Uterine fibroids are the most common solid tumors of the female genital tract, and they develop in 20-40% of women of childbearing age (1). Although not all the
women with fibroids exhibit symptoms, approximately 10-20% of women with fibroids have symptoms that negatively affect their quality of life (2). Menorrhagia, which often leads to iron-deficiency anemia, and pain during menstruation are the most common complica- tions of uterine leiomyoma. The therapeutic options for the treatment of fibroids include hysterectomy, my- omectomy, gonadotropin-releasing hormone agonists and a number of experimental ablative techniques in- volving energy sources such as focused ultrasound or ra- diofrequency ablation. Uterine artery embolization
Uterine Artery Embolization for the Treatment of Symptomatic Fibroids
1Kyung Ah Kim, M.D., Man Deuk Kim, M.D., Hee Jin Kim, M.D., Mee Hwa Lee, M.D.2 Jin Ho Cho, M.D.2, Sun Hee Cha, M.D.2, Sang-Wook Yoon, M.D., Eun Hee Ahn, M.D.2
Purpose: The aim of this study was to determine the potential usefulness of uterine artery embolization (UAE) for the management of uterine leiomyoma.
Materials and Methods: Sixty nine patients (mean age; 40.3 years, age range; 31-52 years) who underwent UAE for symptomatic fibroids (with menorrhagia, dysmenor- rhea and bulk-related symptoms) from January 2000 to December 2000 were retro- spectively analyzed. The mean follow-up period was 3.5 months (range: 1-8 months).
The fibroids ranged in size from 2.0 cm to 13.2 cm with a mean size of 5.8 cm. We per- formed embolization using polyvinyl alcohol particles (250-710μm). The improve- ment of the clinical symptoms was analyzed. Reduction of the uterine and predomi- nant fibroid volumes was assessed using MRI.
Results:Symptom improvement for the menorrhagia (87.5%), dysmenorrhea (83.3%) and the bulk-related symptoms (79.2%) was reported. Complications included ovarian failure in four patients (5.8% of the total patients, mean age: 43.3 yrs) and infection in three patients (4.3% of the total patients) who underwent conservative management with intravenous antibiotics and analgesics. The volume reduction rate of the uterus and the predominant fibroids after uterine artery embolization were 36.3% and 56.6%, respectively.
Conclusion:UAE is a promising new treatment for symptomatic fibroids and may be a valuable alternative to hysterectomy.
Index words : Arteries, uterine
Arteries, therapeutic embolization Uterus neoplasms, therapy
1Department of Diagnostic Radiology, Bundang CHA General Hospital, Pochon CHA University
2Department of Obstetrics & Gynecology, Bundang CHA General Hospital, Pochon CHA University
Received November 25, 2004 ; Accepted May 3, 2005
Address reprint requests to : Man Deuk Kim, M.D., Department of Diagnostic Radiology, Bundang CHA General Hospital, Pochon CHA University, 351 Yatap-dong, Bundang-gu, Sungnam-si, Kyonggi-do 463- 712, Republic of Korea.
Tel. 82-31-780-5382 Fax. 82-31-780-5381 E-mail: mdkim@cha.ac.kr
(UAE) has emerged as a viable treatment option for pa- tients with symptomatic fibroids, and this technique is successful for controlling symptoms in 85-95% of pa- tients (3-5). The purpose of our study was to evaluate the effectiveness and safety of UAE for its use in the management of uterine leiomyoma.
Materials and Methods
The institutional review board of our hospital gave ap- proval for the entire study, and each patient gave us a written informed consent. A retrospective analysis was performed with using the records of 69 patients who un- derwent UAE for leiomyoma from January 2000 to December 2000 at our institution. The mean age of the women was 42.0 years (range: 27-55 years). The mean follow-up duration was 102 days (range: 42-175 days).
