Address reprint requests to Hyun Woo Reu, M.D.
Department of Rehabilitation Medicine, Honam Regional Rehabilitation Hospital Bonchondong, Bukgu, Gwangju, Korea
TEL: 82-62-220-3153 FAX: 82-62-223-0245, E-mail: gorea2@hanmail.net 투고일: 2013년 5월 23일, 수정일: 2013년 6월 12일, 게재확정일: 2013년 6월 12일
�이 논문은 2011학년도 조선대학교 학술연구비의 지원을 받아 연구되었음.
INTRODUCTION
Tethered cord syndrome (TCS) occurs when conus medullaris exists as far as the lower area of the second lumbar area or when the filum terminale is 2 mm thick or more, so that a lesion is caused due to compression injury, dragging in nerve roots or the spinal cord.
1.2In most cases, we can determine it suspicious, clinically speaking, when a patient suffers from a decline in motor and sensory func- tion which does not meet the normal expectation out of myotome, dermatome or paresthesia, or when such symp-
toms are accompanied with muscular atrophy, a change in muscle tone, spastic gait, urinary incontinence, scoliosis or malformation, such as the deformation of feet.
3.4In 1953, Garceau first introduced the syndrome by call- ing it “filum terminale syndrome”. Afterwards, in 1976, Hoffman & Colleagues et al. referred to patients as having
“tethered spinal cord”, who experienced such symptoms caused by the elongating of the spinal cord and/or filum terminale, or the thickening of filum terminale.
Most symptoms are caused by the extending of the spinal cord during adolescence as a result, these symptoms
49세까지 증상이 없었던 마르팡 증후군을 동반한 계류척수 증후군 환자 - 증례 보고 -
조선대학교 의과대학 재활의학교실, 호남권역재활병원�
강정훈∙한 용∙류현우�
– Abstract –
A Tethered Cord Syndrome with Marfan Syndrome in A 49-Year-Old Woman Who Has No Specific Symptoms - A Case Report -
Jung-Hun Kang, M.D., Yong Han, M.D., Hyun Woo Reu, M.D. *
Department of Rehabilitation Medicine, Chosun University Hospital, Gwangju, Korea, Honam Regional Rehabilitation Hospital, Gwangju, Korea
*계류척수 증후군(Tethered cord syndrome)은 척수의 신장과 척수 종말끈의 비후 등으로 척수가 견 인되면서 신경학적 이상을 일으키는 질환으로 대부분의 증상은 청소년기 이전에 발생한다. 본 증례는 마르팡 증후군을 가진 49세의 여성에서 요추부 자기공명영상 검사 상 마르팡 증후군에 의한 경막낭의 팽창과 함께 계류척수 증후군이 동반되어 관찰되었으나 40대 후반까지 특별한 신경학적 증상이 나타나 지 않았던 경우이다.
Key Words: Tethered cord syndrome, Marfan syndrome, Dural ectasia
– 54 –
are in some cases, mistakenly understood as pediatric problems, which could be adequately diagnosed when a patient finally comes of age. In the case of TCS (tethered cord syndrome) commonly found during the childhood, neurologic injury can be prevented by surgical treatment.
However, in many cases, for grown-ups having with con- genital TCS, it can be diagnosed as such only when symp- toms are clearly noticeable. In the case of congenital TCS in childhood, there have been numerous studies and litera- ture; however, in the case of TCS in adults, more develop- ment has yet to be made since there is no clear therapy in most instances. In this case, TCS and the inflating of dural sacs due to Marfan syndrome was observed in a 49-year old female patient after an MRI (Magnetic Resonance Imaging) was conducted on the lumbar spine. However, a remarkably abnormal neurologic symptom in the patient was not present until her late 40s. Therefore, this case needs to be reported.
CASE
A 49-year-old female patient with a height and weight of 172 cm and 52 kg, respectively, reported her chief complaint as lumbodynia (backache), edema in the right part of her lower limb, a decline in muscular strength, and paresthesia and so on. which occurred after she had been given a mitral valve replacement surgery 5 months before she came to our hospital. She was provided with a conservative treatment but continuously suffered from the symptoms. So, she finally came to the rehabilitation treatment center in our hospital. As a nurse working in our hospital, the patient has lived a healthy life without hypertension, diabetes mellitus, lumbodynia, or radiating pain in the lower limb, according to her anamnesis.
Having been diagnosed with tetralogy of Fallot and Marfan syndrome, she has only had regular checkups accordingly. A physical examination revealed that patel- lar tendon reflex on both sides and ankle jerk reflex were normal; manual muscle testing indicated that hip flexors, extensor, adductor, abductor and knee extensor muscles all showed 5/5, but knee flexor and ankle dorsiflexor muscles showed 4/4 on both sides, which indicates a decline in muscular strength. The dysesthesia reported by the patient was a blunt and benumbed sense. While it is not expected of dermomyotome, she reported discom- fort in many different areas of her body. A straight leg raising test found that it was positive at the angle of 50 degrees on the right side and 60 degrees on the left side,
but Patrick’s test found it to be negative.
