Intracorporeal Anastomosis in Laparoscopic Gastric Cancer Surgery
Hisahiro Hosogi, and Seiichiro Kanaya Department of Surgery, Osaka Red Cross Hospital, Osaka, Japan
Laparoscopic gastrectomy has become widely used as a minimally invasive technique for the treatment of gastric cancer. When it was first introduced, most surgeons preferred a laparoscopic-assisted approach with a minilaparotomy rather than a totally laparoscopic pro- cedure because of the technical challenges of achieving an intracorporeal anastomosis. Recently, with improved skills and instruments, several surgeons have reported the safety and feasibility of a totally laparoscopic gastrectomy with intracorporeal anastomosis. This review describes the recent technical advances in intracorporeal anastomoses using circular and linear staplers that allow for totally lapa- roscopic distal, total, and proximal gastrectomies. Data that demonstrate advantages in early surgical outcomes of a total laparoscopic method compared to laparoscopic-assisted operations are also discussed.
Key Words: Intracorporeal anastomosis; Laparoscopic distal gastrectomy; Laparoscopic total gastrectomy; Circular stapler; Linear stapler
Correspondence to: Seiichiro Kanaya
Department of Surgery, Osaka Red Cross Hospital, 5-30, Fudegasaki, Tennouji-ku, Osaka 543-8555, Japan
Tel: +81-6-6774-5111, Fax: +81-6-6774-5131 E-mail: skanaya@osaka-med.jrc.or.jp Received July 12, 2012
Revised July 18, 2012 Accepted July 18, 2012
Copyrights © 2012 by The Korean Gastric Cancer Association www.jgc-online.org
This is an open-access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/
licenses/by-nc/3.0) which permits unrestricted noncommercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Introduction
Since the first laparoscopic gastrectomy was described by Goh et al.(1) in 1992, the safety and feasibility of laparoscopic gastrecto- my in the treatment of early gastric cancer have been demonstrat- ed.(2,3) Reported advantages of laparoscopic gastrectomy compared to open gastrectomy include improved cosmesis, less pain, earlier recovery, and better quality of life. According to the Korean Gastric Cancer Association, 1,089 cases of laparoscopic gastric surgery were performed in 2004.(4) In Japan, more than 1,500 gastrectomies were performed laparoscopically in 2003.(3)
Many of those resections were performed by a laparoscopic- assisted technique that requires a mini-laparotomy, mainly for anastomosing the bowel. More recently, several methods of
intracorporeal anastomosis have been used not only for laparo- scopic distal gastrectomy (LDG), but also for laparoscopic total gastrectomy (LTG) and laparoscopic proximal gastrectomy (LPG).
These advances allow a gastrectomy to be performed by a totally laparoscopic approach. In this review, we describe the recent tech- nical innovations and the early surgical outcomes of intracorporeal anastomosis in gastric cancer surgery.
