Preoperative Assessment of Mesorectal Fascial
Involvement in Patients with Rectal Cancer: The Diagnostic Value of MDCT for Measuring the Mesorectal Fascial Thickness1
Min-Jeong Seo, M.D., Jung-Hee Yoon, M.D., Eun-Joo Lee, M.D., Seong-Sook Cha, M.D., Sang-Suk Han, M.D.
1Department of Radiology, College of Medicine, Inje University, Busan Paik Hospital Received April 12, 2007 ; Accepted July 6, 2007
Address reprint requests to : Jung-Hee Yoon, M.D., Department of Radiology, Busan Paik Hospital, Inje University, College of Medicine, 633-165, Gaegum-dong, Busanjin-gu, Busan 614-735, Korea.
Tel. 82-51-890-6728 Fax. 82-51-896-1085 E-mail: Minkimom @ yahoo.co.kr
Purpose: To assess the diagnostic value of the use of multi-detector row computed to- mography (MDCT) in evaluating mesorectal fascial (MRF) involvement in patients with T3 stage rectal cancer.
Materials and Methods: From September 2005 to June 2006, we enrolled 21 patients with T3 stage rectal cancer. In addition, 21 healthy patients were enrolled in a control group. Two radiologists measured the mean MRF thickness independently. We consid- ered positive MRF involvement when the MRF thickness exceeded 4 mm, and then we measured the MRF thickness of patients with T3 rectal cancer. We analyzed inter- observer agreement for the measured MRF thickness of the control group and as- sessed the diagnostic value of 4 mm, 5 mm and 6 mm as references in predicting MRF involvement.
Results: The mean MRF thickness of the control group was 3.24±0.50 mm (radiolo- gist 1) and 3.04±0.51 mm (radiologist 2). Using 4 mm, 5 mm and 6 mm as a reference thickness in predicting MRF involvement, sensitivity was 100%, 100% and 28.57%, specificity was 71.43%, 85.71% and 92.86%, the false negative rate (FNR) was 0%, 0%
and 71.43%, the false positive rate (FPR) was 28.57%, 14.29% and 7.14%, the negative predictive value (NPV) was 100%, 100% and 72.2%, the positive predictive value (PPV) was 63.64%, 77.78% and 66.7%, and the accuracy was 80.95%, 90.48% and 71.43%.
Conclusion: Preoperative assessment of the MRF thickness on MDCT is beneficial in predicting MRF involvement in patients with advanced rectal cancer and a value of 5 mm as a reference MRF thickness was established.
Index words :Fascia, mesorectum Rectal neoplasms
Tomography, X-ray computed Rectum
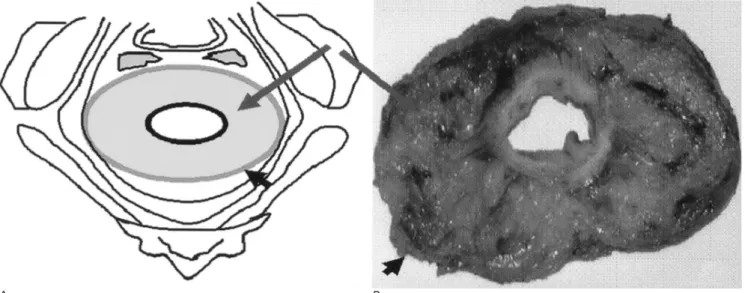
Rectal cancer is a common disease with a high mortal- ity rate in Western countries and is on the increase in Korea (1). The standard surgical procedure for rectal cancer is en bloc resection of the tumor and total mesorectal excision (TME). The local tumor recurrence is strictly dependent upon the circumferential resection margin (CRM) and the mesorectal fascia represents the CRM when TME is used as the surgical approach (Fig.
1) (2, 3). A local tumor recurrence after resection of a rectal cancer occurs in 3-32% of patients. Complete TME results in reduced local tumor recurrence rates be- low 10% without additional radiotherapy. Preoperative neoadjuvant radio- or chemotherapy is needed for pre- vention of the local tumor recurrence in patients with a close or involved resection margin (4-8).