In a motor nerve conduction study, for evaluating con- duction of the deep peroneal nerve, we gave stimuli to the peroneal nerve at the just lateral to the tibialis anterior tendon and 2 cm distal to the fibular head to record onset latency, amplitude and nerve conduction velocity of compound motor action potential obtained from the extensor digitorum brevis, all of which were normal.
Also, we gave stimuli to the tibial nerve posterior to the medial malleolus of the ankle and in popliteal space to record onset latency, amplitude and nerve conduction velocity of compound motor action potential taken in abductor hallucis, all of which were found to be normal.
Antidromic sensory nerve conduction study showed normal latency and amplitude in both the superficial peroneal nerve and sural nerve, and the latency of H- reflex on both sides were found to be delayed. In the motor evoked potentials test taken by way of giving stimuli to the cranial part and measuring potentials in abductor hallucis on both sides, the measured values were 42.7 ms on the right side and 42.3 ms on the left, respectively. In somatosensory evoked potential test of the tibial nerve on both sides, the values were 43.0 ms on the right and 42.7 ms on the left. We observed the find- ing of a slight delay in latency taken transcranially. The central motor conduction time taken in abductor hallucis was found to be 14.25 ms on the right and 14.15 ms on the left, which were somewhat delayed (Table 1). The needle electromyography showed that there were a lot of abnormal spontaneous activities in the paraspinal mus- cles and in the muscles of the lower limbs of the corre- sponding segments on both sides of L4 to S1.
MRI study of the lumbar spine indicated there is an enlargement of dural sacs caused by Marfan syndrome, and we diagnosed it as the condition accompanied with tethered cord syndrome. In order to check whether there is a neurological anomaly, we conducted an MRI study into the craniocervical (head and neck) and cervicospinal area, but found no abnormal finding. Afterwards, as a conservative treatment to a decline in muscle strength in both lower limbs, as well as dysesthesia, we are current- ly providing physiotherapy together with pregabalin and giving steady rehabilitation treatment. Currently, she is showing some improvement in dysesthesia.
DISCUSSION
Neurologic disorders known as tethered cord syn-
drome or occult spinal dysraphism sequence are caused by the malformation of the spinal cord and include sev- eral different types such as tight filum terminale, lipomeningomyelocele, split cord malformations, dermal sinus tracts, cycstoceles and so on, all of which have the common trait of pulling of the spinal cords inside spinal canals. Normally, the spinal cord is loosely bound inside the spinal canal and moves freely up and down to be bent or pulled. However, the tethered spinal cord is tight- ly bound at its end. It is common that in the course of growing up during childhood, the spinal cord is pulled and finally, in adulthood, the injury progress of the spinal cord may sometimes do permanent damage.
The symptoms in childhood can be characterized by hairy patches, dimples, or fatty tumors in the lower area of the waist, or malformation of the spine, weakness of the lower limb, lumbodynia, scoliosis, bladder inconti- nence and so on can be found in the region where the tethered cord is located. When paresthesia or motor abnormality as a symptoms is not found, it is not diag- nosed until adulthood in some cases.
3.4The characteristic symptom found in adults may include a pain in the lumbar area or a severe radiating pain in the lower limb, inguinal area, or perineum, as well as muscular weakness, a blunt sense or sensory extinction in both limbs, rectal and urinary incontinence, etc. As for neurologic symptoms, a mixture of the dam- age to the upper and lower motor neurons can be shown such as amyotrophy, hyperreflexia, or abnormal plantar reflex. In many instances, the remarkable change in sense may include pain or a sensory extinction of tem-
perature or proprioceptor sense. Also, chronic re-infec- tion and renal disease can be occured frequently, such as pyelonephritis or renal failure due to renal calculi.
Female patients can show intestinal hernia or miscar- riage after parturition by atonia of pelvic floor.
For treatment, it is recommended that an early opera- tion be conducted as soon as possible, before the symp- tom is vividly displayed and worsened, because neuro- logic injury progresses in an irreversible way. Often, it may be involved in Chiari malformation or Ehlers-Dan- los syndrome, so there is a need to make a differential diagnosis for these disorders.
According to her anamnesis, the patient stated she has never had any neurologic symptom such as the pain in the lumbar area or radiating pain in both limbs and so on. Because her primary complaints included suffering from backaches, a decline in muscle strength or pares- thesia in both lower limbs, which occurred after the mitral valve replacement surgery, she visited the hospital.
