INTRODUCTION
Hepatic hydrothorax (HH) is a complication of advanced cir- rhosis characterized by transudative pleural effusion in the absence of underlying cardiac or pulmonary disease, with an estimated rate of 5–10% in cirrhotic patients.1 HH results from pathologic trans-diaphragmatic migration of ascitic fluid in patients with liver cirrhosis.2 In one study, HH was right-sided in 70% of cases, left-sided in 18%, and bilateral in 12%.1 Patients with minimal pleural effusion may be asymptomatic or have pulmonary symptoms of dyspnea, cough, chest discomfort, hy- poxemia, or respiratory failure. They are prone to recurrent bouts of spontaneous bacterial pleuritis with or without con- current spontaneous bacterial peritonitis. Ascites usually pres-
Various Treatment Modalities in Hepatic Hydrothorax:
What Is Safe and Effective?
Jae Hyun Yoon
1*, Hee Joon Kim
2*, Chung Hwan Jun
1, Sung Bum Cho
3, Yochun Jung
4, and Sung Kyu Choi
1Departments of 1Gastroenterology and Hepatology, and 2Surgery, Chonnam National University Hospital, Chonnam National University Medical School, Gwangju;
3Department of Gastroenterology and Hepatology, Chonnam National University Hwasun Hospital, Chonnam National University Medical School, Hwasun;
4Department of Thoracic and Cardiovascular Surgery, Chonnam National University Hospital, Chonnam National University Medical School, Gwangju, Korea.
Purpose: Hepatic hydrothorax is a complication of decompensated liver cirrhosis that is difficult and complex to manage. Data concerning the optimal treatment method, other than liver transplantation, are limited. This study aimed to compare the clinical features and outcomes of patients treated with various modalities, while focusing on surgical management and pigtail drainage.
Materials and Methods: Forty-one patients diagnosed with refractory hepatic hydrothorax between January 2013 and December 2017 were enrolled.
Results: The mean Child-Turcotte-Pugh and model for end stage liver disease scores of the enrolled patients were 10.1 and 19.7, respectively. The patients underwent four modalities: serial thoracentesis (n=11, 26.8%), pigtail drainage (n=16, 39.0%), surgery (n=10, 24.4%), and liver transplantation (n=4, 9.8%); 12-month mortality rate/median survival duration was 18.2%/868 days, 87.5%/79 days, 70%/179 days, and 0%/601.5 days, respectively. Regarding the management of refractory hepatic hydrothorax, surgery group required less frequent needle puncture (23.5 times in pigtail group vs. 9.3 times in surgery group), had a lower oc- currence of hepatorenal syndrome (50% vs. 30%), and had a non-inferior cumulative overall survival (402.1 days vs. 221.7 days) compared to pigtail group. On multivariate analysis for poor survival, body mass index <19 kg/m2, refractory hepatic hydrothorax not managed with liver transplantation, Child-Turcotte-Pugh score >10, and history of severe encephalopathy (grade >2) were as- sociated with poor survival.
Conclusion: Serial thoracentesis may be recommended for management of hepatic hydrothorax and surgical management can be a useful option in patients with refractory hepatic hydrothorax, alternative to pigtail drainage.
Key Words: Cirrhosis, drainage, hydrothorax, surgery
pISSN: 0513-5796 · eISSN: 1976-2437
Received: June 26, 2019 Revised: August 14, 2019 Accepted: August 19, 2019
Co-corresponding authors: Sung Kyu Choi, MD, PhD, Department of Gastroen- terology and Hepatology, Chonnam National University Hospital, Chonnam Na- tional University Medical School, 42 Jebong-ro, Dong-gu, Gwangju 61469, Korea.
Tel: 82-62-220-6296, Fax: 82-62-220-8578, E-mail: choisk@jnu.ac.kr and Yochun Jung, MD, PhD, Department of Thoracic and Cardiovascular Surgery, Chon- nam National University Hospital, Chonnam National University Medical School, 42 Jebong-ro, Dong-gu, Gwangju 61469, Korea.
Tel: 82-62-220-6547, Fax: 82-62-220-1636, E-mail: yochuni@naver.com
*Jae Hyun Yoon and Hee Joon Kim contributed equally to this work.
•The authors have no potential conflicts of interest to disclose.
© Copyright: Yonsei University College of Medicine 2019
This is an Open Access article distributed under the terms of the Creative Com- mons Attribution Non-Commercial License (https://creativecommons.org/licenses/
by-nc/4.0) which permits unrestricted non-commercial use, distribution, and repro- duction in any medium, provided the original work is properly cited.