The symptoms related to leiomyomas were classified in- to three categories: abnormal bleeding (menorrhagia), pelvic pain (dysmenorrhea) and bulk-related symptoms (frequency of urination or pelvic heaviness). The women were asked to evaluate the changes of their symptoms after the procedure and also their satisfaction with the procedure and its outcomes. We classified the symptomatic outcomes of menorrhagia and dysmenor- rhea as markedly improved, slightly or moderately im- proved, no change, or worsened as compared with the patient’s condition before the procedure. The patients’
satisfaction with the procedures and outcomes were classified as satisfied and dissatisfied. Embolization was performed through the right femoral artery approach in all patients with use of the Seldinger technique.
Nonselective pelvic arteriography was done; if the en- tire course of uterine artery could not be evaluated, then additional internal iliac arteriography was performed.
Following this procedure, both the uterine arteries were catheterized. Co-axial 3 French catheters (TrackerⓇ-18 Infusion Catheter, Boston Scientific, Fremont, U.S.A.) were used to get as distal as possible into the uterine ar- teries. Polyvinyl alcohol (PVA) particles (ContourⓇ, Boston Scientific, Fremont, U.S.A.) mixed with 40 mL of 1:1 saline-contrast mixture was employed as the em- bolizing material. The size of the PVA particles we used was 250-710μm. Embolization was performed until there was a complete cessation of the blood flow in the ascending uterine artery with a residual flow in the low- er uterine segment. The preprocedural and postproce- dural follow-up (mean: 3.5 months, range: 1-8 months) contrast enhanced MRI (1.5 T Supermagnet, Magnetom
Vision, Siemens, Erlangen, Germany) of the pelvis were performed for all patients. All the patients underwent axial, sagittal fast spin echo T2 weighted imaging and contrast enhanced T1 weighted sagittal images. The fol- lowing imaging parameters were used for the T2 weighted imaging: (TR/TE, 3500/99; matrix 256×132;
section thickness: 6 mm; intersection gap: 1.8 mm;
number of excitations: 3). Enhanced MR imaging was performed 2 minute after the intravenous infusion of 10 mL of gadolinium (Dotarem(r), Guerbet, Aulnay-sous- Bois, France) and the FLASH (Fast low-Angle Shot) se- quences were also taken (TR/TE, 117.3/4.1; flip angle:
80°; matrix: 140×256; section thickness: 5 mm).
We calculated the uterine and fibroid volumes by us- ing the formula for a prolate ellipse: length×width×
depth×0.5233. The ellipsoid formula was convenient to use for assessing fibroleiomyomas’ size, and this tech- nique has been shown to be reliable for the measure- ment of uterine volume, as compared with more sophis- ticated region-of-interest methods (6, 7).
Results
The clinical symptoms and outcomes after UAE are summarized in Table 1. The maximum diameter of the dominant fibroids ranged from 2.0 cm to 13.2 cm, and the mean diameter was 5.8 cm. The most common pre- senting symptom was menorrhagia, and this was noted in 81.1% of the patients. Menstrual pain was observed in 60.9% of the patients. Bulk-related symptoms such as pelvic heaviness and urinary frequency were encoun- tered in 76.8% of the patients. The menorrhagia and dysmenorrhea improved in 87.5% and 83.3% of the pa-
Table 1. Clinical Symptoms and Outcomes after Uterine Fibroid Embolization
Symptoms N (%)
Menorrhagia (n=56)
Improved 49 (87.5%)
Markedly 27
Slightly & Moderately 22
Unchanged 04
Worsened 03
Dysmenorrhea (n=42)
Improved 35 (83.3%)
Markedly 19
Slightly & Moderately 16
Unchanged 06
Worsened 01
Bulk-related symptoms (n=53)
Improved 42 (79.2%)
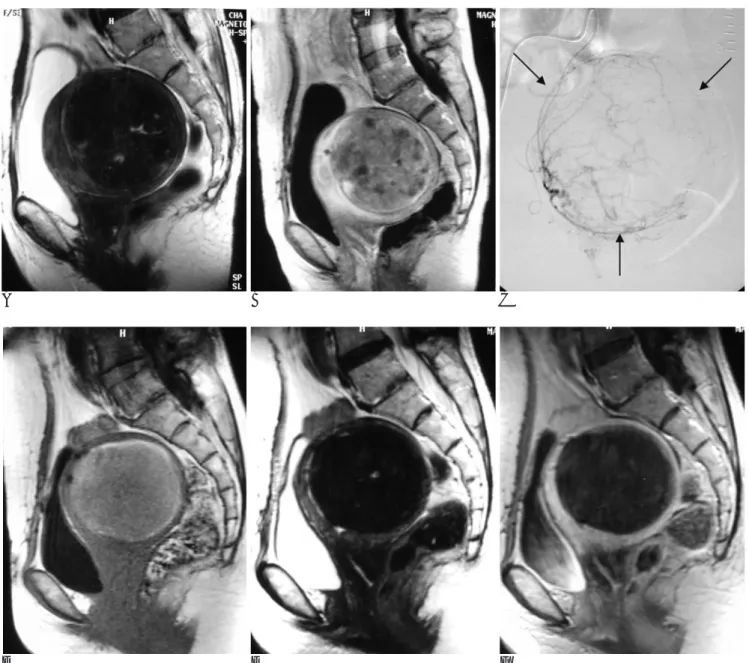
tients, respectively. 79.2% of the patients experienced improvement of the bulk related symptoms. MR imag- ing revealed that the mean volume reduction rates of the uterus and the dominant fibroid were 36.3% and 56.6%, respectively (Fig. 1), as is shown in Table 2.
