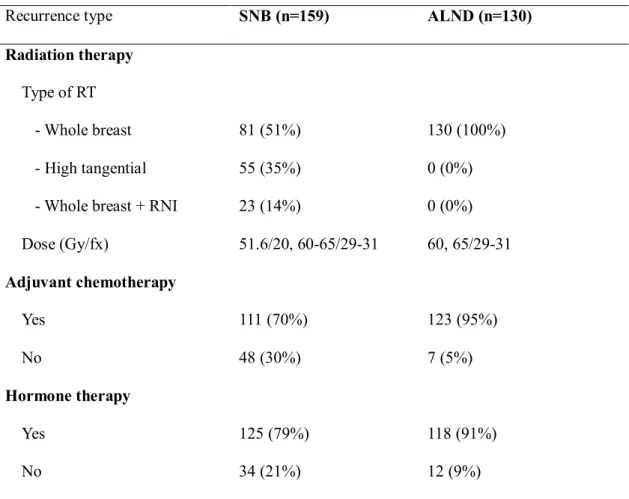
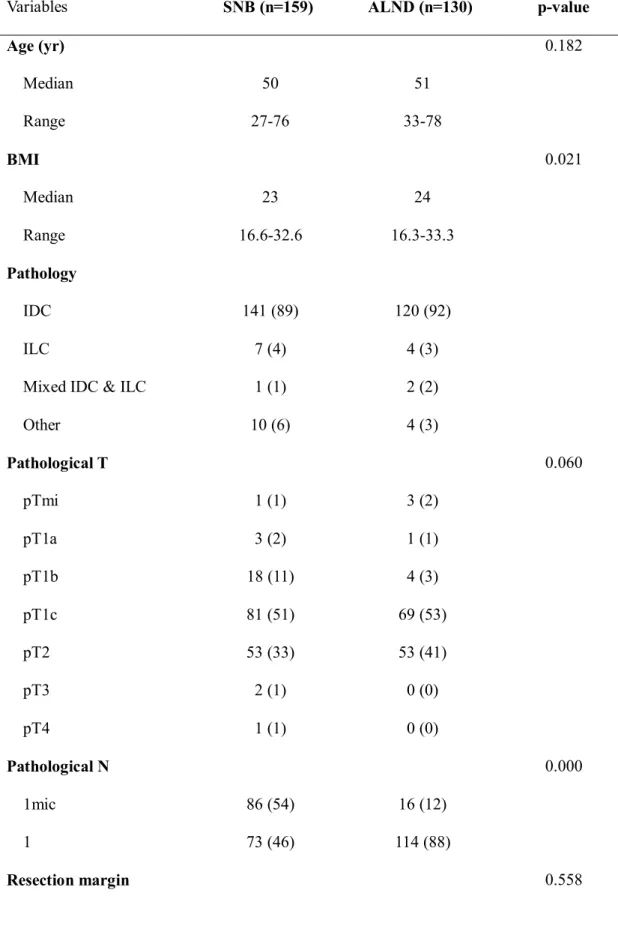
Materials and methods: We retrospectively analyzed patients with pN1M0 breast cancer who were treated with breast-conserving surgery and adjuvant radiation therapy (RT) between January 2012 and July 2015. To compare treatment outcomes and complications, 40 patients treated with third field RT (whole breast RT + regional nodal radiation) in the ALND group were excluded. Among these patients, 130 patients underwent axillary lymph node dissection (ALND) and 159 patients underwent sentinel lymph node biopsy (SNB) alone. n=23) of patients in the SNB group treated with third field RT.
The proportion of patients with a positive estrogen receptor (ER) and those with Ki-67 less than 14% in the SNB group was significantly lower than that in the ALND group. Compared to patients treated with other types of RT (whole breast RT, high tangent RT), patients treated with third field RT had more risky features. In the SNB group, a regional recurrence was observed in one patient treated with standard tangential field RT.