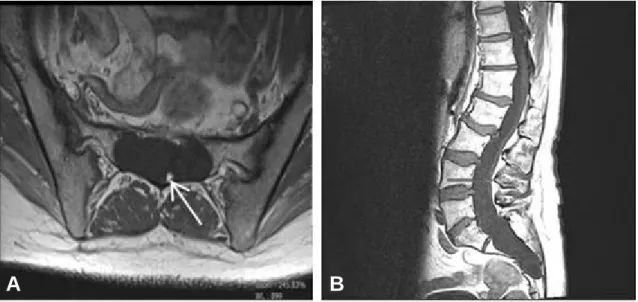
The simple radiological imaging and hematological studies did not show any abnormal findings, and even the nerve conduction study did not reveal any abnormal findings. However, needle electromyography revealed abnormal spontaneous activities in both lower limbs and the lumbar area, which was diagnosed as lumbosacral radiculopathy. As a more detailed test, we conducted an MRI study in the lumbar area. In this test, fatty filum terminale thickened to as much as 3.5 mm in the T1 axial image, while a filum normally has a thickness of about 2 mm or less. Even in the sagittal image, low- lying conus could be recognized in the lower part of the
Table 1. Electrophysiologic FindingsRight Left
OL Amplitude CV Latency OL Amplitude CV Latency
(msec) (mV/μV) (m/s) (msec) (msec) (mV/μV) (m/s) (msec)
SNAP
Sural 2.0 20.0 2.3 21.5
Superficial peroneal 2.3 21.0 2.5 22.7
CMAP
Peroneal (EDB) 3.0 7.6 44 3.5 8.5 44
Tibial (AH) 5.6 20.9 42 5.2 18.6 43
H-reflex (GCM) 32.2 32.5
SEPs (Posterior tibial nerve) 43.0 42.7
MEPs (AH) 42.7 42.3
CMCT (AH) 14.25 14.15
OL: Onset latency, CV: Conduction velocity, SNAP: Sensory nerve action potential, CMAP: Compound muscle action potentials, SEPs: Somatosensory evoked potentials, MEPs: Motor evoked potentials, CMCT: Central motor conduction time, EDB: Extensor digitorum brevis muscle, AH: Abductor hallucis muscle, GCM: Gastrocnemius muscle.
– 56 –
second lumbar vertebra (Fig. 1). A brain MRI study, as well as MRIs in the craniocervical (head and neck) area showed no Arnold-Chiary malformation and no abnor- mal findings. According to the anamnesis of the patient, there has been tetralogy of Fallot as well as Marfan syn- drome, so she is taller than the average height of a woman by far; her arms and legs are unusually long.
MRI study of the lumbar spine revealed enlargement of dural sacs and other abnormal findings, which patients with Marfan syndrome often develop.
Marfan syndrome is a kind of genetic disorder that brings out the anomaly of connective tissue its most severe complications may include anomalies of the heart valve and abnormal aorta, or may cause abnormalities of connective tissues surrounding the eyes, the lungs, the spinal cord, or some disorders of the skeletal system, such as tall stature, span greater than height, pectus cari- natum or pectus excavatum, long slender limbs with arachnodactyly, and wrist and thumb signs and so on.
It cannot be diagnosed merely by the observation of abnormal appearance, but can be determined by clinical symptoms and laboratory findings in the non-skeletal system, in particular, by abnormalities of the eyes, aorta, or heart. One of the most remarkable examples in the anomalies of the skeletal system is that the patient is taller than average height and having longer fingers and toes. In addition, scoliosis, sternal pectus excavatum, or pectus carinatum can be found, even though not common.
The sign of the central nervous system (CNS) of Mar- fan syndrome can show inflating dural sacs due to weak-
ness of the connective tissues of dura mater surrounding the spinal cord. They may cause pain in the lumbar area, pain in the lower limbs, abdominal pain, a neurologic symptom in lower limb, or headache. While a patient lies on her back, the symptoms may be mitigated or some- times do not show specific symptoms. Ahn et al. sug- gested two kinds of primary diagnostic criteria about dural ectasia. First, the width of the dural sacs below the fifth lumbar vertebra should be wider than those of above the fourth lumbar vertebrae. Second, there should be the anterior sacral meningocele. As for minor criteria of diagnosis, he suggested that the diameter of nerve sleeve should be wider than 6.5 mm at level of the fifth lumbar vertebra and the diameter of scalloping should be wider than 3.5 mm at level of the first sacral vertebrae.
They suggested the diagnosis can be made only if there is one main standard and two minor standards.