The increased leiomyoma signal intensity that was seen on the T1-weighted MR images obtained after em- bolization was thought to result from the hemorrhagic necrosis and the presence of the blood breakdown prod- ucts (Fig. 2). Pelvic pain was observed in most women after UAE. This pain was managed with intravenously administered opiates and non-steroidal anti-inflammato-
ry drugs (NSAIDS) such as ketoprofen. No major com- plications requiring hysterectomy or laparotomy were observed in any of the patients. Four (6.2%) women were amenorrheic after embolization (age range: 40-46
A B
Fig. 1. A-44-year-old woman with a broad based submucosal leiomyoma.
The T2-weighted and gadolinium-en- hanced T1-weighted sagittal images re- veal a 7 cm sized leiomyoma and the enhancement is equivalent to that of the surrounding myometrium before embolization (A, B). After embolization, the leiomyoma is no longer enhancing and there is volume reduction of 50.7%
(C, D).
C D
Table 2. Reduction of the Uterine and Dominant Fibroid Volumes (Volume±standard deviation) after UFE
Pre-UFE Post-UFE Mean % change Uterus 373.9±182.3 215.6±96.8 36.3%
Predominant Fibroid 99.9±87.6 040.3±41.7 56.6%
Note: Volumes are in units of cm3 UFE: Uterine Fibroid Embolization
yrs, mean age: 43.3 yrs). Six of the women passed their fibroids spontaneously (Fig. 3). Two patients required hysteroscopic assistance to resect the whole fibroid since the residual myomas hung about the orifice of the uterine cervix. Three (4.6%) patients were readmitted because of abdominal pain, fever, leukocytosis, a foul odor from their vaginal discharge and a high suspicion of infection of the necrotic myomas; they were treated by intravenous antibiotics and analgesia. No other clini-
cal sequelae, either early or delayed, were documented as a result of infection. Two patients became pregnant;
one patient delivered their baby vaginally and the other patient delivered their baby by elective cesarean sec- tion. Ninety-two percent of the women were satisfied with the procedure and its outcome. Ninety-five percent of the women would also recommend this treatment to others.
A B C
D E F
Fig. 2. A-54-year-old woman with an intramural myoma.
The T2-weighted and gadolinium-enhanced T1-weighted sagittal images. Before embolization, an 8.3 cm sized intramural myoma is demonstrated with contrast enhancement (A, B). The angiogram obtained with using the right femoral artery approach shows the selective opacification of the right uterine artery. The fibroid vasculature of the uterus (arrows) is demonstrated (C). After em- bolization, the increased intensity of the leiomyoma on the T1-weighted MR image results from hemorrhagic necrosis and the pres- ence of blood breakdown products (D). The T2-weighted and gadolinium-enhanced T1-weighted sagittal images reveal that the leiomyoma is no longer enhancing (E, F).