Yonsei Med J 2019 Oct;60(10):944-951 https://doi.org/10.3349/ymj.2019.60.10.944
ents in HH; therefore, patients with HH have poor underlying liver function.3 The development of HH represents progres- sion to decompensated cirrhosis and warrants prompt con- sideration for liver transplantation (LT).4
Although LT is the optimal treatment modality for HH, it has poor accessibility due to donor organ shortage.5 Long-term management of HH using methods other than LT is challeng- ing, due to the underlying poor liver function and lack of clini- cal trials supporting a satisfactory therapy. Medical therapy with diuretics, as well as a low-salt diet, repeated thoracente- sis, pigtail drainage, transjugular intrahepatic portosystemic shunt (TIPS), and surgery have been reported for the manage- ment of HH.6 However, no large-scale studies have determined the optimal treatment modality, other than LT, for patients with HH. Therefore, this study aimed to identify the clinical characteristics and outcomes of cirrhotic patients with HH un- dergoing various modalities, such as medical treatment, re- peated thoracentesis, pigtail drainage, and surgery.
MATERIALS AND METHODS
Patients
The inclusion criteria were age ≥18 years, diagnosis of liver cirrhosis, and refractory HH occurring between January 2013 and December 2017. Since surgery for HH has been available since 2013 at our center, we included all patients who were di- agnosed with HH within the study period. HH was defined as large transudative pleural effusion (>500 mL) in a patient in whom other causes, such as heart failure, pneumonia, and malignancy, had been excluded. Data were collected from hospital records, and data on mortality and cause of death were obtained using the Statistics Korea microdata integrated service (https://mdis.kostat.go.kr). The institutional review board committee of Chonnam National University Hospital (CNUH-2018-132) approved the study protocol, and the re- quirement for informed consent was waived as patient data were de-identified.
Pleural fluid analysis
All patients underwent more than one thoracentesis, and all samples of pleural fluid obtained initially were examined.
Routine pleural fluid and serum examinations included cell counts with differential counts, gram stains, cultures, pleural fluid pH, serum and fluid protein levels, albumin level, biliru- bin level, and lactate dehydrogenase (LDH) level.
Transudate pleural fluid was defined as having either a pleural fluid/serum protein ratio ≤0.5, a pleural fluid/serum LDH ratio ≤0.6, or a pleural fluid LDH level less than two-thirds of the upper limit of normal for serum LDH. Serum-pleural flu- id analysis gradient was defined as the difference in albumin levels between serum and pleural fluid.
Treatment modalities
Patient groups were defined using four different treatment modalities. Serial thoracentesis group included patients who had at least more than two therapeutic thoracentesis without other treatment modalities and were on continuous diuretics therapy. The median time interval between consecutive tho- racenteses was calculated in this group.
Pigtail drainage group included patients who had a pigtail catheter inserted using Seldinger technique and were on con- tinuous diuretic therapy. Pigtail catheter was maintained for continuous drainage of pleural effusion, and re-insertion/re- moval was performed according to clinical requirements.
Usually, thoracentesis was routinely performed before pigtail drainage for evaluation and initial management of hydrotho- rax. However, in case of massive pleural effusion that may not be managed with thoracentesis, initial drainage was achieved with pigtail drainage. If clinically needed, especially when a patient re-suffered from dyspnea after pigtail drainage remov- al, additional thoracentesis was performed. Pleurodesis was not performed in pigtail drainage group.
LT group included patients who underwent LT due to ad- vanced liver cirrhosis combined with HH. Surgery group in- cluded patients who underwent surgery for the management of HH. All patients in surgery group underwent video-assisted thoracoscopic surgery (VATS) for the detection and closure of diaphragmatic defects (Supplementary Fig. 1, only online) with concomitant pleurodesis. Pleurodesis was performed with Abnoba Viscum F (ABNOBA GmbH, Pforzheim, Germa- ny) in eight patients, and Steritalc® (Novatech SA, La Ciotat, France) powder in two patients. A 24-Fr chest tube was main- tained for 7–8 days and removed after confirmation of stable chest tube drainage volume. Diaphragmatic defect closure was performed using sutures and additional fibrin glue. Post- operative positive expiratory end pressure (5–10 cmH2O) in an intubated state was maintained for 1 day, and peritoneal drainage for 5 days. Surgery for HH was considered successful if the patient had no recurrence of ipsilateral pleural effusion, or if they did not exhibit symptoms requiring drainage in case of recurrence. Surgery for HH was considered to have failed if there was recurrence of pleural effusion requiring drainage.
After discharge, plain chest radiographs were obtained every 2 or 3 months in outpatient clinics to check for recurrence.
Patients with refractory HH were recommended to undergo LT. Consultations at specific departments were arranged for detailed counselling.
