REPO RT
Clin Exp Thyroidol 2015 May 8(1): 103-107 http://dx.doi.org/10.11106/cet.2015.8.1.103Received April 7, 2014 / Revised 1st July 7, 2014, 2nd August 11, 2014 / Accepted August 13, 2014
Correspondence: Keum-Seok Bae, MD, PhD, Department of Surgery, Wonju Severance Christian Hospital, 20 Ilsan-ro, Wonju 220-701, Korea
Tel: 82-33-741-1303, Fax: 82-33-742-1815, E-mail: bksgs@yonsei.ac.kr
Copyright ⓒ 2015, the Korean Thyroid Association. All rights reserved.
This is an open-access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http:// creative- commons.org/licenses/by-nc/4.0/), which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Poorly Differentiated Thyroid Carcinoma with Gross Internal Jugular Vein Invasion and
Multiple Lung Metastases
Yong-Moon Lee
1, Jae Hyun Park
2, Junjeong Choi
3, Keum-Seok Bae
2and Seong Joon Kang
2Department of Pathology1, Chungbuk National University College of Medicine, Cheongju, Departments of Surgery2 and Pathology3, Yonsei University Wonju College of Medicine, Wonju, Korea
A rare case of poorly differentiated thyroid carcinoma (PDTC) with gross intraluminal invasion to the internal jugular vein whose clinical manifestation was multiple lung metastases is described. A 66-year-old man was referred to the outpatient clinic of the Department of Internal Medicine, hemato-oncology subdivision for multiple lung nodules found by his regular health check-up. These lung nodules showed variable sizes with irregular shapes, and typical distributions throughout the parenchyma, which were consistent with metastatic nodules. Ultrasonography revealed a 4.5 cm sized hypoechoic mass with irregular shape in his left thyroid lobe and a huge thrombus in the left internal jugular vein. PDTCs associated with gross intraluminal invasion to the great cervical vein and multiple lung nodules as their first clinical manifestation are extremely rare. We would emphasize the importance of preoperative detailed evaluation of the disseminated disease by ultrasonography in suspected patients.
Key Words: Poorly differentiated thyroid carcinoma, Internal jugular vein, Lung, Invasion, Metastasis
Introduction
Poorly differentiated thyroid carcinomas (PDTCs) are tumors of intermediate biological aggressiveness, con- sistent with their intermediate differentiation. They ac- count for up to 10% of all thyroid cancers.1) Most PDTCs appear as solitary large thyroid mass, with or without concurrent enlarged regional lymph nodes, and lung and/or bone metastases are also relatively frequent at the time of diagnosis. Even though vas- cular invasion and distant metastasis are well-known characteristics of PDTCs, the cases associated with gross intraluminal invasion of internal jugular vein
found by preoperative ultrasonography and multiple lung metastases are extremely rare. Herein, we docu- mented our experience with a 66-year-old man who underwent surgical treatment for PDTC accompanied by macroscopic intraluminal invasion to the internal jugular vein with multiple lung metastases.
Case Report
A 66-year-old man was referred to Wonju Seve- rance Christian Hospital due to multiple lung nodules found during his regular health check-up. He had no remarkable previous medical history, but complained of mild malaise and 4 kg of weight loss during the re-
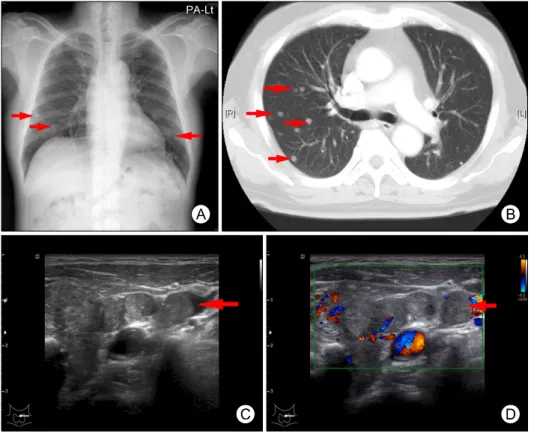
Fig. 1. Radiologic evalua- tions. Multiple small nodules (arrows) were found in lung parenchyma, which showed irregular shape, but well-de- fined border on simple chest X-ray (A) and chest CT scan (B). (C) Ultrasonography of transverse section of the left internal jugular vein. A solid tumor thrombus (arrow) in the lumen are shown. (D) With color Doppler ultrasono- graphy of a transverse sec- tion applied, Doppler signal of moving blood flow can be observed around the tumor thrombus (arrow) in the lu- men of the left internal jugular vein.