To achieve the treatment plan for reducing local tu- mor recurrence, the anticipated plan of the TME must be evaluated. Magnetic resonance (MR) imaging has been reported to be highly accurate in the prediction of a wide or involved CRM by measuring the shortest dis- tance between the tumor and mesorectal fascia (5, 9, 10).
In clinical practice, many centers in Korea perform computed tomogrphy (CT) for the initial staging of rectal cancer. However, there are few studies on the role of CT in assessing mesorectal fascial involvement with ad- vanced rectal cancer (7)
We have experienced that there is difficulty in mea- suring the shortest distance between the tumor/or metastatic lymph node and mesorectal fascia using mul-
ti-detector row computed tomography (MDCT), as there is a limitation of the low spartial resolution and a prob- lem of differentiation between a benign reactive lymph node and a metastatic lymph node. According to one study, the mesorectal fascia is better seen with MDCT than with MR, particularly in patients with gross obesity (4).
In this study, we attempted to assess the diagnostic value of the mesorectal fascial thickness on MDCT in evaluating mesorectal fascial involvement in patients with histopathologically proven T3 stage rectal cancer.
Materials and Methods
Patients
From September 2005 to June 2006, we selected 40 patients with histopathologically proven T3 stage rectal cancers that underwent preoperative MDCT. Of these patients, 19 patients were excluded because they under- went preoperative radio- or chemotherapy; thus the study population comprised 21 patients (9 males and 12 females; median age, 59.5 years; age range, 33-83 years).
For a control group, we enrolled 21 patients without any rectal and perirectal pathology (control group; 12 males and 9 females; median age, 58 years; age range, 34-80 years).
CT scans
All patients underwent contrast-enhanced ab-
A B
Fig. 1. A diagram and surgical specimen of the normal mesorectum and mesorectal fascia. In A (diagram) and B (surgical speci- men), the rectum is surrounded by fatty tissue that forms a structure known as the mesorectum (long arrows). The mesorectum is surrounded by the mesorectal fascia (short arrows), which represents the circumferential resection margin (CRM) when TME is used as the surgical approach.
dominopelvic MDCT. All preoperative MDCT scans were obtained within a 6-week period before surgery (mean interval, 38 days). All CT studies were performed with a four-detector row scanner (Simens Medical Solutions, Erlangen, Germany) or a sixty-four detector row scanner (Toshiba, Nasu Shiobara, Japan). The scan- ning parameters for the four-detector row CT were 5- mm section thickness, pitch of 6, tube current of 120 kVp, 120 mAs. The scanning parameters for the sixty- four detector row CT were 5-mm section thickness, pitch of 0.5, tube current of 120 kVp, and 350-400 mAs. An nonionic contrast material (100 ml, Iopromide, UltravistⓇ370; Schering, Berlin, Germany) was injected intravenously at a rate of 3-4 mL/sec by using a power injector. Oral contrast media, rectal contrast media and air insufflation were not used.
Scans were acquired in a craniocaudal direction from the level of the diaphragm to the anus during one breath-hold. The delay between the beginning of con- trast material injection and image acquisition was 45 seconds for patients with a primary rectal cancer and 120 seconds or 180 seconds for the control group pa- tients.
Image Analysis
We retrospectively reviewed imaging findings by us- ing the cine mode on the picture archiving and commu- nication system viewer (Marotech, Seoul, Korea).
Independently, two radiologists (J.H.Yoon, M.J.Seo) measured the greatest thickness of the mesorectal fascia of the control group patients. The two radiologists using a consensus approach measured the mesorectal fascial thickness. Based on the mean mesorectal fascial thick-
ness of the control group patients, we considered as pos- itive mesorectal fascial involvement when the mesorec- tal fascial thickness was more than 4 mm. Radiological mesorectal fascial involvement was then compared with histopathological mesorectal fascial involvement. All histopathologialc assessment was performed after surgi- cal excision with TME.