Definition and management of refractory HH
HH was diagnosed using the following international criteria:
1) serum-to-pleural fluid albumin gradient >1.1; 2) pleural flu- id total protein <2.5 g/dL or pleural fluid/serum total protein ratio <0.5; 3) pleural fluid/serum LDH ratio <0.6; and 4) poly- morphonuclear cell count <250 cells/mm3.7 Refractory HH was defined as pleural effusion that 1) failed to respond to re-
striction of salt intake, the maximum dose of diuretic treat- ment (spironolactone at 400 mg/day and furosemide at 160 mg/day), and serial thoracentesis of more than two times; or 2) reappeared rapidly after therapeutic thoracentesis.
The number of needle punctures for drainage per person- years and the amount of drainage per day were analyzed. The occurrence rates of acute kidney injury (AKI) and hepatorenal syndrome (HRS) were recorded. AKI was defined as an in- crease in serum creatinine level of ≥0.3 mg/dL within 48 h, or an increase in serum creatinine to ≥1.5 times the baseline lev- el. HRS was defined as occurrence of AKI in patients despite diuretic cessation and albumin infusion, and chronic or acute hepatic disease with advanced hepatic failure and without any other apparent cause for AKI.
Ascites grading
Grading of ascites amount was based on the quantitative cri- teria proposed by the International Ascites club.8 Grade 1 as- cites is mild and can be detected only by imaging examina- tion, such as ultrasonography. Grade 2 ascites is moderate and evidenced by moderate symmetrical distension of the ab- domen, and is therefore readily detectable on physical exami- nation. Grade 3 ascites is large with marked distension of the abdomen.
Statistical analysis
Data are expressed as mean±standard deviation, or median with range. Chi-squared test or Student’s t-test was used for univariate analyses, and logistic regression was used for mul- tivariate analyses. Analysis of variance was used for multifac- torial comparisons. Cumulative overall survival was calculated using Kaplan-Meier method and compared between groups using log-rank test. Variables with p<0.05 in univariate analy- sis were entered into multivariate Cox regression analysis. In all analyses, p<0.05 was considered statistically significant. All statistical analyses were conducted using Statistical Package for the Social Sciences for Windows version 20.0 (IBM Corp., Armonk, NY, USA).
RESULTS
Baseline clinical characteristics of enrolled patients
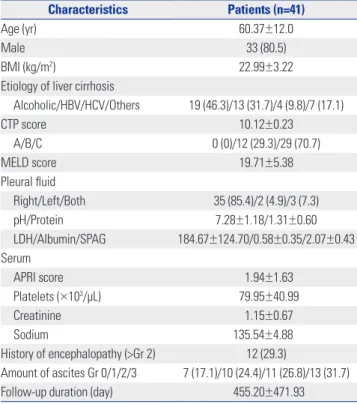
We identified 52 patients who were diagnosed with HH dur- ing the study period. With sodium restriction and use of di- uretics, HH was controlled in 11 patients, whereas 41 patients had refractory HH and underwent four treatment modalities for management of HH (Fig. 1). Baseline characteristics of en- rolled patients are shown in Table 1. Male sex was predominant (80.5%), and the mean age was 60.4 years. Alcohol consumption was the most common cause of liver cirrhosis (46.3%), fol- lowed by hepatitis B virus infection (31.7%). The mean Child- Turcotte-Pugh (CTP) score was 10.1, and CTP C class was themost common (70.7%). The mean Model for End Stage Liver Disease (MELD) score was 19.7. In total, 29.3% of patients had a previous history of hepatic encephalopathy (grade >2).
Table 1. Baseline Characteristics of Enrolled Patients
Characteristics Patients (n=41)
Age (yr) 60.37±12.0
Male 33 (80.5)
BMI (kg/m2) 22.99±3.22
Etiology of liver cirrhosis
Alcoholic/HBV/HCV/Others 19 (46.3)/13 (31.7)/4 (9.8)/7 (17.1)
CTP score 10.12±0.23
A/B/C 0 (0)/12 (29.3)/29 (70.7)
MELD score 19.71±5.38
Pleural fluid
Right/Left/Both 35 (85.4)/2 (4.9)/3 (7.3)
pH/Protein 7.28±1.18/1.31±0.60
LDH/Albumin/SPAG 184.67±124.70/0.58±0.35/2.07±0.43 Serum
APRI score 1.94±1.63
Platelets (×103/μL) 79.95±40.99
Creatinine 1.15±0.67
Sodium 135.54±4.88��
History of encephalopathy (>Gr 2) 12 (29.3)
Amount of ascites Gr 0/1/2/3 7 (17.1)/10 (24.4)/11 (26.8)/13 (31.7)
Follow-up duration (day) 455.20±471.93
BMI, body mass index; HBV, hepatitis B virus; HCV, hepatitis C virus; CTP, Child- Turcotte-Pugh; MELD, model for end-stage liver disease; LDH, lactate dehydro- genase; SPAG, serum-pleural fluid albumin gradient, APRI, aspartate amino- transferase to platelet ratio index; Gr, grade.
