar -0.738 0.288 0.478 0.123 - 1.864 Cleft sign on MRI
No 1.000
Yes 0.093 0.852 1.098 0.413 - 2.917 Bone cement distribution
Sponge 0.865 1.000
Lump 0.015 0.977 1.015 0.366 - 2.818 Mixed -0.237 0.634 0.789 0.298 - 2.090 Examined by binary logistic regression analysis, C.I.: confidence interval
- 16 -
IV. DISCUSSION
A. Vertebral height, compression ratio, and segmental Cobb’s angle
The present study compared vertebral height, compression ratio, and segmental Cobb’s angle change following the two procedures. Many studies have measured preoperative and postoperative values of the vertebral height and/or wedge angle to compare the
vertebroplasty and kyphoplasty, but the compression ratio has not been included previously (Hiwatashi et al., 2005; Pradhan et al., 2006; Hiwatashi et al., 2009; Sun et al., 2011). Normal vertebral height varies according to the patient’s height, gender, level, and
degenerative changes. Although the vertebral height is increased after the operation, it is not a consistent indicator for the measurement of compression. In contrast, Keynan’s method defines the vertebral compression ratio as including the vertebral height of the compressed level and two adjacent levels (Keynan et al., 2006). This measurement represents a practical change of the vertebral body and is more constant than the vertebral height.
The vertebral height and compression ratio showed very strong correlation, whereas segmental Cobb’s angle change had weak correlation with the vertebral height and
compression ratio (Fig. 4, Table 3). The cause of the weak correlation of segmental Cobb’s angle was assumed to reflect the relative position of the patient: a postoperative X-ray was taken in the supine position, whereas the preoperative X-ray was taken in the supine or erect position, according to the patient’s pain severity. Teng et al. reported that the effect of vertebroplasty on kyphosis reduction was less marked than on the vertebral height restoration, because the kyphosis angle was affected by the relative position of adjacent vertebral bodies and the intervertebral disc (Teng et al., 2003).
Based on the correlation and regularity of variables, the present study regarded that the compression ratio is a more important and influential factor than the vertebral height and segmental Cobb’s angle.
B. Equality of preoperative variables and adjusted postoperative variables
The vertebroplasty and kyphoplasty groups had similar frequencies (109, 112 cases). Preoperative covariances including age, BMD, fractured level group, diagnosis to operation interval did not differ between the two groups. Symptom onset to diagnosis interval was
- 17 -
significantly different; the reason for this was unclear but represented an unequal factor between the two groups.
Preoperative values of vertebral height, compression ratio, and segmental Cobb’s angle were significantly different between the two groups (p < 0.05, Table 2). In other words, the compression of the kyphoplasty group was more prominent. Although postoperative variables showed more changes in the kyphoplasty group, these were based on different preoperative conditions (Table 2). For example, 5% of the compression cases did not show increases greater than 5%, whereas 30% of the compression cases showed increases up to 30%. The group with greater compression had more potential for restoration. Clearly, these different preoperative conditions would have affected postoperative values.
The postoperative results were adjusted using a general linear model to overcome the different preoperative conditions (Table 4). The adjusted postoperative values were quite different from the pre-adjusted results (Table2). The adjusted postoperative vertebral height was significantly higher in the kyphoplasty group. The adjusted segmental Cobb’s angle was smaller in the kyphoplasty group. These results were the opposite of those obtained from the pre-adjusted comparison. Kyphoplasty showed a more effective recovery of the vertebral height and segmental Cobb’s angle. However, the postoperative compression ratio, a principal and most influential factor, differed, as it failed to show any advantage of the kyphoplasty. The vertebroplasty with the bone filler device achieved the same compression reduction as was observed with kyphoplasty.
C. Intravertebral cleft and bone cement distribution
The intravertebral cleft previously represented ischemic necrosis (Kümmell’s disease) (Laloux et al., 1991; Dupuy et al., 1996; Chou and Knight, 1997). The recent studies show that the cleft is a region of nonunion, with pseudoarthrosis of the fracture (Mochida et al., 2001; Ito et al., 2002; Lane et al., 2002; Hashidate et al., 2006). The cleft appears on non-contrast MRI as a vertebral cavity filled with fluid or gas occurring at the fractured endplate (Oka et al., 2005). It is an indication of nonunion of the bone and can show motion according to the patient’s position or respiration (Malghem et al., 1993). It is also an important factor for vertebral re-collapse and lumped type bone cement distribution (Kim et al., 2012b).