Statistical analysis
In measuring the mean mesorectal fascial thickness of the control group patients, interobserver agreement was analyzed using the Pearson coefficient and paired t-test.
A p value of less than 0.05 was considered statistically significant. We analyzed the sensitivity, specificity, false negative rate (FNR), false positive rate (FPR), positive predictive value (PPV), negative predictive value (NPV) and accuracy of three different reference points (4 mm, 5 mm and 6 mm) in the predicting the involved mesorectal fascia.
Results
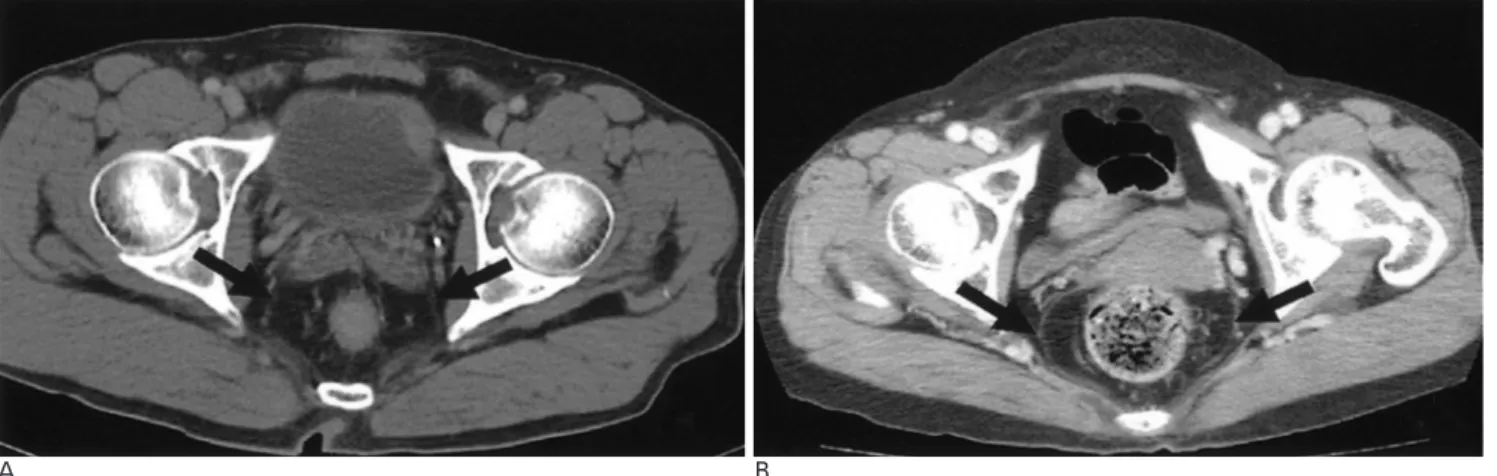
The mean mesorectal fascial thickness of the control group patients was 3.24±0.50 mm (as determined by radiologist 1) and 3.04±0.51 mm (as determined by ra- diologist 2) (Fig. 2). In measuring the mean mesorectal fascial thickness of the control group patients, the Pearson coefficient was 0.847 and the p-value was less than 0.001, indicating an excellent correlation between the two radiologists.