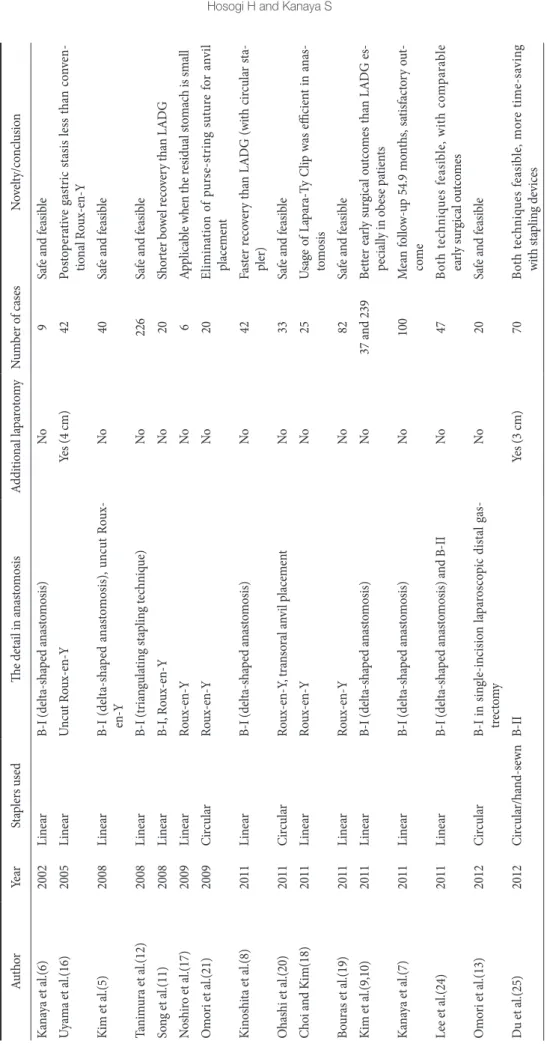
LDG (Table 1)
1. Billroth-I anastomosis
In both Korea and Japan, many surgeons tend to choose Billroth- I anastomosis following distal gastrectomy. Because of the technical difficulty of intracorporeal gastroduodenostomy, most surgeons have preferred laparoscopy-assisted distal gastrectomy (LADG) rather than totally laparoscopic distal gastrectomy (TLDG).(5) In 1992, we developed a simple and secure method of intracorporeal gastroduodenostomy, using only endoscopic linear staplers, which we have named the delta-shaped anastomosis.(6) This technique creates a functional end-to-end anastomosis between the posterior wall of the stomach and the duodenal bulb. Because of its advan-
Table 1. Previous reports of intracorporeal anastomosis in laparoscopic distal gastrectomy AuthorYearStaplers usedThe detail in anastomosisAdditional laparotomyNumber of casesNovelty/conclusion Kanaya et al.(6)2002LinearB-I (delta-shaped anastomosis)No9Safe and feasible Uyama et al.(16)2005LinearUncut Roux-en-YYes (4 cm)42Postoperative gastric stasis less than conven- tional Roux-en-Y Kim et al.(5)2008LinearB-I (delta-shaped anastomosis), uncut Roux- en-YNo40Safe and feasible Tanimura et al.(12)2008LinearB-I (triangulating stapling technique)No226Safe and feasible Song et al.(11)2008LinearB-I, Roux-en-YNo20Shorter bowel recovery than LADG Noshiro et al.(17)2009LinearRoux-en-YNo6Applicable when the residual stomach is small Omori et al.(21)2009CircularRoux-en-YNo20Elimination of purse-string suture for anvil placement Kinoshita et al.(8)2011LinearB-I (delta-shaped anastomosis)No42Faster recovery than LADG (with circular sta- pler) Ohashi et al.(20)2011CircularRoux-en-Y, transoral anvil placementNo33Safe and feasible Choi and Kim(18)2011LinearRoux-en-YNo25Usage of Lapara-Ty Clip was efficient in anas- tomosis Bouras et al.(19)2011LinearRoux-en-YNo82Safe and feasible Kim et al.(9,10)2011LinearB-I (delta-shaped anastomosis)No37 and 239Better early surgical outcomes than LADG es- pecially in obese patients Kanaya et al.(7)2011LinearB-I (delta-shaped anastomosis)No100Mean follow-up 54.9 months, satisfactory out- come Lee et al.(24)2011LinearB-I (delta-shaped anastomosis) and B-IINo47Both techniques feasible, with comparable early surgical outcomes Omori et al.(13)2012CircularB-I in single-incision laparoscopic distal gas- trectomyNo20Safe and feasible Du et al.(25)2012Circular/hand-sewnB-IIYes (3 cm)70Both techniques feasible, more time-saving with stapling devices B-I = Billroth-I; LADG = laparoscopy assisted distal gastrectomy; B-II = Billroth-II.
tages, this procedure is gaining widespread acceptance among sur- geons in Japan and Korea, where it is becoming a standard recon- struction procedure in LDG.(5-10) Recently we reported the short and long-term outcomes of the initial 100 consecutive cases with a mean follow-up period of 54.9 months.(7) The learning curve for the surgeons was steep; mean time to perform the anastomosis was 13 minutes. One patient developed a minor anastomotic leak, and another suffered from postoperative dumping syndrome. Two- thirds of the patients tolerated a 1,500 kcal/day soft diet at the time of discharge. According to these results, we concluded that the delta-shaped anastomosis is safe, simple, and provides satisfactory postoperative outcomes.