cent six months. On his simple chest X-ray, scattered nodules were found, and the chest computerized to- mography (CT) revealed multiple well-defined nodules in both lungs. The metastasis should be considered first of all. There were no specific findings on the gas- troenteroscopic and serologic evaluations except for the elevation of serum total T3 (7.3 ng/mL), free T4 level (8.5 ng/dL), and marked suppressed serum TSH level (0.01 U/mL) indicating hyperthyroidism. But he denied other symptoms such as palpitation, and visual disturbance. During the neck evaluation using ultra- sonography, 4.5 cm sized hypoechoic mass was found in his left thyroid lobe, which shaped irregularly and showed heterogeneous echotexture indicating macrocalcification. Furthermore, left internal jugular vein was directly invaded, and the blood flow was ob- structed by intraluminal heteroechoic mass on color Doppler, which was considered to be tumor thrombus (Fig. 1). Fine needle aspiration examination to left lobe mass in thyroid supported the possibility of the malig- nancy strongly. Torso PET/CT using F-18 FDG 10.4 mCi followed the ultrasonography and it revealed dif- fuse FDG uptake around the left internal jugular vein
and spotty uptake throughout the both lungs. But nei- ther abnormal uptake was recognized in the liver nor in the skeletons. The possibility of brain metastasis was ruled out using brain magnetic resonance imag- ing (MRI). He was prescribed with methimazole 30 mg daily for 2 weeks to regulate his hyperthyroidism, and finally total thyroidectomy and central compartment neck dissection (CCND) with segmental resection of the left internal jugular vein and partial resection of strap muscle were performed.
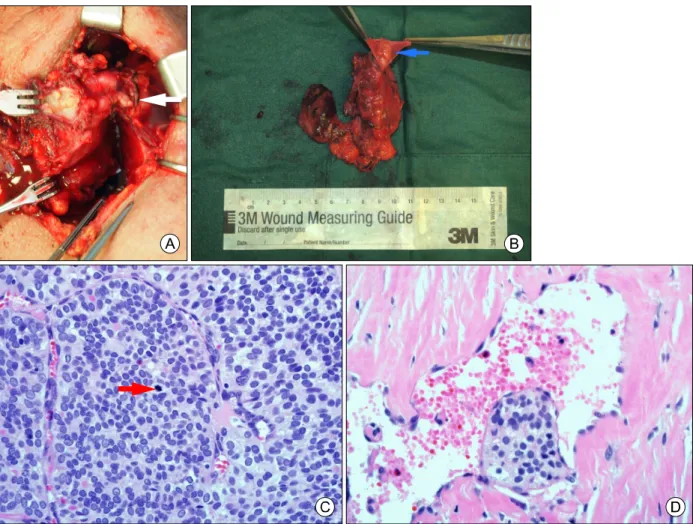
On gross examination, the left thyroid lobe was en- tirely replaced by hard 4.5×2×2 cm sized white to gray solid mass with extension to fibrous capsule ac- companied by multiple satellite nodules, which showed intraluminal tumor invasion of left internal jugular vein grossly.
Microscopic examination revealed an ill-defined solid lesion involving perithyroidal soft tissue and skel- etal muscle (pT3). The tumor cells demonstrated solid and insular growth pattern with frequent vascular in- vasion, and multifocal necrosis, but any metastasis was not identified in all six regional lymph nodes dis- sected (pN0). High magnification observations re-
Fig. 2. Intraoperative and microscopic features. (A) A gross intraluminal tumor thrombus (arrow) are shown with hard and whitish tumor mass in the left thyroid lobe. (B) After dissection, tumor thrombus (arrow) are clearly found in the lumen of left internal jugular vein. (C) The tumor has an insular pattern of growth with absence of conventional nuclear features of papillary carcinoma.