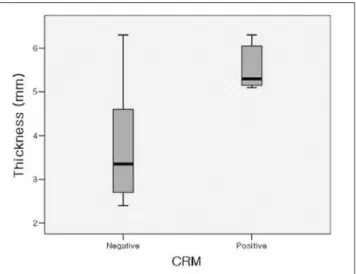
Under the consensus approach, the mesorectal fascial thickness was 3.70±1.22 mm (total of 14 cases; range, 2.7-6.3 mm) in the negative CRM group of patients and
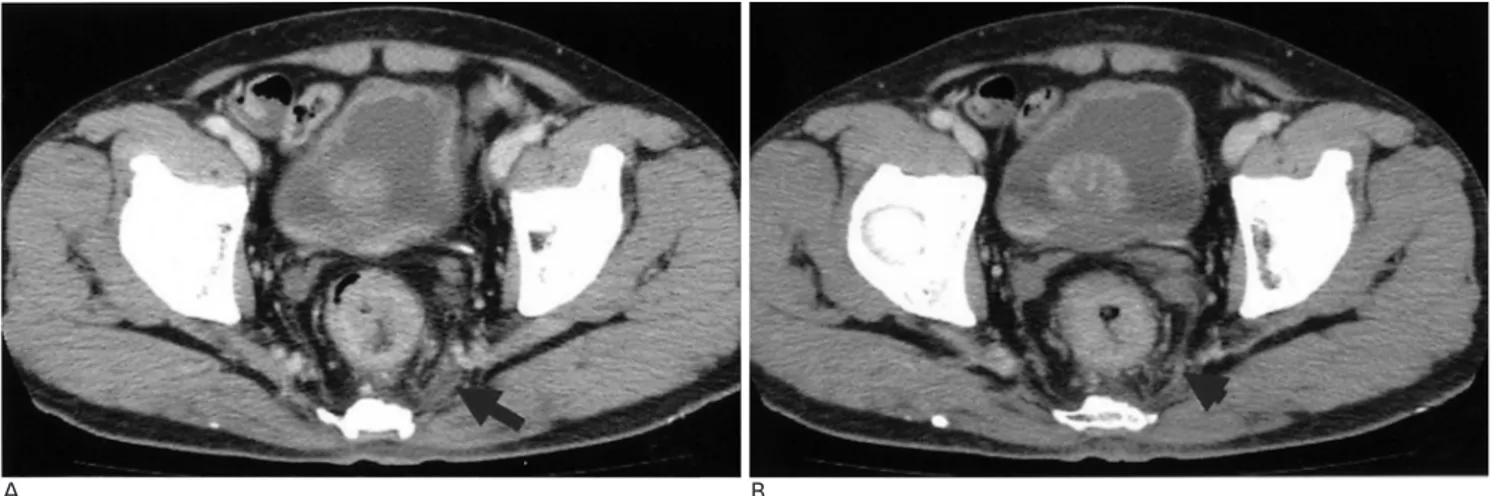
A B
Fig. 2. The normal mesorectum and mesorectal fascia on axial MDCT scans in a male (A) and female (B) patient. The mesorectum is seen as hypodense and the mesorectal fascia is delineated as a thin, curvilinear structure of similar density of the muscle adja- cent to the rectum.
5.59±0.53 mm (total of 7 cases; range, 5.1-6.3 mm) in the positive CRM group of patients. The distributions are shown on graph 1.
When we used 4 mm as a reference mesorectal fascial thickness on axial MDCT scans, 11 cases were interpret- ed as having an involved mesorectal fascia but on histopathology, 7 cases had an involved mesorectal fas- cia. There were four false positive cases. The sensitivity was 100%, specificity was 71.43%, the FNR was 0%, the FPR was 28.57%, PPV (Fig. 3) was 63.64%, NPV (Fig. 4) was 100% and accuracy was 80.95%.
When we used 5mm as a reference mesorectal fascial thickness on axial MDCT scans, 9 cases were interpret-
ed as having an involved mesorectal fascia. There were two false positive cases. The sensitivity was 100%, specificity was 85.71%, the FNR was 0%, the FPR was 14.29%, PPV was 77.78%, NPV was 100% and accuracy was 90.48%.
When we used 6mm as a reference mesorectal fascial thickness on axial MDCT scans, 3 cases were interpret- ed as having an involved mesorectal fascia. There was one false positive case and five false negative cases. The sensitivity was 28.57%, specificity was 92.86%, the FNR was 71.43%, the FPR was 7.14%, PPV was 66.7%, NPV was 72.2% and accuracy was 71.43% (Table 1).