With the acceptance of our delta-shaped anastomosis, several retrospective analyses comparing early surgical outcomes of TLDG using delta-shaped anastomosis with those of LADG have been reported.(8-11) In all of these studies, the reconstruction in LADG was performed with extracorporeal Billroth-I anastomosis, with a circular stapler. In TLDG groups the umbilical wound was ex- tended up to 3 cm for specimen extraction, while in LADG groups, a 4~6 cm mid-line incision in the epigastrium was added. Early postoperative outcomes, such as blood loss, return of gastroin- testinal function, pain scores, and hospital stay were significantly improved in TLDG compared with LADG.(9,10) Furthermore, in obese patients overall complication rates were significantly lower in TLDG than in LADG.(9) In performing LADG, the extracorporeal anastomosis that is done through a small incision can cause exces- sive traction on the organs and increase operative manipulation, especially in obese patients. To the contrary, in an intracorporeal anastomosis, direct visualization by laparoscopy provides a better operative field and minimizes surgical trauma; these advantages are also independent of body habitus.
Other techniques for intracorporeal Billroth-I anastomosis have been reported. Tanimura et al.(12) described a triangulating stapling technique with linear staplers. The posterior walls of the stomach and duodenal bulb are stapled in an inverted fashion, and the ante- rior walls are stapled with 2 staplers in an everted manner, making the shape of the anastomosis triangular. They reported on the fea- sibility of this procedure with their 111 cases experience. Omori et al.(13) described an intracorporeal circular-stapled Billroth-I anas- tomosis in a single-incision laparoscopic operation. They obviated the need for a purse-string suture for anvil head insertion into the duodenal bulb, and safely employed the technique in 20 patients.
The long-term surgical outcomes for these procedures are ex- pected.
2. Roux-en-Y anastomosis
Roux-en-Y reconstruction is another option for distal gastrec- tomy, with the advantage of less bile reflux into the gastric remnant or reflux esophagitis. Similarly in LADG, Roux-en-Y reconstruc- tion provided better surgical outcomes than Billroth-I reconstruc- tion, preventing postoperative complications (i.e. anastomotic leak or stricture) and bile reflux into the gastric remnant.(14) However, long-term follow-up is still necessary, because Roux-en-Y gas- trojejunostomies are considered relatively ulcerogenic.(15) There are other disadvantages as well: any subsequent need for endoscopic access to the ampulla of Vater is more difficult, and Roux-stasis syndrome, a unique complication of this procedure, may occur.
Regarding the anastomotic techniques, both linear staplers(16-18) and circular staplers(19,20) have been reported with successful re- sults. The uncut Roux-en-Y method using a linear stapler provided better results in preventing Roux-stasis syndrome.(16) Noshiro et al.(17) reported a novel stapling technique with linear staplers that is possible when the residual stomach is small. Circular stapling tech- niques have been used by transoral anvil placement.(20) Elimina- tion of the purse-string suture has also been described.(21) Long- term follow-up results with larger number of patients are expected.
3. Billroth-II anastomosis
Billroth-II anastomosis is another standard method of recon- struction, although there are some concerns of gastric remnant car- cinogenesis due to alkaline reflux gastritis.(22,23) There are reports using both linear(16,24) and circular staplers.(25) When using linear staplers, care must be taken to avoid stricturing of the efferent loop of the jejunum, especially when the entry hole is closed with a stapler.(16) Uyama et al.(16) make the enterotomy on the afferent loop and perform an antiperistaltic Billroth-II anastomosis, placing some stitches between the afferent loop and the lesser curvature of the gastric remnant to prevent food from flowing into the affer- ent loop. We think these concepts are reasonable, and may provide better surgical outcomes for patients.