5-7In the case of the patient here, the inflating of dural sacs that begins from the first lumbar vertebra can be observed in the T1-weighted sagittal MR image. In the T2-weighted transverse MR image, it can be observed that the inflating progressed and extended up to the peripheral tissues and the anterior part of sacral vertebra part. The dural sac of the fifth lumbar vertebra is as wide as 20.76 mm, which is wider than the 19.26 mm of the fourth lumbar vertebra. It has been found that myelomeningocele occurs on both sides and in front due to bony defect of sacral vertebra (Fig. 2). The imaging study showed scalloping of the first sacral vertebra with the value of 4.29 mm, satisfying the diagnostic criteria
Fig. 1. MRI images showing a fatty filum terminale (arrow) bright on T1 image (A), and low-lying conus medullaris (B).
A B
(Fig. 3).
In order to make a quantitative evaluation, Oosterhof et al. calculated the ratios of the inflating of dural sacs as an indicator for the diagnosis of Marfan syndrome by computing and dividing the diameters of dural sacs at the each vertebral levels with the diameters from the first lumbar vertebral body to the first sacral vertebral body, respectively, among the 44 normal subjects. They report- ed the values of dural sac ratio from the first lumbar ver- tebra to the first sacral vertebra should be less than 0.64, 0.55, 0.47, 0.48, 0.48 and 0.57 mm as being normal, respectively. Also, the dural sac ratios were found to have 95% sensitivity and 98% specificity from the third lumbar vertebra to the first sacral vertebra in the same
number of patients diagnosed with Marfan syndrome.
The calculation of the dural sac ratios from the third lumbar vertebra to the first sacral vertebra in this patient showed respective values of 0.59, 0.59, 0.69, and 0.98 mm
8(Fig. 4), which were greater than the diagnostic cut- off values.
The patient, as stated above, has tethered cord syndrome and has not been diagnosed as having had the disorder in her juvenile period or adulthood. However, after the operation of mitral valve replacement owing to Fallot’s syndrome, she suffered from weakness and dysesthesia in both lower limbs. The nerve conduction studies did not show significant abnormal findings, but needle elec- tromyography revealed abnormal spontaneous activities
Fig. 2. T1 weighted sagittal and axial MRI scans of lumbosacral spine. Arrows indicate the anterior sacral meningocele.A B
Fig. 3. The width of the dural sac at the level of L5 is greater than L4 and the scalloping of S1 is greater than 3.5 mm.
Fig. 4. Sagittal T2 weighted MR images of the lumbosacral spine show measurment of vertebral body diameters and dural sac diameters.
in the lumbar area and both lower limbs. For further evaluating of this patient’s neurologic symptoms with abnormal needle electromyography and somewhat delayed central motor conduction time, we conducted MRI study of the lumbar spine and diagnosed her as hav- ing tethered cord syndrome. This is exceptional as com- pared to common cases in which tethered cord syndrome is normally diagnosed before adulthood.
CONCLUSION
In this study, we reported a case of Marfan syndrome with dural sac inflation began from the first lumbar ver- tebra complicated by tethered cord syndrome. The patient is taller than the average body height, so symp- toms could have been found in earlier age. However, this patient did not show any neurologic symptoms until her late 40’s.
REFERENCES
1. Fitz CR, Harwood-Nash DC: The tethered conus. Am J Roentgenol 1975: 125: 515-523.
2. Newton TH, Potts DG: Computed tomography of the
spine and spinal cord. Spinal dysraphism Vol. 1. San Anselmo, CA: Clavadel press 1983: 299-354.
3. Barson AJ: The vertebral level of termination of the spinal cord during normal and abnormal development. J Anat 1970: 106: 489-497.
4. Smoker WRK, Godersky JC, Knutzon RK, Keyes WD, Norman D, Bergman W: The Role of MR imaging in eval- uating metastatic spinal disease. Am J Roentgenol 1987:
149: 1241-1248.
5. Ahn NU, Sponseller PD, Ahn UM, Nallamshetty L, Rose PS, Buchowski JM, et al: Dural ectasia in the Marfan syn- drome: MR and CT findings and criteria. Genet Med 2000: 2: 173-179.
6. Janjua MZ, Muhammad F: Measurements of the normal adult lumbar spinal canal. J Pak Med Assoc 1989: 39:
264-268.
7. Villeirs GM, Van Tongerloo AJ, Verstraete KL, Kunnen MF, De Paepe AM: Widening of the spinal canal and dural ectasia in Marfan’s syndrome: assessment by CT.
Neuroradiology 1999: 41: 850-854.
8. Oosterhof T, Groenink M, Hulsmans FJ, Mulder BJM, van der Wall EE, et al: Quantitative assessment of dural ecta- sia as a marker for Marfan syndrome. Radiology 2001:
220: 514-551.
– 58 –