Discussion
The rectum is surrounded by fatty tissue that forms a structure known as the mesorectum. The mesorectum contains lymph nodes, vessels, and several fibrous septa and is surrounded by the mesorectal fascia. The mesorectal fascia has been defined as the fine linear structure enveloping the mesorectum, which represents
Graph 1. Distribution chart of mesorectal fascial thickness in the rectal cancer group; the mean mesorectal fascial thickness was 3.70±1.22 mm (total of 14 cases; range, 2.7-6.3 mm) in the nega- tive CRM group and 5.59±0.53 mm (total of 7 cases; range, 5.1- 6.3 mm) in the positive CRM group.
A B
Fig. 3. A positive CRM in a 33-year-old man.
A. On an axial contrast enhanced MDCT image, the mesorectal fascia in the right posterolateral aspect is thickened to 6.3 mm (ar- row).
B. On histopathology, tumor cell infiltrations are identified in the stained mesorectal fascia (arrowheads).
Table 1. Statistical Parameters and Results of Mesorectal Fascial Involvement According to the Thickness of the Mesorectal Fascia Determined on Axial MDCT
4 mm (%) 5 mm (%) 6 mm (%)
Sensitivity 100 100 28.57
Specificity 71.43 85.71 92.86
False negative rate 0 0 71.43
False positive rate 28.57 14.29 07.14
Accuracy 80.95 90.48 71.43
Positive predictive value 63.64 77.78 66.7 Negative predictive value 100 100 72.2
the CRM when TME is used as the surgical approach (3- 5, 9). The use of TME is an accepted procedure for the surgical treatment of rectal cancer as part of either ante- rior resection or abdominoperineal excision (4). The use of TME implies the complete excision of all of the mesorectum enclosed within the mesorectal fascia. This dissection is performed in a circumferential manner down to the levator muscles to produce a globular, bilobed tissue block (2).
The most important factor, particularly in terms of lo- cal tumor recurrence, is CRM involvement. Although a complete TME results in reduced local tumor recur- rence rates, in the U.S.A., postoperative chemotherapy combined with radiothepapy has been used for the treatment of patients with T3/N1 tumors. In Europe, preoperative radiotherapy is also used for treatment of rectal cancers for patients with fixed tumors. For pa- tients with a close or involved resection margin, preop- erative neoadjuvant radio- or chemotherapy are needed for prevention of the local recurrence (4-8).
This study shows the normal mesorectal fascial thick- ness on MDCT and the diagnostic value of the mesorec- tal fascial thickness in predicting mesorectal fascial in- volvement in patients with advanced rectal cancer.
There was a previous report about the effect of rectal distension and implications for preoperative prediction of tumor-free circumferential resection margin on MR (10). For exclusion of the possibility that rectal insuffla- tion influenced the mesorectal fascial thickness, we did not use rectal contrast media or air insufflation during the performance of the MDCT scans.
In this study, there was a different scan interval used for the primary rectal cancer group of patients and the control group of subjects. It was not that we intended to assess the enhancement pattern, but that we intended to measure the thickness. We believed that the different scan intervals would not influence the thickness itself.
The mesorectal fascia limited mesorectum showed hy- podensity, and the mesorectal fascia itself was seen as a thin, curvilinear structure of similar density of the mus- cle adjacent to the rectum (3). Usually, the mesorectal fascia is best visualized at the level of the middle portion of the acetabulum. As there is an abundant fatty compo- nent, the mesorectal fascia can be more clearly visual- ized.
It is believed that CT has a low tissue contrast resolu- tion as compared to MR. Taking the circumstances into consideration, we used 1 mm-intervaled three different standpoints as references in the predicting the mesorec- tal fascial involvement. However, we believe that the spatial resolution of MDCT can well delineate the mesorectal fascia itself in spite of the inherent lower contrast resolution than that of MR and all the mesorec- tal fascias were well visualized in our study.
In our study, the mean mesorectal fascial thickness of the positive CRM group of patients as determined by histopathology was significantly thicker than that of the other groups.