Values are presented as mean±standard deviation or n (%) unless otherwise indicated.
Hepatic hydrothorax diagnosed by thoracentesis (n=52)
Sodium restriction and diuretics
Controlled (n=11)
Uncontrolled (n=41)
Serial thoracentesis (n=11)
Pigtail drainage (n=16)
Surgery (n=10)
LT (n=4)
Fig. 1. Flowchart of patient enrollment and treatment. LT, liver transplanta- tion.
age as well as the total drainage amount per follow-up dura- tion. The volumes of drained pleural and peritoneal fluid were summed. The number of needle punctures (23.5 vs. 9.3) and drainage amount (288.0 mL/day vs. 125.5 mL/day) were high- er in pigtail group than in surgery group. Surgery group was associated with much less frequent needle punctures for tho-
Clinical characteristics and outcomes of patients
based on treatment modalities
Patients were categorized based on the treatment modalities they received for the management of HH: diuretics with serial thoracentesis, pigtail drainage, surgery, and LT. Moreover, 11 (26.8%) patients received diuretics with serial thoracentesis, 16 (39.0%) patients underwent pigtail drainage, 10 (24.4%) patients underwent surgery, and four (9.8%) patients under- went LT. Disease etiology did not differ among groups (Table 1). The median value of interval in serial thoracentesis group was 19 (range, 5–244) days. Although no statistically signifi- cant difference was found (p=0.06), the lowest CTP score was observed in serial thoracentesis group, and the highest score was observed in pigtail drainage group. MELD score was the highest in LT group and the lowest in serial thoracentesis group (22.0 vs. 17.0, p=0.017). Although surgery group showed slight- ly lower MELD scores than pigtail drainage group (18.0 vs.
21.5), no statistically significant difference was found (p=0.091).
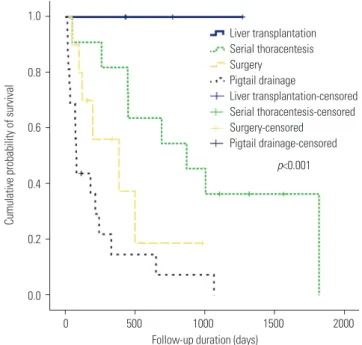
Mortality significantly differed among groups (Table 2). Fig. 2 shows the comparison of survival rates among treatment mo- dalities according to Kaplan-Meier analysis.
Clinical outcomes in pigtail drainage and surgery groups in refractory HH patients
Table 3 shows the comparison of clinical outcomes and adverse events between pigtail drainage group and surgery group in patients with refractory HH. Given the small number of pa- tients included in both groups, there were only few statistically significant differences in the comparisons. We calculated the number of needle punctures per year for pleural fluid drain-
1.0
0.8
0.6
0.4
0.2
0.0
0 500 1000 1500 2000 p<0.001
Follow-up duration (days)
Cumulative probability of survival
Liver transplantation Serial thoracentesis Surgery
Pigtail drainage
Liver transplantation-censored Serial thoracentesis-censored Surgery-censored
Pigtail drainage-censored Table 2. Clinical Characteristics and Outcomes of Patients Based on Treatment Modalities
Serial thoracentesis
(n=11) Pigtail drainage
(n=16) Surgery
(n=10) Liver transplantation
(n=4) p value
Cause of cirrhosis 0.618
Alcohol 4 (36.4) 10 (62.5) 4 (40.0) 1 (25.0)
HBV 4 (36.4) 3 (18.8) 3 (30.0) 3 (75.0)
HCV 2 (18.2) 0 (0.0)�� 0 (0.0)�� 0 (0.0)��
Idiopathic 1 (9.0)�� 3 (18.8) 3 (30.0) 0 (0.0)��
HCC 4 (36.4) 3 (18.8) 2 (20.0) 0 (0.0)�� 0.729
Diuretics dose
Furosemide (mg/day) 72.0 55.0 57.8 90.0 0.373
Spironolactone (mg/day) 175.0 146.2 125.0 133.3 0.917
Albumin (g/dL) 2.94 2.60 2.49 2.55 0.462
Total bilirubin (mg/dL) 2.39 4.04 3.15 7.38 0.024
PT (INR) 1.45 1.77 1.64 2.01 0.013
CTP (median, range) 9.0 (8–12) 11.0 (8–13) 10.5 (9–12) 10.5 (10–13) 0.063
MELD (median, range) 17.0 (10–22) 21.5 (14–32) 18.0 (11–28) 22.0 (17–29) 0.017
Survival duration (median, range) 868.0 (49–1817) 79.0 (15–1064) 179.0 (48–980) 601.5 (428–1270) <0.001
12 months mortality (%) 18.2 87.5 70.0 0.0 <0.001
HBV, hepatitis B virus; HCV, hepatitis C virus; HCC, hepatocellular carcinoma; PT, prothrombin time; INR, international normalized ratio; CTP, Child-Turcotte-Pugh;
MELD, model for end-stage liver disease.