Discussion
Uterine leiomyomas are benign, hypervascular tu- mors that originate in the intramural portion of the my- ometrium as an abnormal proliferation of smooth-mus- cle cells (8). Uterine leiomyomas are the most frequent tumors of the female genital tract; they occur in 20- 50% of women who are older than 40 years (9), and these tumors can cause abnormal bleeding, pelvic pain, heaviness and discomfort.
Of the over 600,000 hysterectomies performed annu- ally in the United States, approximately 30% are per- formed for the treatment of uterine fibroids (2).
20-25% of women who undergo myomectomy will ultimately require an additional surgical procedure (10- 12). Hormonal treatment usually fails to control the symptoms or the tumor growth after the treatment is stopped (13). UAE is gaining acceptance as an effective alternative to surgical treatment, and it successfully con- trols symptoms in 85-95% of patients (3-5). Overall, the mean uterine volume reduction and dominant fi- broid volume reduction following UAE were 23%-48%
and 43-68%, respectively (14-17).
Postembolization syndrome (pelvic pain, nausea, vom- iting) is a common side effect of UAE resulting from tis- sue ischemia, but most of these symptoms are well con- trolled with conservative treatment. Other complica- tions include ovarian failure, infection of the necrotic myomas, vaginal discharge and vaginal dryness that is related to non-targeted tissue embolization (14-17).
Uterine necrosis or infection leads to emergency hys- terectomy in 1-2% of the cases. Chronic vaginal dis- charge is one of the frequent complications of UAE, and this results from the persistent drainage of necrotic ma- terial into the uterus. The etiology of ovarian failure is not yet clearly understood and it is likely to be a multi- factorial process. The following hypotheses have been suggested. 1) The older ovary may have less functional reserve than the younger ovary and therefore, it may be more susceptible to the embolic insult of the material re- fluxed into the ovarian artery from the uterine artery. 2) Statistical coincidence. Because the natural rate of menopause is approximately 4% in 45-year-old women and 35% in 49-year-old women, some patients may lose their ovarian function even without fibroid emboliza- tion. 3) The studies of ovarian function after hysterecto- my with sparing the ovary have demonstrated a range of early ovarian failure of 16.7-57.5% (18). There may be a role that a viable uterus plays in the normal ovarian function. Although the aftereffects of UAE on fertility have not been established, successful pregnancies have been reported after UAE (19). In our series, two patients became pregnant with one case delivering their baby vaginally and the other delivering by elective cesarean section.
Although a few studies with positive outcomes after performing UAE for fibroids have been published in the Korean literature, their preprocedural diagnoses and the volume reductions of uterus and myoma following UAE were determined by transvaginal ultrasound (20-22).
To our knowledge, this report is the largest series to de-
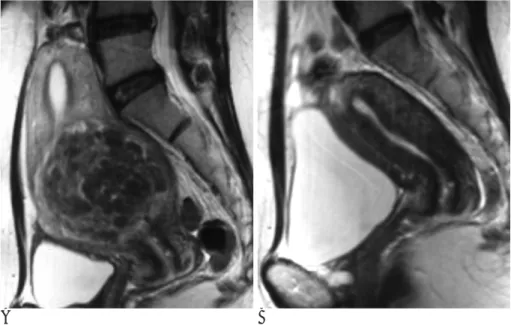
A B
Fig. 3. A-41-year-old woman with a submucosal myoma.
The T2-weighted sagittal image shows a broad-based submucosal myoma of about 7 cm (A). The follow-up MRI 3 months after embolization shows that the myoma has disappeared (B).
scribe UAE for symptomatic fibroids in Korea.
Furthermore, all the patients in our series underwent both preprocedural and follow-up MRI. Ultrasonogra- phy has been the traditional imaging modality used to assess women with symptomatic fibroids, but this modality has a limited ability to detect coexistent uter- ine or pelvic pathology, and it typically does not identify infarcted fibroids following UAE. MRI has a high accu- racy for distinguishing between fibroids and other uter- ine diseases such as adenomyosis, and it also has ability to characterize infarcted fibroids and to measure the uterine and fibroid volumes more accurately (23, 24).