The bone cement distribution was categorized as spongy (trabecular, interdigitation), lumped (solid, cleft), and mixed type (Oka et al., 2005; Tanigawa et al., 2007; Kim et al.,
- 18 -
2012b). The spongy type was considered a more physiological distribution. The lumped type was a round mass congregation of bone cement with destroyed trabecular structure. It was related to the peri-halo phenomenon that led to vertebral re-collapse and new fractures of the adjacent vertebra (Tanigawa et al., 2007; Kim et al., 2012b). Tanigawa et al. reported that the lump shaped distribution increased the incidence of new compression fractures (Tanigawa et al., 2007). In contrast, another study reported that bone cement distribution had no influence on adjacent new fractures (Rho et al., 2012).
The present study showed that the frequency of intravertebral clefts did not differ between the two groups (Table 1). However, the bone cement distribution was significantly different (Table 2). The lump shaped distribution was found significantly more frequently in the kyphoplasty group; it was considered that the balloon inflation of the kyphoplasty had destroyed the normal trabecular structure. Vertebroplasty with the bone filler device was superior to kyphoplasty for bone cement distribution, as a more physiological spongy type bone cement distribution was made possible without destroying the normal trabecular structure.
D. Bone cement volume
The amount of bone cement that is adequate for vertebroplasty and kyphoplasty remains uncertain. Molloy et al. suggested that unipedicular injection of 3.5 cc of bone cement did not lead to preferential collapse (Molloy et al., 2005). A small bone cement amount is a cause of procedure failure, whereas a large bone cement amount may not be advisable clinically as it increases the risk of cement leakage (Ryu et al., 2002). A recent study indicated the optimal bone cement fraction was 24% of the vertebral body and suggested an optimal volume based on levels and gender: e.g., T12 for female was 3.35 to 5.22 cc (Nieuwenhuijse et al., 2012).
The mean bone cement amount differed according to several studies. Kummar et al. injected 3.2 cc for vertebroplasty and 1.8 cc for kyphoplasty (Kumar et al., 2010), while Movrin et al. injected 5.8 ± 1.7 and 5.5 ± 1.1 cc, respectively (Movrin et al., 2010), Lie et al. injected 4.91 ± 0.65 and 5.56 ± 0.62 cc, respectively (Liu et al., 2010), and Schofer et al. injected 3.9 ± 1.5 and 4.9 ± 1.2 cc (Schofer et al., 2009).
In the present study, the mean bone cement volume was 6.00 ± 1.39 cc for vertebroplasty and 5.54 ± 1.40 cc for kyphoplasty, which greater amounts than were used in previous
- 19 -
studies (Table 2). The bone cement volume used for the vertebroplasty group was
statistically greater than that used for the kyphoplasty group. This suggested that the cavity formation of the balloon of the kyphoplasty did not result in a greater need for bone cement injection when compared with the hollow tract formation of the bone filler device.
E. Bone cement leakage rate
The bone cement leakage is the most bothersome problem occurring during these procedures. Although most bone cement leakage did not cause clinical symptoms, some articles have reported serious complications such as symptomatic pulmonary embolism and intra-cardiac foreign body (Abdul-Jalil et al., 2007; Kim et al., 2013; Sifuentes Giraldo et al., 2013).
The combination of low-viscosity cement and high injection pressure leads to more frequent cement leakage through fractures and blood vessels (Nieuwenhuijse et al., 2011; Ma et al., 2012). More compression of the vertebral body and greater cortical disruption are also risk factors of bone cement leakage (Nieuwenhuijse et al., 2011). The presence of an
intravertebral cleft is also related to greater bone cement leakage (Ha et al., 2006; Nieuwenhuijse et al., 2011).
When compared with kyphoplasty, the vertebroplasty itself is a risk factor because of the use of lower viscosity cement and a smaller diameter needle. Leakage rates ranging from 11% to 73% have been reported in previous studies (Garfin et al., 2001; Watts et al., 2001;
Shapiro et al., 2003). The different diagnostic criteria used for leakage detection by X-ray were assumed to be a cause of this wide range of leakage rates. As shown in the CT study, if stricter criteria were applied, the leakage rate determined by X-ray would significantly increase (Schmidt et al., 2005).