Values are presented as median (range) or n (%) unless otherwise indicated.
Fig. 2. Comparison of survival rates among treatment modalities by Ka- plan-Meier analysis (serial thoracentesis vs. surgery, p=0.114; surgery vs. pigtail drainage, p=0.108; serial thoracentesis vs. pigtail drainage, p=
0.001).
racentesis compared to pigtail drainage group (0.9 vs. 18.8), but associated with a slightly higher number of needle punc- tures for paracentesis (8.4 vs. 4.8). As shown in Table 3, the cause of death did not differ significantly between the two groups, and various adverse events occurred in both groups, but not life-threatening events. However, in surgery group, some interventions, such as prolonged hospital stay, were needed due to the additional use of antibiotics and surgery (e.g., herniorrhaphy). We assessed the cut-off values of CPT score which may indicate poorer prognosis in surgery group, and patients with a CTP score >10 points had poorer death-re- lated outcomes (p=0.038).
Among 10 patients who underwent surgery, no periopera- tive mortality occurred; and all patients were discharged from the hospital after 22.5 days (median, range 7–50). Although diaphragmatic defects were found by VATS in nine patients, the defect could not be located in one patient, and only pleurodesis was performed. Including this patient, two (20.0%) patients experienced HH recurrence. Eight (80.0%) patients had an in- creased volume of ascites; and among these patients, five were administered increased dose of diuretics. Of these five patients, two patients experienced HRS, which eventually led to death. However, there was no difference in mortality rates between the two groups.
Analysis of factors related to survival
We assessed multiple factors related to survival. In univariate analysis, body mass index (BMI) <19 kg/m2, refractory HH man- aged with pigtail drainage, CTP score >10, history of severe he- patic encephalopathy (grade >2), ascites >grade 1, and MELD score ≥16 were related to poor outcomes (Table 4). In multi- variate analysis, BMI <19 kg/m2, refractory HH managed with pigtail drainage, and CTP score >10 were related to poor sur- vival rates with statistical significance.
DISCUSSION
This study demonstrated the characteristics and clinical out- comes of patients treated with four different modalities for the management of HH. Some previous studies have reported on the results of various modalities for HH treatment;9-11 howev- er, these studies were limited to a few methods. To the best of our knowledge, this is the first study to elucidate and compare the safety and efficacy of surgery and pigtail drainage, repre- senting refractory HH patients with decompensated cirrhosis encountered in clinical practice.
Regarding risk factors for HH, alcohol consumption was the most common cause of HH in the present study. Chronic al- Table 3. Comparison of Clinical Outcomes between Pigtail Drainage and Surgery Groups
Surgery (n=10) Pigtail (n=16) p value
Number of needle punctures for drainage/year 9.3 23.5 0.161
Thoracentesis 0.9 18.8 0.016
Paracentesis 8.4 4.8 0.381
Drainage amount (mL/day) 125.5 288.0 0.320
Occurrence of AKI 5 (50.0) 11 (68.8) 0.548
Occurrence of HRS 3 (30.0) 8 (50.0) 0.432
Cumulative overall survival (day) 402.1 221.7 0.113
Cut-off value of CTP >10 - 0.038
Cause of death 6 14
Hepatic failure 2 (33.3) 6 (42.9)
HRS 2 (33.3) 4 (28.6)
Varix bleeding 1 (16.7) 1 (7.1)
HCC progression 1 (16.7) 2 (14.3)
Sepsis - 1 (7.1)
Adverse events Chest tube site oozing 1 Pigtail site oozing 7
Delayed port site bleeding 1 Pigtail site infection 1 Incisional hernia 1 Pigtail site pain* 4
Pneumonia 1 Urinary tract infection 1
CRBI 1 Perioperative mortality 0
Recurrence of HH 2
AKI, acute kidney injury; HRS, hepatorenal syndrome; CTP, Child-Turcotte-Pugh; HRS, hepatorenal syndrome; HCC, hepatocellular carcinoma; CRBI, central cathe- ter-related bacterial infection; HH, hepatic hydrothorax.