In terms of embolic agents, PVA particles and calibrat- ed microspheres are currently widely used. PVA parti- cles tend to clump and form aggregates within the catheters and within the vessels. Calibrated micros- pheres are associated with a more controlled arterial oc- clusion and their use can lead to a more effective em- bolization. However, in a recent study of Spies et al, there were no significant differences between the out- comes of fibroid embolization with using PVA and the tris-acryl gelatin microsphere (25). Six of our patients ex- perienced vaginal expulsion. They presented with lower abdominal pain during expulsion, and vaginal discharge with small pieces of tissue occurred for several days to several months. After passing the myomas, all of their symptoms were resolved. The exact mechanism of transvaginal expulsion is not clear. The suggested hy- pothesis is that the shrinkage difference between the myoma and the myometrium following UAE forces the fibroids to be expelled.
The high rates of the women’s satisfaction (92%) and recommendation (95%) to others in our study were di- rectly related to the improvements in their symptoms and to the reduced impact of their disease on their lives.
We concluded that UAE is a promising new treatment and it is safe and effective for treating and controlling symptomatic fibroids.
References
1. Buttram VC, Reiter RC. Uterine leiomyomata: etiology, sympto- matology and management. Fertil Steril 1981;36:433-445
2. Lepine LA, Hillis SD, Marchbanks PA, Roonin LM, Morrow B, Kieke BA, et al. Hysterectomy surveillance-United States, 1980- 1993. MMW Morb Mort Wkly Rep CDC Surveill Summ 1997;46:1- 15
3. Ravina JH, Herbreteau D, Ciraru-Vigneron N, Bouret JM, Houdart E, Aymard A, et al. Arterial embolisation to treat uterine myomata.
Lancet 1995;346:671-672
4. Spies JB, Ascher SA, Roth AR, Kim J, Levy EB, Gomez-Jorge J.
Uterine artery embolization for leiomyomata. Obstet Gynecol 2001;
98:29-34
5. Walker WJ, Pelage JP. Uterine artery embolisation for sympto- matic fibroids: clinical results in 400 women with imaging follow up. Br J Obstet Gynaecol 2002;109:1262-1272
6. Broekmans FJ, Heitbrink MA, Hompes PGA, Schoute E, Falke T, Schoemaker J. Quantitative MRI of uterine leiomyomas during triptorelin treatment: reproducibility of volume assessment and predictability of treatment response. Magn Reson Imaging 1996;14:
1127-1135
7. Orsini LF, Salardi S, Pilu G, Bovicelli L, Cacciari E. Pelvic organs in premenarcheal girls: real-time ultrasonography. Radiology 1984;
153:113-116
8. Sasadeusz KJ, Andrews RT. Uterine fibroid embolization. Semin Roentgenol 2002;37:361-370
9. Verkauf BS. Myomectomy for infertility enhancement and preser- vation. Fertil Steril 1992;58:1-15
10. Reidy JF, Bradley EA. Uterine artery embolization for fibroid dis- ease. Cardiovasc Intervent Radiol 1998;21:357-360
11. Sutton CJ. Treatment of large uterine fibroids. Br J Obstet Gynaecol 1996;103:494-496
12. Hutchins FZ. Abdominal myomectomy as a treatment for sympto- matic uterine fibroids. Obstet Gynecol Clin North Am 1995;22:781- 789
13. Worthington-Kirsch RL, Popky GL, Hutchins FL Jr. Uterine arteri- al embolization for the management of leiomyomas: quality-of-life assessment and clinical response. Radiology 1998;208:625-629 14. Hutchins SL Jr, Worthington-Kirsch RL, Berkowitz RP. Selective
uterine artery embolization as primary treatment for symptomatic leiomyomata uteri. J Am Assoc Gynecol Laparosc 1999;6:279-284 15. Goodwin SC, McLucas B, Lee M, Chen G, Perrella R, Vedantham
S, et al. Uterine artery embolization for the treatment of uterine leiomyomata: mid-term results. J Vasc Interv Radiol 1999;10:1159- 1165
16. Pelage JP, Le Dref O, Soyer P, Kardache M, Dahan H, Abitbol M, et al. Fibroid-related menorrhagia: treatment with superselective embolization of the uterine arteries and mid-term follow-up.