Meta-analysis of the bone cement leakage rate revealed a value of 21.6% for
vertebroplasty and 13.1% for kyphoplasty, and the difference was statistically significant (Ma et al., 2012). The lower leakage rate is a practical reason for the preference for
kyphoplasty. The leakage rate in the present study was 51.4% for vertebroplasty and 43.8% for kyphoplasty, and these values were not statistically different (Table 2). The high rate of bone cement leakage of the conventional vertebroplasty could be adequately reduced by the use of the bone filler device.
- 20 - F. Leakage risk factors due to preoperative conditions
Logistic regression analysis of the preoperative conditions showed BMD and diagnosis to operation interval to be the significant risk factors. The bone cement leakage decreased 48.2% when BMD decreased by one unit. The leakage decreased 3.4% when diagnosis to operation interval decreased by one day (Table 5). In turn, an osteoporotic vertebra with low BMD had a low risk of bone cement leakage. Early operation after diagnosis also decreased the leakage rate. The operation type was not a statistically significant risk factor; the choice of the vertebroplasty with the bone filler device was not a risk factor of bone cement leakage. Although the intravertebral cleft was generally considered to be a risk factor for bone cement leakage, a recent study reported that it was not (Tanigawa et al., 2009). The present study also supported this conclusion as the logistic regression analysis also indicated that the intravertebral cleft was not a risk factor.
G. Limitations
The present study had several limitations. It was non-randomized and observational study. A control group that underwent conservative management was not included. The bone
cement injection pressure and velocity were controlled manually. Operative results were one surgeon’s results. Multicenter research and would increase reliability. Randomized case control trials should be evaluated.
- 21 -
V. CONCLUSION
Kyphoplasty is regarded as the next step in conventional vertebroplasty. However, this procedure has a few drawbacks such as destruction of the vertebral trabecular structure, a lumped shape bone cement distribution, and higher medical costs. Vertebroplasty with a bone filler device is a simple and familiar procedure. It showed an equivalent compression ratio reduction to that achieved with kyphoplasty. The bone cement distribution was more physiological and lumped distribution was avoided. Sufficient bone cement injection was possible without increasing the rate of bone cement leakage. Therefore, vertebroplasty with a bone filler device can be considered as a compatible option for the osteoporotic compression fracture, and has the advantages of both conventional vertebroplasty and kyphoplasty.
- 22 -
REFERENCES
1. Abdul-Jalil Y, Bartels J, Alberti O, Becker R: Delayed presentation of pulmonary
polymethylmethacrylate emboli after percutaneous vertebroplasty. Spine (Phila Pa 1976) 32: E589-593, 2007
2. Belkoff SM, Mathis JM, Fenton DC, Scribner RM, Reiley ME, Talmadge K: An ex vivo biomechanical evaluation of an inflatable bone tamp used in the treatment of
compression fracture. Spine (Phila Pa 1976) 26: 151-156, 2001
3. Berenson J, Pflugmacher R, Jarzem P, Zonder J, Schechtman K, Tillman JB, Bastian L, Ashraf T, Vrionis F, Cancer Patient Fracture Evaluation I: Balloon kyphoplasty versus non-surgical fracture management for treatment of painful vertebral body compression fractures in patients with cancer: a multicentre, randomised controlled trial. Lancet Oncol 12: 225-235, 2011