Values are presented as n (%) unless otherwise indicated.
*Defined as pain that required intervention.
cohol consumption and poor calorie intake causes muscle at- rophy, resulting in low BMI and cachexia. These factors may increase the risk of anatomic thinning and the separation of col- lagenous fibers in the tendinous portion of the diaphragm.12
Regarding treatment modality other than LT, many man- agement options are available, such as serial thoracentesis, pigtail drainage, chest tube insertion, TIPS, and surgery. How- ever, most patients have severely decompensated liver cirrho- sis with poor liver function. Therefore, many difficulties are as- sociated with making treatment decisions in clinical practice.
In terms of clinical outcomes based on treatment modali- ties, LT had the most favorable outcomes. Although the total number of patients who underwent LT was small, all four pa- tients survived, with median survival duration of 601.5 days.
Consistent with other studies,9,11 patients who underwent se- rial thoracentesis showed better survival than those who un- derwent pigtail drainage or surgery in our study. Unlike other studies that did not consider the liver function of patients in each group,9,11 serial thoracentesis group had better liver func- tion than the other two groups (pigtail drainage and surgery) in the current study. This better liver function, rather than treat- ment modality, might have led to the higher survival rate. There- fore, considering the impracticality of LT in clinical practice, serial thoracentesis on demand can be an option for patients with relatively preserved liver function. However, serial thora- centesis was not effective in some patients with more advanced cirrhosis; and in these cases, pigtail drainage or surgery was performed in the present study.
Traditionally, surgery for HH is considered to have high risks for morbidity and mortality due to portal hypertension and poor liver function.13 Although there have been several stud- ies concerning the surgical management of HH, these studies are limited and clinical outcomes were not positive.14-18 How- ever, the results of the present study showed a success rate of 80.0% without recurrence and surgery-related mortality. Fur- thermore, compared to pigtail drainage, needle puncture was required less frequently, and the total drainage amount of pleu- ral and peritoneal fluid was smaller (9.3 times vs. 23.5 times,
125.5 mL/day vs. 288 mL/day, respectively). However, para- centesis was required more frequently in surgery group as per the main mechanism of HH (the passage of ascites via dia- phragmatic defects), and the distribution of ascitic fluid be- tween peritoneal and thoracic cavities became confined to peritoneal cavity only, increasing the occurrence rate of asci- tes.5,14,19-23 For these reasons, the obliteration of diaphragmatic defects can eventually increase the amount of ascitic fluid.
However, despite evaluating the dose of diuretics, AKI and HRS occurred more frequently in pigtail drainage group than in surgery group, although statistically not significant (p=0.548, p=0.432, respectively). Kaplan-Meier analysis revealed that the cumulative overall survival was longer in surgery group than in pigtail drainage group (402.1 days vs. 221.7 days, p=
0.113). However, this superior result of surgery group may be due to selection bias that patients in surgery group may have had more preserved liver function and better performance score than those in pigtail drainage group. Although it was not statistically significant, both CPT score and MELD score was lower in surgery group.
Furthermore, we compared survival rates between patients with CTP scores >10 and those with CTP scores ≤10. CTP >10 group had poorer survival rate than CTP ≤10 group. This sug- gests that in patients who are ineligible for LT, considering its ability to provide better quality of life and non-inferior surviv- al duration compared to pigtail drainage, surgery can be an option in patients with refractory HH and CTP ≤10. No signifi- cant difference in the causes of death was found between the two groups. Although no life-threatening events occurred, various adverse events, such as chest tube site oozing, bleeding, hernia due to increased peritoneal pressure, infections, and pain, occurred in both groups.
TIPS is recommended in several studies and guidelines for managing HH, and the following criteria for TIPS have been suggested: age <65 years, MELD <18, CTP class A or B, cardiac ejection fraction >60%, no history of severe encephalopathy, no response to diuretic treatment, and/or repetitive therapeu- tic thoracentesis.13,20,21,24-26 However, these criteria in refractory Table 4. Univariate and Multivariate Analyses on Survival Rates
Factors Univariate analysis Multivariate analysis
HR (95% CI) p value HR (95% CI) p value
BMI <19 (kg/m2) 6.6 (1.81–24.92)� 0.001 15.5 (3.23–74.58) 0.001
Serial thoracentesis 0.41 (0.17–0.99)� 0.053
Pigtail drainage 4.24 (1.97–9.14)� <0.001 4.52 (2.02–10.15) <0.001
Surgery 1.24 (0.50–3.08)� 0.639
LT 0.03 (0.00–1.93) 0.103
CTP score >10 3.6 (1.81–7.32) <0.001 2.9 (1.22–7.14) 0.021
History of severe encephalopathy 2.7 (1.33–5.44) 0.004
Ascites >Gr 1 2.2 (1.01–4.62) 0.038
MELD ≥16 2.6 (1.12–5.93) 0.033
HR, hazard ratio; CI, confidence interval; BMI, body mass index; LT, liver transplantation; CTP, Child-Turcotte-Pugh; Gr, grade; MELD, model for end stage liver dis- ease.