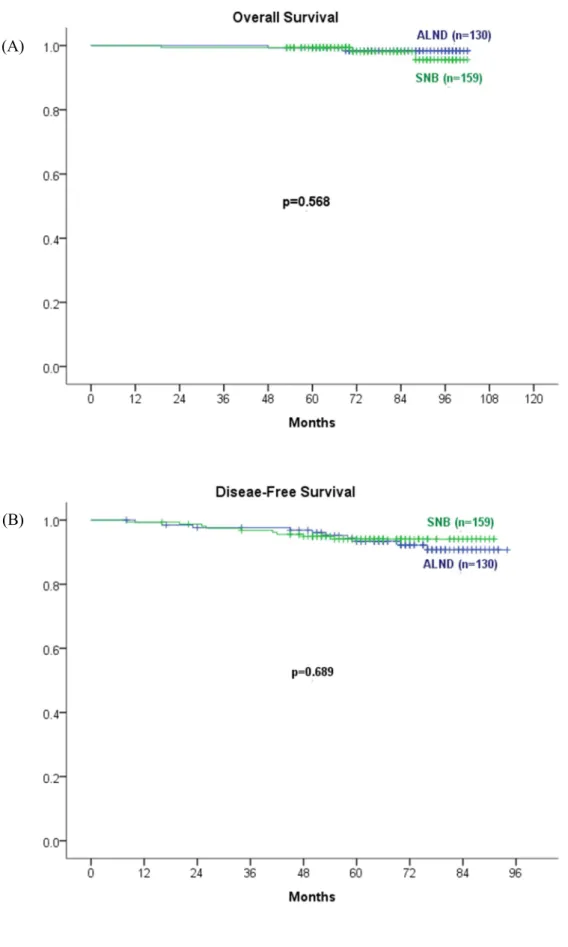
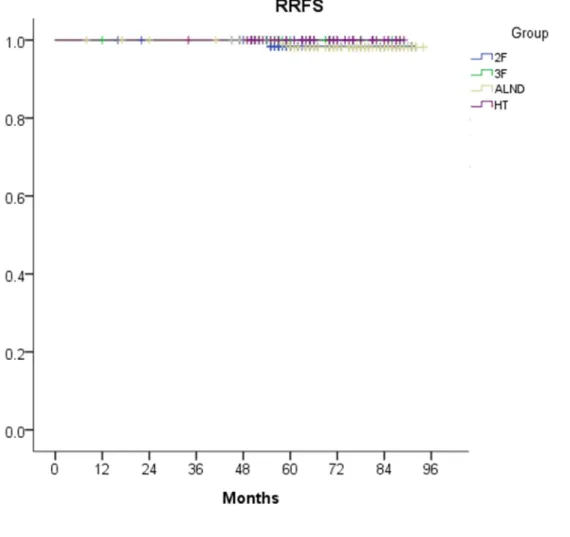
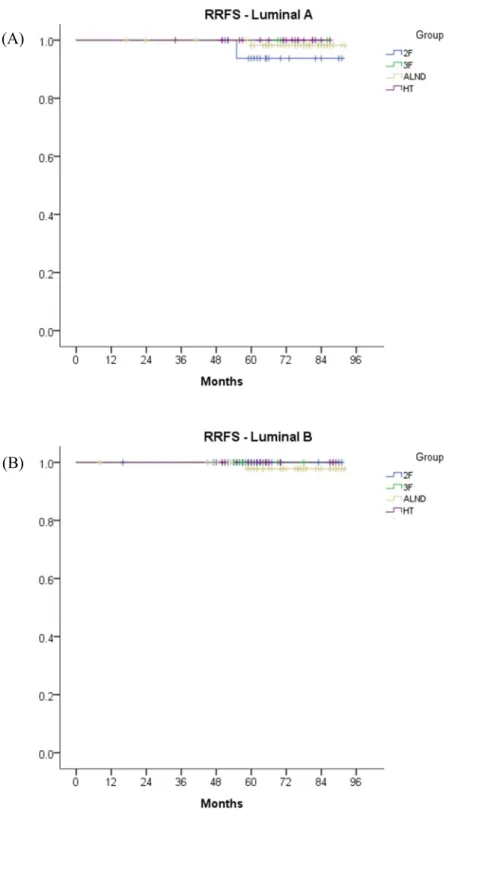
Regional recurrence was not observed in patients who underwent high-tangent RT or third-field RT. There was no significant difference in 5-year RRFS by type of radiation treatment area or molecular subtype. Conclusion: In cN0/pN1 breast cancer patients, ALND did not improve OS or DFS, but.