4. Chou LH, Knight RQ: Idiopathic avascular necrosis of a vertebral body. Case report and literature review. Spine (Phila Pa 1976) 22: 1928-1932, 1997
5. Dublin AB, Hartman J, Latchaw RE, Hald JK, Reid MH: The vertebral body fracture in osteoporosis: restoration of height using percutaneous vertebroplasty. AJNR Am J Neuroradiol 26: 489-492, 2005
6. Dupuy DE, Palmer WE, Rosenthal DI: Vertebral fluid collection associated with vertebral collapse. AJR Am J Roentgenol 167: 1535-1538, 1996
7. Garfin SR, Yuan HA, Reiley MA: New technologies in spine: kyphoplasty and vertebroplasty for the treatment of painful osteoporotic compression fractures. Spine (Phila Pa 1976) 26: 1511-1515, 2001
8. Ha KY, Lee JS, Kim KW, Chon JS: Percutaneous vertebroplasty for vertebral
compression fractures with and without intravertebral clefts. J Bone Joint Surg Br 88: 629-633, 2006
9. Hashidate H, Kamimura M, Nakagawa H, Takahara K, Uchiyama S: Pseudoarthrosis of vertebral fracture: radiographic and characteristic clinical features and natural history. J Orthop Sci 11: 28-33, 2006
10. Heini PF, Orler R: Kyphoplasty for treatment of osteoporotic vertebral fractures. Eur Spine J 13: 184-192, 2004
- 23 -
11. Hiwatashi A, Moritani T, Numaguchi Y, Westesson PL: Increase in vertebral body height after vertebroplasty. AJNR Am J Neuroradiol 24: 185-189, 2003
12. Hiwatashi A, Sidhu R, Lee RK, deGuzman RR, Piekut DT, Westesson PL: Kyphoplasty versus vertebroplasty to increase vertebral body height: a cadaveric study. Radiology 237: 1115-1119, 2005
13. Hiwatashi A, Westesson PL, Yoshiura T, Noguchi T, Togao O, Yamashita K, Kamano H, Honda H: Kyphoplasty and vertebroplasty produce the same degree of height
restoration. AJNR Am J Neuroradiol 30: 669-673, 2009
14. Ito Y, Hasegawa Y, Toda K, Nakahara S: Pathogenesis and diagnosis of delayed vertebral collapse resulting from osteoporotic spinal fracture. Spine J 2: 101-106, 2002 15. Johnell O, Kanis JA: An estimate of the worldwide prevalence and disability associated
with osteoporotic fractures. Osteoporos Int 17: 1726-1733, 2006
16. Keynan O, Fisher CG, Vaccaro A, Fehlings MG, Oner FC, Dietz J, Kwon B,
Rampersaud R, Bono C, France J, Dvorak M: Radiographic measurement parameters in thoracolumbar fractures: a systematic review and consensus statement of the spine trauma study group. Spine (Phila Pa 1976) 31: E156-165, 2006
17. Kim HT, Kim YN, Shin HW, Kim IC, Kim H, Park NH, Choi SY: Intracardiac foreign body caused by cement leakage as a late complication of percutaneous vertebroplasty. Korean J Intern Med 28: 247-250, 2013
18. Kim KH, Kuh SU, Chin DK, Jin BH, Kim KS, Yoon YS, Cho YE: Kyphoplasty versus vertebroplasty: restoration of vertebral body height and correction of kyphotic deformity with special attention to the shape of the fractured vertebrae. J Spinal Disord Tech 25: 338-344, 2012a
19. Kim KH, Kuh SU, Park JY, Kim KS, Chin DK, Cho YE: What is the importance of "halo" phenomenon around bone cement following vertebral augmentation for osteoporotic compression fracture? Osteoporos Int 23: 2559-2565, 2012b
20. Kumar K, Nguyen R, Bishop S: A comparative analysis of the results of vertebroplasty and kyphoplasty in osteoporotic vertebral compression fractures. Neurosurgery 67: ons171-188; discussion ons188, 2010
21. Laloux P, Lefebvre S, Esselinckx W, de Cloedt P: Spinal cord compression secondary to vertebral aseptic osteonecrosis. Spine (Phila Pa 1976) 16: 480-481, 1991
- 24 -
22. Lane JI, Maus TP, Wald JT, Thielen KR, Bobra S, Luetmer PH: Intravertebral clefts opacified during vertebroplasty: pathogenesis, technical implications, and prognostic significance. AJNR Am J Neuroradiol 23: 1642-1646, 2002