The specificity was elevated and the false positive rate was reduced as the reference mesorectal fascial thick- ness was thicker. Using 6 mm as a reference mesorectal fascial thickness showed the lowest sensitivity, lowest
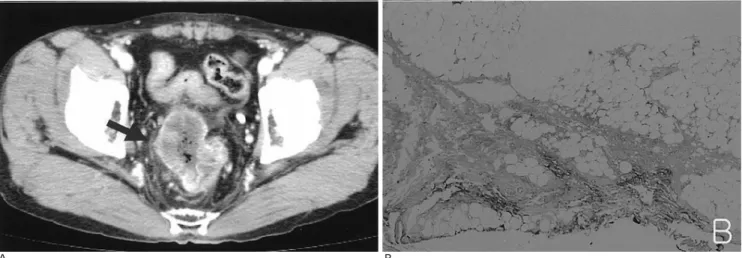
A B
Fig. 4. An negative CRM in a 57-year-old man.
A. On an axial contrast enhanced MDCT image, the distance between the tumor and mesorectal fascia is very close, but there is no evidence of mesorectal fascial thickening (arrow).
B. On histopathology, there is no evidence of tumor cell infiltration in the mesorectal fascia.
NPV, lowest accuracy and highest FNR. We consider that 5 mm as a reference mesorectal fascial thickness is the most valuable cut-off value in the predicting the mesorectal fascial involvement in patients with ad- vanced rectal cancer.
There were several false positive cases. One was pseu- do-thickening due to a partial volume averaging effect between the mesorectal fascia and presacral fascia (Fig.
5). The mesorectal fascia has a close and delicate anatomic relation with its boundaries. It is attached pos- teriorly to the presacral fascia by the Waldeyer fascia.
The rectovaginal fascia is present anteriorly and attach- es to the perineal body inferiorly, the uterosacral liga- ments superiorly, and the arcus tendineus fascia pelvis
laterally (11). The partial volume between the mesorec- tal fascia and these structures can lead to misinterpreta- tion. In another negative CRM case, the mesorectal fas- cial thickness was 4.2 mm. On histopathology, it showed a close CRM in which the shortest distance be- tween tumor infiltration and the mesorectal fascia was 2 mm (Fig. 6). Most histopathologists define the surgical margin as involved if the tumor extends to within 1 or 2 mm of the CRM and clinically, close and involved CRM are similarly treated and need preoperative neoadjuvant therapy. The mesorectal fascial thickness was thicker than 5 mm in two cases. One case showed a thickness of 5.6 mm and the other case showed a thickness of 6.3 mm. These levels resulted from benign mesorectal fas-
A B
Fig. 5. An false positive CRM due to partial volume averaging in a 70-year-old man.
A. On an axial contrast enhanced MDCT image, the mesorectal fascia in the left posterolateral aspect is thickened to 4.6 mm (ar- row), suggesting a positive CRM.
B. At 5 mm below the level in A, the mesorectal fascial thickness is normal (arrowhead). On histopathology (data not shown), there is no evidence of tumor cell infiltration in the mesorectal fascia.
A B
Fig. 6. An false positive CRM in a 61-year-old man.
A. On an axial contrast enhanced MDCT image, the mesorectal fascial thickness is 4.2mm (arrow), so it was considered as a posi- tive CRM.
B. On histopathology, there is no evidence of mesorectal fascial involvement. However, the shortest distance between the mesorectal fascia and tumor cell infiltration is 2 mm (arrow).
cial thickening from inflammatory cell infiltration or desmoplatic reactions. It is very difficult to differentiate between a desmoplastic reaction caused by fibrosis and true tumor cell infiltration because of the radiological similar findings.
We selected pathologically proven T3 stage rectal can- cers as prognostically T3 tumors are the most important tumors to be accurately assessed as current trends advo- cate the use of neoadjuvant therapies. Preoperative stag- ing using CT scans in rectal cancer patients was first re- ported in the early 1980s. Early reports with conven- tional CT mainly focused on locally advanced rectal can- cer and the accuracies for the T3 stage were 79-94%
(12-14). Most early studies were performed using non- helical CT units that were limited by a lack of the high resolution, thin collimation images achievable by the current MDCT instruments. According to Mathur et al.