Introduction
Materials and Methods
We contoured lymph nodes at levels I and II in the axilla for adequate coverage and adjusted the caudal border to cover 1 cm above the axillary vein (Figure 2). The highly tangential fields were modified with multileaf collimators (MLCs) to reduce the radiation dose to the pectoralis major muscle and to achieve adequate coverage of the axillary lymph nodes. Patients who underwent breast-conserving surgery were included in this study, and patients who underwent mastectomy were excluded.
The extent of ALND varied according to individual surgeon preference, but the majority of patients underwent stage I and II lymph node dissection (n = 82, 63%). We assessed regional recurrence-free survival (RRFS), overall survival (OS), disease-free survival (DFS), and pattern of recurrence (ie, locoregional, contralateral breast, distant metastases). RRFS was defined as the time from initiation of RT to regional recurrence or death from any cause.
OS was defined as the time from the first diagnosis of the disease to the date of last follow-up or the date of death. DFS was defined as the time from initiation of RT to disease recurrence or death from any cause. Lymphedema was assessed by measuring limb volume (Circumference at the wrist and 5 cm below/above the elbow).
Breast cancer-related lymphedema (BCRL) was defined as a difference in volume between the affected arm and the unaffected arm of 2 cm or more.
Results
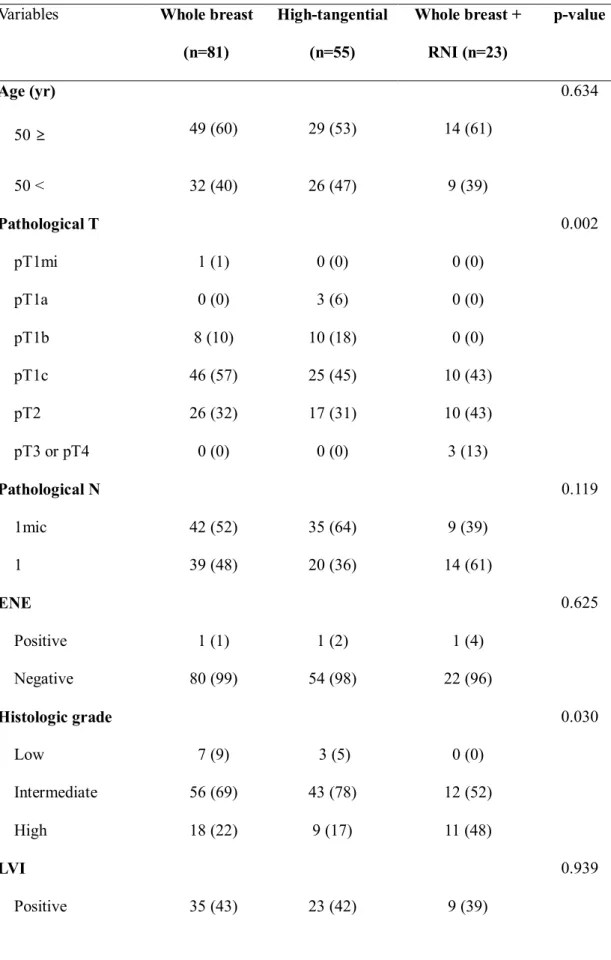
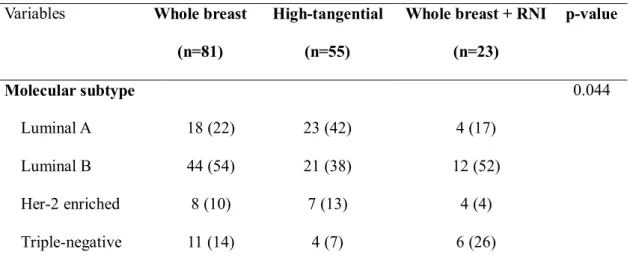
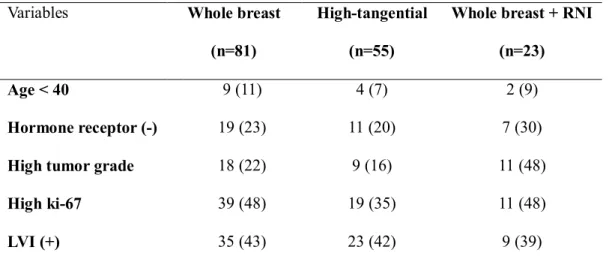
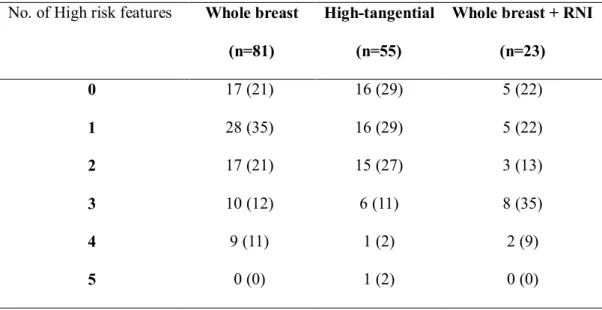
The high-risk characteristics of patients in the SNB group are summarized according to the field of irradiation (Table 4). The proportion of patients with two or more high-risk features was 44% in patients treated with whole breast RT (36/81) and 42% in patients treated with high tangent RT (23/55). Compared with these two groups, patients treated with third-field RT (whole breast + RNI) had more high-risk characteristics (Table 5).
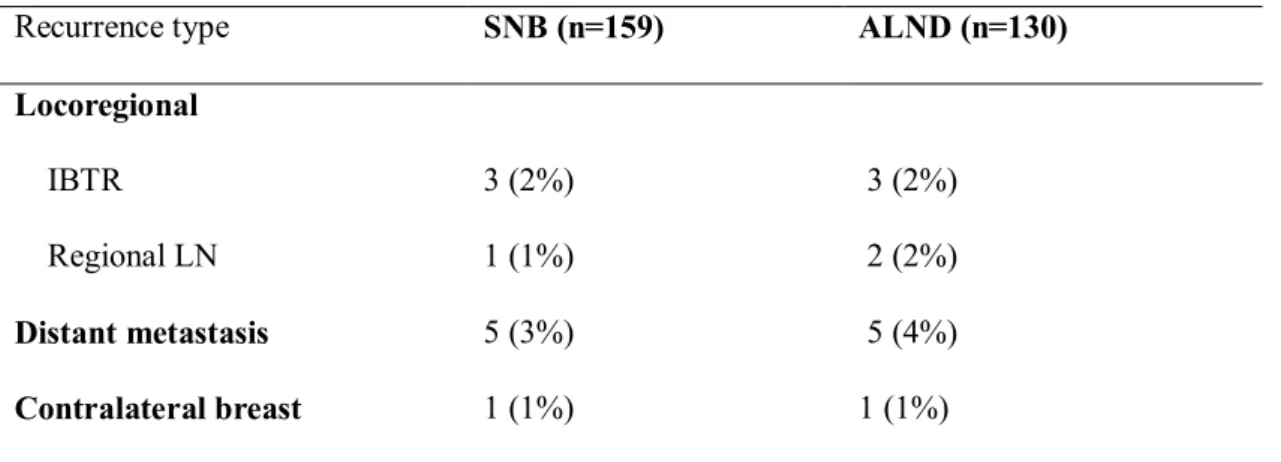
Adjuvant hormone therapy was administered to 125 patients (79%) in the SNB group and 118 patients (91%) in the ALND group. At the median follow-up of 73 months, there were 6 cases of ipsilateral breast tumor recurrence (IBTR) and 2 relapses in the contralateral breast. There were 3 cases of regional recurrence (axillary and supraclavicular lymph nodes) and 10 cases of distant recurrence.