Atypical mitoses (up to 4/10 HPF, arrow) and (D) microscopic vascular invasion are detected (x400).
vealed large, hyperchromatic, and oval to round nuclei resembling that of follicular neoplasm with upto 4/10 HPF atypical mitoses, but lacking of intranuclear pseudo-inclusion and deep groove which are the cy- tologic characteristics of papillary thyroid carcinoma (Fig. 2). The immunohistochemical stain results of tu- mor cells were all negative for galactin-3 CK19, CD56, and PPAR-γ. Based on the above findings, poorly differentiated thyroid carcinoma was made for the final diagnosis. The patient underwent radioactive iodine (131I) ablation with a dose of 150 mCi and has been followed with no evidence of progression in lung nodules 9 months after surgery.
Discussion
Poorly differentiated thyroid carcinomas (PDTCs) were classified by WHO in 2004 as tumors of follicular cell origin that have morphologic and biologic charac- teristics intermediate between well-differentiated (papi- llary and follicular) thyroid carcinoma and anaplastic thyroid carcinoma.2)
When diagnosed, PDTCs are typically already at an advanced stage of disease, with extrathyroidal ex- tension and extensive local invasion.3) They have a tendency to metastasize to regional lymph nodes (50-85%), and distantly (36-85%), most commonly to the lung (14-54%), and bones (18-33%).4,5) Further- more, the 5-year, 10-year, and 15-year survival
rates are considerably lower in patients with PDTCs (50, 34, and 0%) than in patients with well differ- entiated thyroid carcinomas (95, 86, and 81%).6) In a recent review, the 5-year overall survival and disease specific survival (DSS) of PDTCs were 62% and 66%, respectively. The 5-year locoregional and distant control were 81% and 59%, respectively. Age ≥45 years, pathological tumor size >4 cm, extrathyroidal extension, higher pathological T stage, positive mar- gins, and distant metastases (M1) were predictive of worse DSS on univariate analysis. Multivariate analysis showed that only pT4a stage and M1 were inde- pendent predictors of worse DSS.7) In contrast to the PDTCs, anaplastic thyroid carcinoma is a highly ag- gressive neoplasm with a poor prognosis. The mortal- ity rate is >90%, with a mean survival of 6 months after diagnosis. Almost all patients complain of a rap- idly growing neck mass and symptoms associated with a large mass such as hoarseness, dysphagia, vocal cord paralysis, cervical pain, and dyspnea are the most frequent and important. The overall 5-year survival ranges from 0% to 14% and the median sur- vival is 4 to 12 months.8)
The rarity of this tumor makes it difficult to draw conclusions from the literature as to the best treatment option for PDTCs. However, aggressive management with total thyroidectomy and neck dissection followed by radioactive iodine remnant ablation is a standard treatment for PDTCs because of their aggressive na- ture with over 50% of PDTCs having regional nodal metastasis.2,9)
Invasion of the internal jugular or great cervical veins by thyroid carcinoma is rare and usually indi- cates the aggressive nature of the disease and a high probability of mortality.10,11) Therefore, appropriate vas- cular imaging should be done if angioinvasion is sus- pected. CT scan was reported to be useful for diag- nosing great vein thrombosis and its typical findings include a distended vein with an enhanced wall, a low-attenuated intraluminal filling defect, and adjacent soft tissue swelling.12) Color Doppler ultrasonography can help to diagnose great cervical vein invasion and plan surgical resection of the tumor. When internal jugular vein obstruction is found incidentally during
routine ultrasonographic evaluation of thyroid lesion, thyroid carcinoma infiltrating the internal jugular vein should be considered in the differential diagnosis.13) Kobayashi et al.14) retrospectively reviewed 7754 ca- ses undergoing thyroidectomy, and found the tumor thrombus, when detected in vessels around the neck by ultrasonography, increased the lung metastasis significantly (p<0.0001). Due to direct exposure of cancer cells to systemic circulation, it could be antici- pated that tumor thrombus in the vessel raises the possibility of lung metastasis. Therefore, the preopera- tive detection of a tumor thrombus on ultrasonography has a clinically important significance, and efforts sh- ould be made not only to localize and characterize thyroid lesion, but also to determine whether tumor thrombi are present.