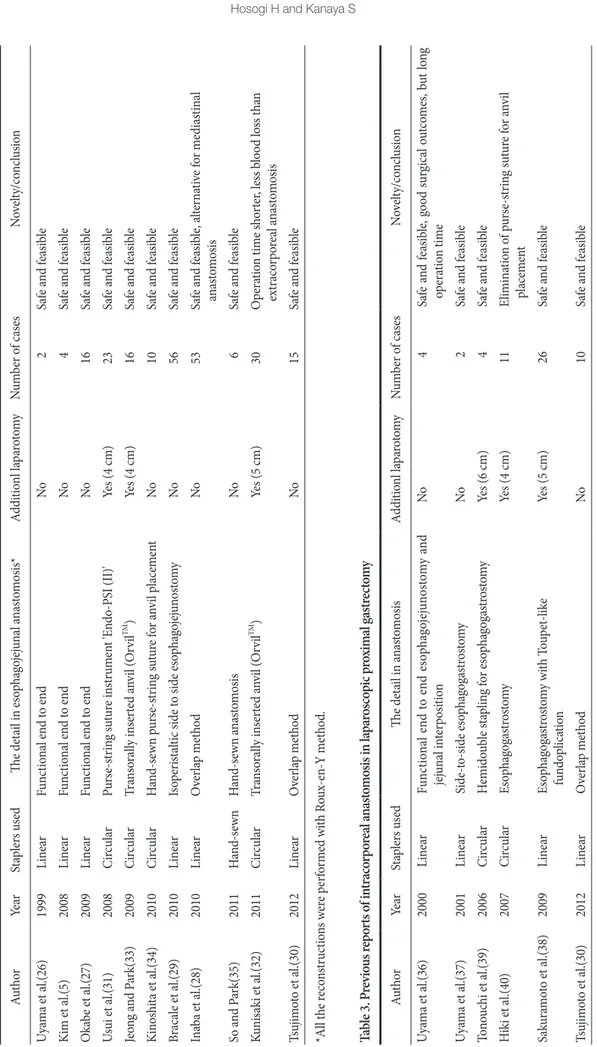
LTG (Table 2)
LTG with intracorporeal anastomosis has been utilized less than LDG because of the technical difficulty of esophagojejunos- tomy. Since 1999, however, some novel techniques to achieve a safe esophagojejunostomy have been reported with good outcomes, both with linear and circular staplers.(5,26-33)
Table 3. Previous reports of intracorporeal anastomosis in laparoscopic proximal gastrectomy AuthorYearStaplers usedThe detail in anastomosisAdditionl laparotomyNumber of casesNovelty/conclusion Uyama et al.(36)2000LinearFunctional end to end esophagojejunostomy and jejunal interpositionNo 4Safe and feasible, good surgical outcomes, but long operation time Uyama et al.(37)2001LinearSide-to-side esophagogastrostomyNo 2Safe and feasible Tonouchi et al.(39)2006CircularHemidouble stapling for esophagogastrostomyYes (6 cm) 4Safe and feasible Hiki et al.(40)2007CircularEsophagogastrostomyYes (4 cm)11Elimination of purse-string suture for anvil placement Sakuramoto et al.(38)2009LinearEsophagogastrostomy with Toupet-like fundoplicationYes (5 cm)26Safe and feasible Tsujimoto et al.(30)2012LinearOverlap methodNo10Safe and feasible Table 2. Previous reports of intracorporeal anastomosis in laparoscopic total gastrectomy AuthorYearStaplers usedThe detail in esophagojejunal anastomosis*Additionl laparotomyNumber of casesNovelty/conclusion Uyama et al.(26)1999LinearFunctional end to endNo 2Safe and feasible Kim et al.(5)2008LinearFunctional end to endNo 4Safe and feasible Okabe et al.(27)2009LinearFunctional end to endNo16Safe and feasible Usui et al.(31)2008CircularPurse-string suture instrument 'Endo-PSI (II)'Yes (4 cm)23Safe and feasible Jeong and Park(33)2009CircularTransorally inserted anvil (OrvilTM )Yes (4 cm)16Safe and feasible Kinoshita et al.(34)2010CircularHand-sewn purse-string suture for anvil placementNo10Safe and feasible Bracale et al.(29)2010LinearIsoperistaltic side to side esophagojejunostomyNo56Safe and feasible Inaba et al.(28)2010LinearOverlap methodNo53Safe and feasible, alternative for mediastinal anastomosis So and Park(35)2011Hand-sewnHand-sewn anastomosisNo 6Safe and feasible Kunisaki et al.(32)2011CircularTransorally inserted anvil (OrvilTM )Yes (5 cm)30Operation time shorter, less blood loss than extracorporeal anastomosis Tsujimoto et al.(30)2012LinearOverlap methodNo15Safe and feasible *All the reconstructions were performed with Roux-en-Y method.