23. Liu JT, Liao WJ, Tan WC, Lee JK, Liu CH, Chen YH, Lin TB: Balloon kyphoplasty versus vertebroplasty for treatment of osteoporotic vertebral compression fracture: a prospective, comparative, and randomized clinical study. Osteoporos Int 21: 359-364, 2010
24. Lyles KW, Gold DT, Shipp KM, Pieper CF, Martinez S, Mulhausen PL: Association of osteoporotic vertebral compression fractures with impaired functional status. Am J Med 94: 595-601, 1993
25. Ma XL, Xing D, Ma JX, Xu WG, Wang J, Chen Y: Balloon kyphoplasty versus percutaneous vertebroplasty in treating osteoporotic vertebral compression fracture: grading the evidence through a systematic review and meta-analysis. Eur Spine J 21: 1844-1859, 2012
26. Malghem J, Maldague B, Labaisse MA, Dooms G, Duprez T, Devogelaer JP, Vande Berg B: Intravertebral vacuum cleft: changes in content after supine positioning. Radiology 187: 483-487, 1993
27. Mochida J, Toh E, Chiba M, Nishimura K: Treatment of osteoporotic late collapse of a vertebral body of thoracic and lumbar spine. J Spinal Disord 14: 393-398, 2001 28. Molloy S, Riley LH, 3rd, Belkoff SM: Effect of cement volume and placement on
mechanical-property restoration resulting from vertebroplasty. AJNR Am J Neuroradiol 26: 401-404, 2005
29. Movrin I, Vengust R, Komadina R: Adjacent vertebral fractures after percutaneous vertebral augmentation of osteoporotic vertebral compression fracture: a comparison of balloon kyphoplasty and vertebroplasty. Arch Orthop Trauma Surg 130: 1157-1166, 2010
30. Nieuwenhuijse MJ, Bollen L, van Erkel AR, Dijkstra PD: Optimal intravertebral cement volume in percutaneous vertebroplasty for painful osteoporotic vertebral compression fractures. Spine (Phila Pa 1976) 37: 1747-1755, 2012
31. Nieuwenhuijse MJ, Van Erkel AR, Dijkstra PD: Cement leakage in percutaneous vertebroplasty for osteoporotic vertebral compression fractures: identification of risk
- 25 - factors. Spine J 11: 839-848, 2011
32. Oka M, Matsusako M, Kobayashi N, Uemura A, Numaguchi Y: Intravertebral cleft sign on fat-suppressed contrast-enhanced MR: correlation with cement distribution pattern on percutaneous vertebroplasty. Acad Radiol 12: 992-999, 2005
33. Papanastassiou ID, Phillips FM, Van Meirhaeghe J, Berenson JR, Andersson GB, Chung G, Small BJ, Aghayev K, Vrionis FD: Comparing effects of kyphoplasty, vertebroplasty, and surgical management in a systematic review of randomized and
non-randomized controlled studies. Eur Spine J 21: 1826-1843, 2012
34. Phillips FM, Todd Wetzel F, Lieberman I, Campbell-Hupp M: An in vivo comparison of the potential for extravertebral cement leak after vertebroplasty and kyphoplasty. Spine (Phila Pa 1976) 27: 2173-2178; discussion 2178-2179, 2002
35. Pradhan BB, Bae HW, Kropf MA, Patel VV, Delamarter RB: Kyphoplasty reduction of osteoporotic vertebral compression fractures: correction of local kyphosis versus overall sagittal alignment. Spine (Phila Pa 1976) 31: 435-441, 2006
36. Rho YJ, Choe WJ, Chun YI: Risk factors predicting the new symptomatic vertebral compression fractures after percutaneous vertebroplasty or kyphoplasty. Eur Spine J 21: 905-911, 2012
37. Rousing R, Andersen MO, Jespersen SM, Thomsen K, Lauritsen J: Percutaneous vertebroplasty compared to conservative treatment in patients with painful acute or subacute osteoporotic vertebral fractures: three-months follow-up in a clinical randomized study. Spine (Phila Pa 1976) 34: 1349-1354, 2009
38. Ryu KS, Park CK, Kim MC, Kang JK: Dose-dependent epidural leakage of
polymethylmethacrylate after percutaneous vertebroplasty in patients with osteoporotic vertebral compression fractures. J Neurosurg 96: 56-61, 2002