(8), CT was significantly understaging T3 tumors com- pared to MR and majority of patients were staged as T2 by CT. Recently MDCT has been used to stage rectal cancer with a reported accuracy of over 90%. MDCT al- lows the use of thinner collimation with improved mul- tiplanar reconstruction (MPR) images. Non-axial images have been used in MR imaging for the staging of rectal cancer, but on MDCT, MPR images are possible within a single breath-hold. MPR images are particularly useful as they can be aligned parallel or perpendicular to the axis of the tumor, similar to the MR image, and can pro- vide more accurate staging (15, 16).
This study has several limitations. First, most studies about mesorectal fascial assessment in rectal cancer is evaluated using the shortest distance between the tumor and mesorectal fascia. However, we ignored this evalua- tion in the assessment of the CRM. To overcome the false positive rate, a further study will be needed in combination with determination of the mesorectal fas- cial thickness and shortest distance between the tumor and mesorectal fascia. Second, we did not use MPR im- ages of the MDCT that can give coronal and sagittal im- ages. By using these images, more accurate information characterizing the anatomical relationship for the mesorectal fascia and the adjacent structures, including the anal sphincter, may be obtained. Third, CT has a low tissue contrast resolution as compared with MR.
This can influence the identification of the mesorectal fascia and the measurement of the mesorectal fascial thickness on CT scans, but all the mesorectal fascias were well visualized in our study. Finally, the use of 5 mm as a reference mesorectal fascial thickness was the
most valuable in predicting the mesorectal fascial in- volvement in advanced rectal cancer in our study.
However, the number of samples is too small for gener- alization. Further evaluation with a large population will be needed.
We conclude that preoperative assessment of the mesorectal fascial thickness on axial MDCT scan is ben- eficial in predicting the mesorectal fascial involvement in patients with advanced rectal cancer and the use of 5 mm as a reference mesorectal fascial thickness is valu- able in predicting mesorectal fascial involvement in ad- vanced rectal cancer.
References
1. Eun CS. Chemoprevention of colorectal cancer: can it be possible by food? Korean J Gastroenterol 2005;45:68-72
2. Chapuis P, Bokey L, Fahrer M, Sinclair G, Bogduk N. Mobilization of the rectum: anatomic concepts and the bookshelf revisited. Dis Colon Rectum 2002;45:1-9
3. Iafrate F, Laghi A, Paolantonio P, Rengo M, Mercantini P, Ferri M, et al. Preoperative staging of rectal cancer with MR Imaging: corre- lation with surgical and histopathologic findings. Radiographics 2006;26:701-714
4. Diop M, Parratte B, Tatu L, Vuillier F, Brunelle S, Monnier G.
“Mesorectum” : the surgical value of an anatomical approch. Surg Radiol Anat 2003;25:290-304
5. Beets-Tan RG, Beets GL, Vliegen RF, Kessels AG, Van Boven H, De Bruine A, et al. Accuracy of magnetic resonance imaging in prediction of tumour-free resection margin in rectal cancer surgery. Lancet 2001;357:497-504
6. Wang C, Zhou Z, Wang Z, Zheng Y, Zhao G, Yu Y, et al. Patterns of neoplastic foci and lymph node micrometastasis within the mesorectum. Langenbecks Arch Surg 2005;390:312-318
7. Sinha R, Verma R, Rajesh A, Richards CJ. Diagnostic value of mul- tidetector row CT in rectal cancer staging: comparison of multipla- nar and axial images with histopathology. Clin Radiol 2006;61:924- 931