1. Esophagojejunostomy with linear staplers
Functional end-to-end anastomoses for esophagojejunostomy have been reported.(5,26-27) One technique is fashioning an an- tiperistaltic side-to-side anastomosis between the left dorsal side of the esophagus and the jejunal limb. The entry hole was also closed with staplers.(26,27) A nasogastric tube, as an insertion guide to the esophageal lumen, was quite helpful for identification of the lumen.(27) An isoperistaltic esophagojejunostomy, the so- called ‘Overlap method’ has also been reported,(28-30) in which the entry hole was closed with intracorporeal hand-sewn sutures.
Because the anastomosis is made in an isoperistaltic manner, the jejunal limb straightens, which may be advantageous when the anastomosis is located in the confined mediastinal space.(28)
2. Esophagojejunostomy with a circular stapler The esophagojejunostomy with a circular stapler is a com- mon method in conventional open total gastrectomy, and surgeons are familiar with this procedure. However, it is often difficult to complete circular-stapled esophagojejunostomy through a mini- laparotomy, because inserting and/or fixing the anvil in a nar- row and deep operative field can be difficult, especially in obese patients. With improvements of surgeons’ skills and dedicated devices, an intracorporeal circular-stapled anastomosis has become more practical. Novel procedures include an endoscopic purse- string suture instrument ‘Endo-PSI(II)’,(31) transorally inserted anvil (OrvilTM, Covidien, Mansfield, MA, USA),(32,33) hand-sewn purse-string suturing techniques,(34) and hand-sewn esophagoje- junostomy(35) have been developed. The insertion and fixation of the anvil becomes easier with these devices and techniques. Early surgical outcomes using the OrvilTM have been reported. Operative time and blood loss were reduced compared to anastomosis with mini-laparotomy.(32) Adequate extension of the neck, appropriate selection of the anvil head,(32) and caution in the insertion of the anvil, to prevent larynx or esophageal injury, are crucial. Preventing abdominal infection is also important when using OrvilTM.(33)
Techniques with both linear and circular staplers in LTG seem feasible, but most of the data are technical reports with a limited number of patients. Further study including larger number of pa- tients, and comparison studies with other techniques measuring short-term and long-term surgical outcomes are warranted to evaluate these anastomotic procedures.
LPG (Table 3)
Several techniques of performing intracorporeal anastomosis in
LPG have been reported.(36) Intracorporeal anastomosis with jeju- nal interposition was first reported in 2000,(36) but seemed compli- cated and time-consuming. Esophagogastrostomy with linear sta- plers(37,38) and circular staplers(39,40) have been reported but no standardized techniques have been established. To achieve a secure anastomosis with satisfactory postoperative quality of life, the addi- tion of an antireflux procedure is necessary to prevent postopera- tive regurgitive esophagitis. Wrapping the anastomosis, or creating a new notch corresponding to the normal cardiac notch to form a flap valve, is necessary as an antireflux procedure. In previous reports,(37,38) anastomosis was made between the posterior wall of the esophagus and the anterior wall of the remnant stomach, which created a new cardiac notch at the dorsal side of the anastomosis.
Sakuramoto et al.(38) added a Toupet-like partial fundoplication.