39. Schmidt R, Cakir B, Mattes T, Wegener M, Puhl W, Richter M: Cement leakage during vertebroplasty: an underestimated problem? Eur Spine J 14: 466-473, 2005
40. Schofer MD, Efe T, Timmesfeld N, Kortmann HR, Quante M: Comparison of
kyphoplasty and vertebroplasty in the treatment of fresh vertebral compression fractures. Arch Orthop Trauma Surg 129: 1391-1399, 2009
41. Shapiro S, Abel T, Purvines S: Surgical removal of epidural and intradural
- 26 -
osteoporotic lumbar compression fracture. Case report. J Neurosurg 98: 90-92, 2003 42. Shindle MK, Gardner MJ, Koob J, Bukata S, Cabin JA, Lane JM: Vertebral height
restoration in osteoporotic compression fractures: kyphoplasty balloon tamp is superior to postural correction alone. Osteoporos Int 17: 1815-1819, 2006
43. Sifuentes Giraldo WA, Lamua Riazuelo JR, Gallego Rivera JI, Vazquez Diaz M: Cement pulmonary embolism after vertebroplasty. Reumatol Clin 9: 239-242, 2013 44. Sun G, Jin P, Li M, Liu XW, Li FD: Height restoration and wedge angle correction
effects of percutaneous vertebroplasty: association with intraosseous clefts. Eur Radiol 21: 2597-2603, 2011
45. Tanigawa N, Kariya S, Komemushi A, Tokuda T, Nakatani M, Yagi R, Sawada S: Cement leakage in percutaneous vertebroplasty for osteoporotic compression fractures with or without intravertebral clefts. AJR Am J Roentgenol 193: W442-445, 2009 46. Tanigawa N, Komemushi A, Kariya S, Kojima H, Shomura Y, Omura N, Sawada S:
Relationship between cement distribution pattern and new compression fracture after percutaneous vertebroplasty. AJR Am J Roentgenol 189: W348-352, 2007
47. Teng MM, Wei CJ, Wei LC, Luo CB, Lirng JF, Chang FC, Liu CL, Chang CY:
Kyphosis correction and height restoration effects of percutaneous vertebroplasty. AJNR Am J Neuroradiol 24: 1893-1900, 2003
48. Voormolen MH, Mali WP, Lohle PN, Fransen H, Lampmann LE, van der Graaf Y, Juttmann JR, Jansssens X, Verhaar HJ: Percutaneous vertebroplasty compared with optimal pain medication treatment: short-term clinical outcome of patients with
subacute or chronic painful osteoporotic vertebral compression fractures. The VERTOS study. AJNR Am J Neuroradiol 28: 555-560, 2007
49. Wardlaw D, Cummings SR, Van Meirhaeghe J, Bastian L, Tillman JB, Ranstam J, Eastell R, Shabe P, Talmadge K, Boonen S: Efficacy and safety of balloon kyphoplasty compared with non-surgical care for vertebral compression fracture (FREE): a
randomised controlled trial. Lancet 373: 1016-1024, 2009
50. Watts NB, Harris ST, Genant HK: Treatment of painful osteoporotic vertebral fractures with percutaneous vertebroplasty or kyphoplasty. Osteoporos Int 12: 429-437, 2001
- 27 -
- 국문 요약 -
피스톤
방식 주입기를 이용한 척추체 성형술의 효과
아주대학교 대학원 의학과 양 동 훈 (지도교수: 조 기 홍) 배경: 척추체 성형술과 풍선 척추체 성형술은 골다공증성 척추 압박골절에 널리 쓰이는 치료법이다. 풍선 척추체 성형술이 더 나은 효과를 보인다고 알려져 있으 나 척추체의 골소주를 파괴하고 비용이 더 높다는 단점이 있다. 목적: 피스톤 방식 뼈시멘트 주입기를 이용한 척추체 성형술과 풍선 척추체 성형 술의 결과를 비교한다. 연구 디자인: 두 가지 수술 그룹의 비교를 통한 단면 연구. 연구 대상: 2008년 1월부터 2012년 10월까지 수술을 시행한 222명. 결과 측정: 수술 전 후의 척추체 높이, 척추체 압박율, 및 Cobb 각도를 측정하고 비교하였다. 방법: 222명 중 27명을 제외한 195명의 환자가 포함되었으며, 1분절의 골절은 169 명 이었고 (86.7%), 두 분절의 골절은 26명 이었다 (13.3%). 총 221개의 척추 분 절에 대해 두 그룹간의 차이를 알기 위해 통계학적 분석을 시행하였다. 결과: 척추체 높이와 압박율은 Cobb각도와 비교 시 더 높은 상관관계를 보였으 며. 세 변수 중 척추체 압박율이 가장 영향력 있는 변수였다. 일반선형모델로 보- 28 - 정한 수술 후 척추체 높이와 Cobb 각도는 두 수술 그룹 간 유의한 차이를 보인 반면, 보정한 수술 후 압박율은 유의한 차이를 보이지 않았다 (p < 0.05). 뼈시멘 트 분포는 척추체 성형술 군에서는 대부분이 spongy형태를 보였으나 (94.5%), 풍 선 척추체 성형술 군에서는 42%로 낮았다. 높은 골밀도 (BMD) 수치와 진단 후 수술까지의 긴 기간은 뼈시멘트 누출을 증가시키는 위험 인자였다. 결론: 피스톤 방식 뼈시멘트 주입기를 이용한 척추체 성형술은 풍선 척추체 성형 술과 대등한 압박율 복원 및 뼈시멘트 누출율을 보일 뿐 아니라, 대부분이 spongy 형태의 뼈시멘트 분포를 보여. 척추체 성형술과 풍선 척추체 성형술의 이 점을 함께 보여주는 효과적인 치료 방법으로 생각된다. 핵심어: 척추체 성형술, 풍선 척추체 성형술, bone filler, 척추체 압박 골절, 뼈시멘 트