8. Mathur P, Smith JJ, Ramsey C, Owen M, Thorpe A, Karim S, et al.
Comparison of CT and MRI in the pre-operative staging of rectal adenocarcinoma and prediction of circumferential resection mar- gin involvement by MRI. Colorectal Dis 2003;5:396-401
9. Michael R. Torkzad, Blomqvist L. The mesorectum: morphomet- ric assessment with magnetic resonance imaging. Eur Radiol 2005;
15:1184-1191
10. Slater A, Halligan S, Taylor SA, Marshall M. Distance between the rectal wall and mesorectal fascia measured by MRI; effect of rectal distension and implications for preoperative prediction of tumour- free circumferential resection margin. Clin Radiol 2006;61:65-70 11. Pannu HK, Kaufman HS, Cundiff GW, Genadry R, Bluemke DA,
Elliot K. Dynamic MR imaging of pelvic organ prolapse: spectrum of abnormalities. Radiographics 2000;20:1567-1582
12. Thoeni RF, Moss AA, Schnyder P, Marguris AR. Detection and staging of primary rectal and rectosigmoid cancer by computed to- mography. Radiology 1981;141:135-138
13. Zannbauer W, Haertel M, Fuchs WA. Computed tomography in carcinoma of the rectum. Gastrointest Radiol 1981;6:79-84 14. Van Waes PF, Koehler PR, Feldberg MA. Management of rectal
carcinoma: impact of computed tomography. AJR Am J Roentgenol 1983;140:1137-1142
15. Kulinna C, Eibel R, Matzek W, Bonel H, Aust D, Strauss T, et al.
Staging of rectal cancer: diagnostic potential of multiplanar re- constructions with MDCT. AJR Am J Roentgenol 2004;183:421-427
16. Matsuoka H, Nakamura A, Masaki T, Sugiyama M, Takahara T, Hachiya J, et al. Preoperative staging by multidetector row com- puted tomography in patients with rectal carcinoma. Am J Surg 2002;184:131-135
대한영상의학회지 2007;57:349-356
직장암 환자에서 수술 전 직장간막의 침범여부: 다검출기 전산화 단층촬영을 이용한 직장간막 두께 측정의 진단적 의미1
1인제대학교 부산백병원 영상의학과 서민정・윤정희・이은주・차성숙・한상석
목적: T3 병기 직장암 환자의 MDCT상 직장간막 두께 측정이 직장간막 침범 여부 진단에 도움이 되는지 알고자 하였 다.
대상과 방법: 최근 MDCT를 시행한 대조군 21명에서 두 명의 영상의학과 의사가 독립적으로 평균 정상 직장간막 두께 를 측정하여 4 mm 이상을 비후된 것으로 정하고, 술 후 T3 병기 직장암 환자 21명에서 합의로 직장간막 두께를 측정 하였다. 대조군의 평균 직장간막 두께를 바탕으로 4 mm 이상일 때 직장간막 침범으로 보고, 정상군에서 관찰자 간 일 치도, 직장간막 두께를 4 mm, 5 mm, 6 mm 기준으로 각각에서 직장암환자의 직장간막 침범 여부에 대한 진단적 가치 를 평가하였다.
결과: 대조군의 평균 정상 직장간막 두께는 3.24±0.50 mm(관찰자 1), 3.04±0.51 mm(관찰자 2)로 통계학적으로 의 미 있는 관찰자 간 일치율을 보였고, 직장간막 두께 기준 4 mm, 5 mm, 6 mm 각각에서, 직장암환자의 직장간막 침범여 부 평가에 대한 MDCT의 민감도는 100%, 100%, 28.57%, 특이도 71.43%, 85.71%, 92.86%, 위음성률0%, 0%, 71.43%, 위양성률 28.57%, 14.29%, 7.14%, 음성예측도 100%, 100%, 72.2%, 양성예측도 63.64%, 77.78%, 66.7%, 정확도 80.95%, 90.48%, 71.43%였다.
결론: MDCT상 직장간막 두께 측정은 직장암의 직장간막 침범 여부 진단에 도움이 되며, 직장간막 두께 5 mm 기준에 서 가장 높은 정확도를 보였다.