We recently developed a novel method of esophagogastric-tube reconstruction with stapled fundoplication for LPG (unpublished data). In this method, the left dorsal side of the esophagus and the anterior wall of the gastric-tube were connected with a 45 mm no- knife stapler in the isoperistaltic manner similar to the ‘Overlap method’.(28,30) The common lumen was created by cutting the center of the staple rows for a length of 15 mm, followed by the closure of the entry hole with interrupted sutures. The remaining connected stomach along the uncut 30 mm staple line functions as a pseudo-fornix, forming an acute angle that attempts to re- create an angle of His. By using a long gastric-tube, a tension-free anastomosis is possible even with bulky tumors invading the distal esophagus. Eight patients with Siewert type II adenocarcinoma of the esophagogastric junction underwent this procedure with good results. We have proposed this procedure as an alternative in LPG, especially for Siewert type II adenocarcinoma of the esophagogas- tric junction.
Reports on intracorporeal esophagogastrostomy for LPG are still limited, and further clinical studies evaluating surgical outcomes and postoperative quality of life are necessary.
Conclusions
In this review, recent reports regarding intracorporeal anas- tomosis in laparoscopic gastric cancer operations were reviewed.
These innovations are causing a shift from ‘laparoscopy-assisted’ to
‘totally laparoscopic’, and the surgeons’ skills and instruments are still developing. Further clinical studies evaluating the procedures in large number of patients are necessary to provide solid evidence to determine the place of intracorporeal anastomosis in laparoscopic gastric cancer surgery.
References
1. Goh P, Tekant Y, Isaac J, Kum CK, Ngoi SS. The technique of laparoscopic Billroth II gastrectomy. Surg Laparosc Endosc 1992;2:258-260.
2. Kim MC, Kim KH, Kim HH, Jung GJ. Comparison of lapa- roscopy-assisted by conventional open distal gastrectomy and extraperigastric lymph node dissection in early gastric cancer. J Surg Oncol 2005;91:90-94.
3. Shiraishi N, Yasuda K, Kitano S. Laparoscopic gastrectomy with lymph node dissection for gastric cancer. Gastric Cancer 2006;9:167-176.
4. Kim HH, Kim KH, Kim DH, Kim C, Kim BS, Kim YW, et al;
Korean Laparoscopic Gastrointestinal Surgery Study Group.
Nationwide survey of laparoscopic gastric surgery in Korea, 2004. J Korean Gastric Cancer Assoc 2005;5:295-303.
5. Kim JJ, Song KY, Chin HM, Kim W, Jeon HM, Park CH, et al.
Totally laparoscopic gastrectomy with various types of intra- corporeal anastomosis using laparoscopic linear staplers: pre- liminary experience. Surg Endosc 2008;22:436-442.
6. Kanaya S, Gomi T, Momoi H, Tamaki N, Isobe H, Katayama T, et al. Delta-shaped anastomosis in totally laparoscopic Billroth I gastrectomy: new technique of intraabdominal gastroduode- nostomy. J Am Coll Surg 2002;195:284-287.
7. Kanaya S, Kawamura Y, Kawada H, Iwasaki H, Gomi T, Satoh S, et al. The delta-shaped anastomosis in laparoscopic distal gastrectomy: analysis of the initial 100 consecutive proce- dures of intracorporeal gastroduodenostomy. Gastric Cancer 2011;14:365-371.
8. Kinoshita T, Shibasaki H, Oshiro T, Ooshiro M, Okazumi S, Katoh R. Comparison of laparoscopy-assisted and total lapa- roscopic Billroth-I gastrectomy for gastric cancer: a report of short-term outcomes. Surg Endosc 2011;25:1395-1401.
9. Kim MG, Kawada H, Kim BS, Kim TH, Kim KC, Yook JH, et al. A totally laparoscopic distal gastrectomy with gastroduode- nostomy (TLDG) for improvement of the early surgical out- comes in high BMI patients. Surg Endosc 2011;25:1076-1082.
10. Kim MG, Kim KC, Kim BS, Kim TH, Kim HS, Yook JH, et al.
A totally laparoscopic distal gastrectomy can be an effective way of performing laparoscopic gastrectomy in obese patients (body mass index≥30). World J Surg 2011;35:1327-1332.