HH patients have a narrow spectrum due to poor liver func- tion, and their application in practice is challenging. The pa- tients enrolled in this study had a median MELD score of 19, and 70.7% of patients had CTP class C. Furthermore, 29.3% of patients had a history of severe hepatic encephalopathy (>grade 2). For these reasons, TIPS was not considered a treat- ment modality in most cases of refractory HH in the present study.
In multivariate analysis for survival, BMI <19 kg/m2, HH managed with pigtail drainage, and CTP score >10 were asso- ciated with poor survival rate. Patients with liver cirrhosis ex- hibit progressive loss of fat and muscle mass. Severe loss of muscle and body mass are known to be related to poor prog- noses.27 In this study, cachexia with low BMI (<19 kg/m2) was the strongest factor associated with survival rate (hazard ratio 10.6, p=0.002). Therefore, encouraging cirrhosis patients with low BMI to gain body weight and providing them with nutri- tional intervention should be considered in clinical practice.
CTP score, which reflects the grade of ascites and encepha- lopathy, was related to survival rates, rather than MELD score.
This study had several limitations. First, this was a single- center retrospective study based on hospital records and loco- regional patient information. Second, the number of included patients was small, due to the short survival duration of de- compensated liver cirrhosis patients and low incidence rate of HH. Considering the small sample size and selection bias, which may have occurred when deciding the treatment mo- dality for various patient conditions, these factors may have influenced the clinical outcomes of treatment modalities and may be impetuous to draw a conclusion. Therefore, further studies investigating a large number of patients with hydro- thorax are required.
In conclusion, serial thoracentesis may be recommended for management of HH. In patients who have refractory HH not managed with serial thoracentesis, surgical management can be a useful option, alternative to pigtail drainage despite several concerns. Further studies investigating a large number of patients with hydrothorax are required.
ACKNOWLEDGEMENTS
This study was supported by grants (CRI 18091-1) from Chon- nam National University Hospital Biomedical Research Insti- tute.
AUTHOR CONTRIBUTIONS
Conceptualization: Sung Kyu Choi and Yochun Jung. Data curation:
Jae Hyun Yoon and Hee Joon Kim. Formal analysis: Jae Hyun Yoon.
Funding acquisition: Jae Hyun Yoon and Chung Hwan Jun. Investiga- tion: Jae Hyun Yoon and Chung Hwan Jun. Methodology: Jae Hyun Yoon. Project administration: Chung Hwan Jun and Sung Kyu Choi.
Resources: Chung Hwan Jun and Yochun Jung. Software: Hee Joon Kim and Sung Bum Cho. Supervision: Sung Kyu Choi and Yochun
Jung. Validation: Yochun Jung and Sung Bum Cho. Visualization:
Sung Bum Cho. Writing—original draft: Jae Hyun Yoon and Hee Joon Kim. Writing—review & editing: Jae Hyun Yoon and Chung Hwan Jun.
ORCID iDs
Jae Hyun Yoon https://orcid.org/0000-0002-4993-2496 Hee Joon Kim https://orcid.org/0000-0002-8636-5726 Chung Hwan Jun https://orcid.org/0000-0002-7136-8350 Sung Bum Cho https://orcid.org/0000-0001-9816-3446 Yochun Jung https://orcid.org/0000-0001-7165-3007 Sung Kyu Choi https://orcid.org/0000-0002-6878-3385
REFERENCES
1. Malagari K, Nikita A, Alexopoulou E, Brountzos E, Papathanasiou M, Mitromaras J, et al. Cirrhosis-related intrathoracic disease. Im- aging features in 1038 patients. Hepatogastroenterology 2005;52:
558-62.
2. Foschi FG, Piscaglia F, Pompili M, Corbelli C, Marano G, Righini R, et al. Real-time contrast-enhanced ultrasound--a new simple tool for detection of peritoneal-pleural communications in hepatic hy- drothorax. Ultraschall Med 2008;29:538-42.
3. Rubinstein D, McInnes IE, Dudley FJ. Hepatic hydrothorax in the absence of clinical ascites: diagnosis and management. Gastro- enterology 1985;88(1 Pt 1):188-91.
