112
접수번호:08-012
Korean Journal of Ophthalmology 2009;23:112-113
ISSN : 1011-8942 DOI : 10.3341/kjo.2009.23.2.112
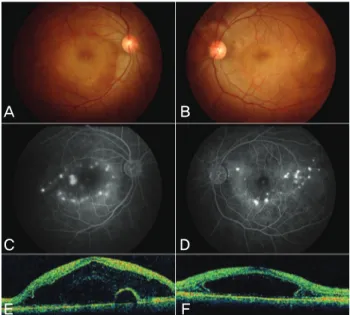
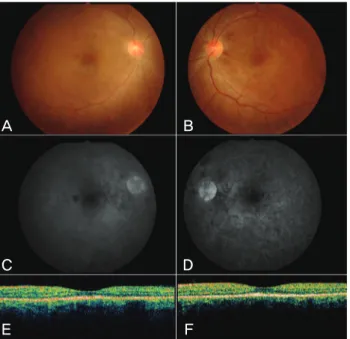
A Case of Vogt-Koyanagi-Harada Disease in a Patient With Graves Disease
Je Hyun Seo, MD
1, Hyeong Gon Yu, MD
1,2,3, Hum Chung, MD
2,31
Department of Ophthalmology, College of Medicine, and Medical Research Center, Seoul National University, Seoul, Korea
2
Institute of Research of Sensory Organs, Medical Research Center, Seoul National University, Seoul, Korea
3