Patients in the SNB group were also divided by molecular subtype (ie, Luminal A, Luminal B, triple negative, Her-2 enriched) or area of irradiation (ie, Whole Breast, High Tangential, Whole Breast + RNI). ), but no significant differences were observed in RRFS (Figures 5, 6), OS, or DFS. The median time to develop BCRL was 13 months in the SNB group and 7.5 months in the ALND group.
Discussion
In this study, there was 1 regional lymph node recurrence in the SNB group and 2 in the ALND group. In addition, there was no significant difference in treatment outcomes compared to the results of patients treated with whole breast RT alone or high tangential RT after SNB. In cases of positive control lymph nodes, the probability of non-control lymph nodes being affected is not small.
Not only third-field RT, which includes the supraclavicular and axillary regions, whole-breast RT and high-tangent RT can also include a significant component of the axillary region [16-18]. In the SNB group, there were no significant differences in treatment outcomes (RRFS, OS, DFS, BCRL) according to the field of irradiation. There was only one case of regional lymph node recurrence (axillary lymph node) and this patient was treated with standard tangential field RT.
BCRL occurred in 4 patients, 3 of whom were treated with high tangent RT and 1 with whole breast RT. Most BCRL in the SNB group occurred in patients receiving high-tangent RT (75%), although it was not statistically significant. Currently, chemotherapy is not given if the results of genomic tests such as MammaPrint or Oncotpye Dx are considered low risk, even if there is a positive sentinel lymph node.
In these patients, high tangential RT may provide better coverage of the axillary area than standard tangential RT [20,21]. In the current study, no regional recurrence was observed in the patients who underwent high-pressure RT or RNI. Treatment outcomes for patients who received high-tangent RT were no worse than patients who received ALND or whole-breast RT.
In addition, high-tangent RT did not increase the incidence of BCRL and was significantly lower than that of the ALND group. And the absence of regional recurrence in patients treated with high tangent RT or RNI suggests that axillary coverage with RT may be beneficial in patients who have not undergone ALND.
Conclusions
목적: 임상병기 N0(cN0)으로 평가된 유방암 환자에서 유방보존술 후 병리학적 병기 N1(pN1) 환자의 치료 결과 및 재발 패턴을 파악하고 이에 따른 적절한 방사선 치료 범위를 결정하고자 한다. 청구서. 환자를 감시림프절 생검 그룹과 겨드랑이 림프절 절제 그룹으로 나누었습니다. 그리고 겨드랑이 림프절 절제술을 받은 환자의 치료 결과와 합병증을 비교합니다.
이 중 국소 림프절 방사선 조사를 받은 환자 40명은 제외되었습니다. 결절 생검만을 시행한 환자 중 81명은 표준 접선 방사선 치료를 받았고, 55명은 고접선 방사선 치료를 받았으며, 23명은 전체 유방 및 국소 림프절 방사선 치료를 받았습니다. 시행되었습니다. 81%의 환자에서 내과적 치료가 시행되었습니다.
모든 호르몬 수용체 양성 환자에서도 마찬가지다. 국소적 무재발 생존기간과 2차 평가변수는 전체 생존기간, 무재발 생존기간, 유방암 관련 림프부종이었다. 결과: 연구에 등록한 환자의 평균 연령은 50세였습니다.
겨드랑이 림프절 절제술을 받은 환자와 비교하여 감시 림프절 생검을 받은 환자의 에스트로겐 수용체 풍부도. N1mic 단계의 환자 비율은 감시 림프절 생검만 받은 환자에서 유의하게 더 높았습니다. 국소재발 3예 중 1예는 감시림프절 생검만을 시행한 환자에서 발생하였고, 2예는 겨드랑이림프절절제술을 시행한 환자에서 발생하였다.
방사선치료만 받은 환자군에서는 표준삼각방사선치료를 받은 환자 1명에서만 국소재발이 발생하였고, 고삼각방사선치료나 국소림프절 방사선치료를 받은 환자에서는 발생하지 않았다. 액와 림프절 절제술을 받은 환자에서 유방암 관련 림프부종의 발생률.