4. Xiol X, Tremosa G, Castellote J, Gornals J, Lama C, Lopez C, et al.
Liver transplantation in patients with hepatic hydrothorax. Transpl Int 2005;18:672-5.
5. Lazaridis KN, Frank JW, Krowka MJ, Kamath PS. Hepatic hydrotho- rax: pathogenesis, diagnosis, and management. Am J Med 1999;
107:262-7.
6. The Korean Association for the Study of the Liver (KASL). KASL clinical practice guidelines for liver cirrhosis: ascites and related complications. Clin Mol Hepatol 2018;24:230-77.
7. Machicao VI, Balakrishnan M, Fallon MB. Pulmonary complica- tions in chronic liver disease. Hepatology 2014;59:1627-37.
8. Moore KP, Wong F, Gines P, Bernardi M, Ochs A, Salerno F, et al.
The management of ascites in cirrhosis: report on the consensus conference of the International Ascites Club. Hepatology 2003;38:
258-66.
9. Hsu SL, Tseng CW. Comparison of treatment of hepatic hydrotho- rax with catheter drainage versus serial thoracentesis. Curr Opin Pulm Med 2018;24:392-7.
10. Badillo R, Rockey DC. Hepatic hydrothorax: clinical features, man- agement, and outcomes in 77 patients and review of the literature.
Medicine (Baltimore) 2014;93:135-42.
11. Hung TH, Tseng CW, Tsai CC, Hsieh YH, Tseng KC, Tsai CC. Mor- tality following catheter drainage versus thoracentesis in cirrhotic patients with pleural effusion. Dig Dis Sci 2017;62:1080-5.
12. Peters TJ, Martin F, Ward K. Chronic alcoholic skeletal myopathy- -common and reversible. Alcohol 1985;2:485-9.
13. Porcel JM. Management of refractory hepatic hydrothorax. Curr Opin Pulm Med 2014;20:352-7.
14. Mouroux J, Perrin C, Venissac N, Blaive B, Richelme H. Manage- ment of pleural effusion of cirrhotic origin. Chest 1996;109:1093-6.
15. Milanez de Campos JR, Andrade Filho LO, de Campos Werebe E, Pandulo FL, Filomeno LT, Jatene FB. Hepatic hydrothorax. Semin Respir Crit Care Med 2001;22:665-74.
16. Milanez de Campos JR, Filho LO, de Campos Werebe E, Sette H Jr, Fernandez A, Filomeno LT, et al. Thoracoscopy and talc poudrage in the management of hepatic hydrothorax. Chest 2000;118:13-7.
17. Nakamura Y, Iwazaki M, Yasui N, Seki H, Matsumoto H, Masuda R, et al. Diaphragmatic repair of hepatic hydrothorax with VATS after abdominal insufflation with CO(2). Asian J Endosc Surg 2012;
5:141-4.
18. Luh SP, Chen CY. Video-assisted thoracoscopic surgery (VATS) for the treatment of hepatic hydrothorax: report of twelve cases. J Zhejiang Univ Sci B 2009;10:547-51.
19. Strauss RM, Boyer TD. Hepatic hydrothorax. Semin Liver Dis 1997;
17:227-32.
20. Alberts WM, Salem AJ, Solomon DA, Boyce G. Hepatic hydrotho- rax. Cause and management. Arch Intern Med 1991;151:2383-8.
21. Cardenas A, Kelleher T, Chopra S. Review article: hepatic hydro- thorax. Aliment Pharmacol Ther 2004;20:271-9.
22. Emerson PA, Davies JH. Hydrothorax complicating ascites. Lan-
cet 1955;268:487-8.
23. Bhattacharya A, Mittal BR, Biswas T, Dhiman RK, Singh B, Jindal SK, et al. Radioisotope scintigraphy in the diagnosis of hepatic hy- drothorax. J Gastroenterol Hepatol 2001;16:317-21.
24. Alonso JC. Pleural effusion in liver disease. Semin Respir Crit Care Med 2010;31:698-705.
25. Degawa M, Hamasaki K, Yano K, Nakao K, Kato Y, Sakamoto I, et al. Refractory hepatic hydrothorax treated with transjugular intra- hepatic portosystemic shunt. J Gastroenterol 1999;34:128-31.
26. Al-Zoubi RK, Abu Ghanimeh M, Gohar A, Salzman GA, Yousef O.
Hepatic hydrothorax: clinical review and update on consensus guidelines. Hosp Pract (1995) 2016;44:213-23.
27. Plauth M, Schütz ET. Cachexia in liver cirrhosis. Int J Cardiol 2002;
85:83-7.