Even though vascular invasion or angioinvasion is a well-documented microscopic feature of PDTCs, a review of English language literature showed that only three cases presenting gross intraluminal invasion of the internal jugular vein accompanied by multiple lung metastases have been reported.14-16)
In summary, we reported our experience with a 66-year-old man who underwent surgical treatment for PDTC accompanied by macroscopic intraluminal invasion to the internal jugular vein found by pre- operative ultrasonography with multiple lung metasta- ses. In general, PDTCs behave less aggressively than anaplastic thyroid carcinomas do, but when they show adjacent structural invasion or distant metastases, we would emphasize the importance of preoperative de- tailed evaluation by CT or ultrasonography for appro- priate treatments.
References
1) Patel KN, Shaha AR. Poorly differentiated thyroid cancer. Curr Opin Otolaryngol Head Neck Surg 2014;22(2):121-6.
2) Hod R, Bachar G, Sternov Y, Shvero J. Insular thyroid car- cinoma: a retrospective clinicopathologic study. Am J Otolaryn- gol 2013;34(4):292-5.
3) Bongiovanni M, Sadow PM, Faquin WC. Poorly diffe- rentiated thyroid carcinoma: a cytologic-histologic review. Adv Anat Pathol 2009;16(5):283-9.
4) Sanders EM Jr, LiVolsi VA, Brierley J, Shin J, Randolph GW.
An evidence-based review of poorly differentiated thyroid cancer.
World J Surg 2007;31(5):934-45.
5) Chao TC, Lin JD, Chen MF. Insular carcinoma: infrequent subtype of thyroid cancer with aggressive clinical course. World J Surg 2004;28(4):393-6.
6) Patel KN, Shaha AR. Poorly differentiated and anaplastic thyroid cancer. Cancer Control 2006;13(2):119-28.
7) Ibrahimpasic T, Ghossein R, Carlson DL, Nixon I, Palmer FL, Shaha AR, et al. Outcomes in patients with poorly diffe- rentiated thyroid carcinoma. J Clin Endocrinol Metab 2014;
99(4):1245-52.
8) Are C, Shaha AR. Anaplastic thyroid carcinoma: biology, pathogenesis, prognostic factors, and treatment approaches. Ann Surg Oncol 2006;13(4):453-64.
9) Wreesmann VB, Ghossein RA, Patel SG, Harris CP, Sch- naser EA, Shaha AR, et al. Genome-wide appraisal of thyroid cancer progression. Am J Pathol 2002;161(5):1549-56.
10) Onaran Y, Terzioglu T, Oguz H, Kapran Y, Tezelman S.
Great cervical vein invasion of thyroid carcinoma. Thyroid 1998;
8(1):59-61.
11) Lalak NJ, Campbell PR. Infiltrating papillary carcinoma of the thyroid with macroscopic extension into the internal jugular vein.
Otolaryngol Head Neck Surg 1997;117(6):S228-30.
12) Roh JL. Papillary thyroid carcinoma presenting a great vein invasion in the neck and upper chest. Otolaryngol Head Neck Surg 2006;135(5):818-20.
13) Thomas S, Sawhney S, Kapur BM. Case report: bilateral massive internal jugular vein thrombosis in carcinoma of the thyroid: CT evaluation. Clin Radiol 1991;43(6):433-4.
14) Kobayashi K, Hirokawa M, Yabuta T, Fukushima M, Kihara M, Higashiyama T, et al. Tumor thrombus of thyroid mali- gnancies in veins: importance of detection by ultrasonography.
Thyroid 2011;21(5):527-31.
15) Leong JL, Yuen HW, LiVolsi VA, Loevner L, Narula N, Baloch Z, et al. Insular carcinoma of the thyroid with jugular vein invasion. Head Neck 2004;26(7):642-6.
16) Donnellan KA, Carron JD, Bigler SA, Wein RO. Metastatic insular thyroid carcinoma in the pediatric patient. Am J Oto- laryngol 2009;30(1):61-4.