11. Song KY, Park CH, Kang HC, Kim JJ, Park SM, Jun KH, et al.
Is totally laparoscopic gastrectomy less invasive than laparos- copy-assisted gastrectomy?: prospective, multicenter study. J
Gastrointest Surg 2008;12:1015-1021.
12. Tanimura S, Higashino M, Fukunaga Y, Takemura M, Nishika- wa T, Tanaka Y, et al. Intracorporeal Billroth 1 reconstruction by triangulating stapling technique after laparoscopic distal gastrectomy for gastric cancer. Surg Laparosc Endosc Percutan Tech 2008;18:54-58.
13. Omori T, Tanaka K, Tori M, Ueshima S, Akamatsu H, Nishida T. Intracorporeal circular-stapled Billroth I anastomosis in single-incision laparoscopic distal gastrectomy. Surg Endosc 2012;26:1490-1494.
14. Kojima K, Yamada H, Inokuchi M, Kawano T, Sugihara K. A comparison of Roux-en-Y and Billroth-I reconstruc- tion after laparoscopy-assisted distal gastrectomy. Ann Surg 2008;247:962-967.
15. Fischer JE, Bland KI, Callery MP, eds. Mastery of Surgery.
Philadelphia: Lippincott Williams & Wilkins, 2007.
16. Uyama I, Sakurai Y, Komori Y, Nakamura Y, Syoji M, Tono- mura S, et al. Laparoscopy-assisted uncut Roux-en-Y opera- tion after distal gastrectomy for gastric cancer. Gastric Cancer 2005;8:253-257.
17. Noshiro H, Ohuchida K, Kawamoto M, Ishikawa M, Uchiyama A, Shimizu S, et al. Intraabdominal Roux-en-Y reconstruction with a novel stapling technique after laparoscopic distal gas- trectomy. Gastric Cancer 2009;12:164-169.
18. Choi YY, Kim YJ. Intracorporeal anastomosis using a Lapra-ty clip in laparoscopic distal gastrectomy: initial clinical experi- ences. J Laparoendosc Adv Surg Tech A 2011;21:51-55.
19. Bouras G, Lee SW, Nomura E, Tokuhara T, Nitta T, Yoshinaka R, et al. Surgical outcomes from laparoscopic distal gastrec- tomy and Roux-en-Y reconstruction: evolution in a totally intracorporeal technique. Surg Laparosc Endosc Percutan Tech 2011;21:37-41.
20. Ohashi M, Iwanaga T, Ohinata R, Kanda T, Iwasaki Y. A novel procedure for Roux-en-Y reconstruction following laparos- copy-assisted distal gastrectomy: transoral placement of anvil and intracorporeal gastrojejunostomy via umbilical mini- laparotomy. Gastric Cancer 2011;14:188-193.
21. Omori T, Oyama T, Akamatsu H, Tori M, Ueshima S, Nakaha- ra M, et al. A simple and safe method for gastrojejunostomy in laparoscopic distal gastrectomy using the hemidouble-stapling technique: efficient purse-string stapling technique. Dig Surg 2009;26:441-445.
22. Caygill CP, Hill MJ, Kirkham JS, Northfield TC. Mortality from gastric cancer following gastric surgery for peptic ulcer. Lancet
1986;1:929-931.
23. Lundegårdh G, Adami HO, Helmick C, Zack M, Meirik O.
Stomach cancer after partial gastrectomy for benign ulcer dis- ease. N Engl J Med 1988;319:195-200.
24. Lee HW, Kim HI, An JY, Cheong JH, Lee KY, Hyung WJ, et al.
Intracorporeal anastomosis using linear stapler in laparoscopic distal gastrectomy: comparison between gastroduodenostomy and gastrojejunostomy. J Gastric Cancer 2011;11:212-218.
25. Du J, Shuang J, Li J, Zhao Q, Hong L, Du X, et al. Totally lapa- roscopic Billroth II gastrectomy with a novel, safe, simple, and time-saving anastomosis by only stapling devices. J Gastroin- test Surg 2012;16:738-743.