Radiology 2000;215:428-431
17. Walker WJ, Green A, Sutton C. Bilateral uterine artery embolisa- tion for myomata: results, complications and failure. Min Invas Ther Allied Technol 1999;8:449-454
18. Siddle N, Sarrel P, Whitehead M. The effect of hysterectomy on the age at ovarian failure: identification of a subgroup of women with premature loss of ovarian function and literature review.
Fertil Steril 1987;47:94-100
19. Ravina JH, Vigneron NC, Aymard A, Le Dref O, Merland JJ.
Pregnancy after embolization of uterine myoma: report of 12 cas- es. Fertil Steril 2000;73:1241-1243
20. JH Hong, SH Song, JK Lee, MJ Oh, HS Saw, YK Park, et al.
Uterine artery embolization of leiomyoma. Korean J Obstet Gynecol 2004;47:481-486
21. YS Lee, M Hong, YS Koh, DS Cha, HI Choi, IB Chung, et al.
Clinical response of uterine embolization for the management of leiomyomas. Korean J Obstet Gynecol 2001;44:43-47
22. JS Park, DY Lee, YT Kim, KH Park, YW Park, JS Cho, et al.
Uterine arterial embolization for uterine leiomyoma : efficacy and clinical outcome. J Korean Radiol Soc 1999;41:481-485
23. Omary RA, Vasireddy S, Chrisman HB, Ryu RK, Pereles FS, Carr JC, et al. The effect of pelvic MR imaging on the diagnosis and treatment of women with presumed symptomatic uterine fibroids.
J Vasc Interv Radiol 2002;13:1149-1153
24. Ascher SM, Arnold LL, Patt RH, Schruefer JJ, Bagley AS, Semelka
RC, et al. Adenomyosis: prospective comparison of MR imaging and transvaginal sonography. Radiology 1994;190:803-806 25. Spies JB, Allison S, Flick P, McCullough M, Sterbis K, Cramp M, et
al. Polyvinyl alcohol particles and tris-acryl gelatin microspheres for uterine artery embolization for leiomyomas: results of a ran- domized comparative study. J Vasc Interv Radiol 2004;15:793-800
대한영상의학회지 2005;52:401-407
자궁 동맥 색전술을 이용한 자궁 근종의 치료1
1포천중문의과대학 분당 차병원 진단방사선과
2포천중문의과대학 분당 차병원 산부인과
김경아・김만득・김희진・이미화2・조진호2・차선희2・윤상욱・안은희2
목적:자궁 근종에 대한 자궁 동맥 색전술의 유용성에 대하여 알아 보고자 하였다.
대상과 방법:자궁 근종으로 인해 과다월경증, 생리통, 종괴 자체에 의한 압박 증상을 주소로 자궁동맥 색전술을 시행 받
은 69명의 환자를 대상으로 후향적 분석 하였다. 평균 연령은 40.3세(31-52세) 였으며, 평균 추적 기간은 3.5개월 (1-8개월)이며, 자궁 가장 큰 근종의 크기는 평균 5.8 cm(2.0-13.2 cm) 이었다. 색전 물질은 폴리비닐알코올 (250- 710 (μm)을 이용하였다. 시술 후 임상 경과에 대하여 조사 하였으며, 시술 전과 시술 후 MRI를 이용 하여 근종과 자궁 의 볼륨 감소를 측정하였다.
결과:과다 월경증은 87.5%, 생리통은 83.3%, 종괴에 의한 압박 증상은 79.2%에서 증상의 호전이 있었다. 부작용으로 는 4명(5.8%, 평균 연령 43.3세)의 환자가 난소 기능 부전이 와서 폐경이 되었고, 3명의 환자에서 감염 증상이 있어 항 생제 치료를 필요로 하였다. 자궁과 가장 큰 근종의 볼륨 감소는 각각 36.3%, 56.6%를 나타내었다.
결론:자궁 동맥 색전술은 자궁 근종으로 인한 증상 개선에 매우 효과적인 치료 방법이며 자궁 절제술을 대치 할 수 있 을 것으로 보인다.