26. Uyama I, Sugioka A, Fujita J, Komori Y, Matsui H, Hasumi A.
Laparoscopic total gastrectomy with distal pancreatosplenec- tomy and D2 lymphadenectomy for advanced gastric cancer.
Gastric Cancer 1999;2:230-234.
27. Okabe H, Obama K, Tanaka E, Nomura A, Kawamura J, Na- gayama S, et al. Intracorporeal esophagojejunal anastomosis after laparoscopic total gastrectomy for patients with gastric cancer. Surg Endosc 2009;23:2167-2171.
28. Inaba K, Satoh S, Ishida Y, Taniguchi K, Isogaki J, Kanaya S, et al. Overlap method: novel intracorporeal esophagojeju- nostomy after laparoscopic total gastrectomy. J Am Coll Surg 2010;211:e25-29.
29. Bracale U, Marzano E, Nastro P, Barone M, Cuccurullo D, Cu- tini G, et al. Side-to-side esophagojejunostomy during totally laparoscopic total gastrectomy for malignant disease: a multi- center study. Surg Endosc 2010;24:2475-2479.
30. Tsujimoto H, Uyama I, Yaguchi Y, Kumano I, Takahata R, Mat- sumoto Y, et al. Outcome of overlap anastomosis using a linear stapler after laparoscopic total and proximal gastrectomy. Lan- genbecks Arch Surg 2012;397:833-840.
31. Usui S, Nagai K, Hiranuma S, Takiguchi N, Matsumoto A, Sanada K. Laparoscopy-assisted esophagoenteral anastomosis using endoscopic purse-string suture instrument “Endo-PSI (II)” and circular stapler. Gastric Cancer 2008;11:233-237.
32. Kunisaki C, Makino H, Oshima T, Fujii S, Kimura J, Takagawa R, et al. Application of the transorally inserted anvil (OrVil) after laparoscopy-assisted total gastrectomy. Surg Endosc 2011;25:1300-1305.
33. Jeong O, Park YK. Intracorporeal circular stapling esophago- jejunostomy using the transorally inserted anvil (OrVil) after laparoscopic total gastrectomy. Surg Endosc 2009;23:2624- 2630.
34. Kinoshita T, Oshiro T, Ito K, Shibasaki H, Okazumi S, Katoh R. Intracorporeal circular-stapled esophagojejunostomy using hand-sewn purse-string suture after laparoscopic total gastrec- tomy. Surg Endosc 2010;24:2908-2912.
35. So KO, Park JM. Totally laparoscopic total gastrectomy using intracorporeally hand-sewn esophagojejunostomy. J Gastric Cancer 2011;11:206-211.
36. Uyama I, Sugioka A, Fujita J, Komori Y, Matsui H, Hasumi A. Completely laparoscopic proximal gastrectomy with je- junal interposition and lymphadenectomy. J Am Coll Surg 2000;191:114-119.
37. Uyama I, Sugioka A, Matsui H, Fujita J, Komori Y, Hatakawa Y, et al. Laparoscopic side-to-side esophagogastrostomy us- ing a linear stapler after proximal gastrectomy. Gastric Cancer 2001;4:98-102.
38. Sakuramoto S, Yamashita K, Kikuchi S, Futawatari N, Katada N, Moriya H, et al. Clinical experience of laparoscopy-assisted proximal gastrectomy with Toupet-like partial fundoplication in early gastric cancer for preventing reflux esophagitis. J Am Coll Surg 2009;209:344-351.
39. Tonouchi H, Mohri Y, Tanaka K, Kobayashi M, Kusunoki M.
Hemidouble stapling for esophagogastrostomy during laparo- scopically assisted proximal gastrectomy. Surg Laparosc En- dosc Percutan Tech 2006;16:242-244.
40. Hiki N, Fukunaga T, Yamaguchi T, Nunobe S, Tokunaga M, Ohyama S, et al. Laparoscopic esophagogastric circular stapled anastomosis: a modified technique to protect the esophagus.
Gastric Cancer 2007;10:181-186.