ABSTRACT
Adrenal hemangiomas are a benign tumor of the adrenal gland. These are usually found incidentally on imaging. They are a rare entity of adrenal tumors which have been documenting in the literature in under 100 reports. The diagnosis is routinely made on post-operative histology. We present a case of a 63-year-old male with a right adrenal nodule increasing in size. Computed tomography scan demonstrated a 4.0 cm lesion.
He underwent surgical resection due to its enlargement through a retroperitoneoscopic approach. Pathology examination revealed the diagnosis of an adrenal hemangioma. Adrenal hemangioma is a rare entity of benign adrenal tumors but should be considered in your differential diagnosis of adrenal incidentalomas. The treatment of choice is surgical resection for confirmative diagnosis and to rule out a malignant lesion.
Keywords: Hemangioma; Adrenalectomy
INTRODUCTION
Adrenal hemangiomas are benign tumors of the adrenal gland. It represents 0.01% of adrenal tumors and less than 100 surgical cases have been reported in the literature (1). These benign tumors can be found at any age, however, they have most commonly encountered 40–70 years of age with a female predominance. They are usually identified incidentally on imaging studies. Most commonly they appear as a single adrenal nodule but bilateral hemangiomas have been reported in the literature (2). There have been reports of adrenal hemangioma hemorrhage however that is extremely rare. We present a case of a growing hemangioma diagnosed incidentally.
CASE REPORT
1. Patient
Our patient is a 63-year-old male with a past medical history including chronic obstructive lung disease, chronic pancreatitis and hypertension. He was discovered to have an adrenal incidentaloma on computed tomography (CT) scan for pancreatitis. He was asymptomatic
Short Communication
Received: Sep 17, 2021 Revised: Sep 23, 2021 Accepted: Sep 23, 2021 Correspondence to Kristin McCoy
Carilion Roanoke Memorial Hospital, 3 Riverside Circle, Roanoke, VA 24016, USA.
E-mail: klmccoy4@gmail.com Copyright © 2021. Korean Association of Thyroid and Endocrine Surgeons; KATES This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (https://
creativecommons.org/licenses/by-nc/4.0/).
ORCID iDs Kristin McCoy
https://orcid.org/0000-0001-6449-2751 Katherine Howe
https://orcid.org/0000-0002-3439-0292 Conflict of Interest
No potential conflict of interest relevant to this article was reported.
Author Contributions Conceptualization: Kristin Mccoy;
Investigation: Kristin Mccoy, Katherine Howe;
Methodology: Kristin Mccoy; Supervision:
Daniel Tershak; Writing - original draft: Kristin Mccoy.
Kristin McCoy , Katherine Howe , Daniel Tershak
Carilion Roanoke Memorial Hospital, Roanoke, VA, USA
Laparoscopic Retroperitoneoscopic Removal of an Adrenal Hemangioma:
a Case Report
form this lesion at the time of his presentation. His history was significant for a 20 lbs weight loss over the past 8 months. Biochemical tests were conducting including metanephrines and cortisol were all negative for a functional tumor. His original identification of the adrenal incidentaloma was on CT scan demonstrated right adrenal gland lesion measuring 2.4 cm in 2019. This lesion was followed annually and increased to 3.5 cm × 2.5 cm in 2020 and measuring 4.0 × 2.5 cm in 2021. Pre-contrast measurement of 33 Housefield units (HU), early postcontrast of 36 HU, and delayed postcontrast of 46 HU (Figs. 1 and 2). The lesion was heterogenous and had calcifications (Fig. 1). On physical exam his abdomen was soft without any palpable masses. Based on the rate of growth of this lesion and the substantial weight loss surgical intervention was warranted to rule out a malignant lesion of the adrenal gland.
2. Operative approach: right laparoscopic retroperitoneoscopic adrenalectomy
A 12 mm incision was made at the tip of the 12th rib on the right side. The tissue was spread down to the muscle and a Kelly was used to dissect through into the retroperitoneum. A finger was placed in here and the retroperitoneal space was swept. 2 additional 5 mm ports were placed including one adjacent to the paraspinal muscles. The dissection was started along the paraspinal muscles and went cranially until we encountered the adrenal. The superior attachments of the adrenal were left and at this point we worked along the lateral Fig. 1. Computed tomography scan coronal view demonstrating right adrenal lesion. Arrow depicting lesion.
Peripheral calcifications are visible.
Fig. 2. Computed tomography scan axial view of the right adrenal lesion. Arrow depicts the lesion.
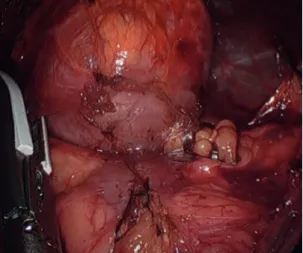
edge and freed the tissue. The kidney was allowed to drop and roll which allowed better exposure of the gland. The attachments were taken along the lateral and inferior edge of the gland using the electrocautery device (Fig. 3). We then dissected along the medial aspect and freed up the feeding adrenal arteries and this allowed the gland to roll more lateral. As we dissected in this area, we came across the inferior vena cava and dissected the gland off of this without any difficulty. The dissection was continued around the entire gland taking the small feeding arteries until everything was detached except for the adrenal vein. The adrenal vein was isolated and at this point it was clipped twice and then transected with the sealing device (Fig. 4). The abdominal pressures were at 25 during the dissection however we did deflate and drop the pressures and found good re-expansion of the inferior vena cava and no significant bleeding seen anywhere.
3. Results
The patient did well post operatively and was discharged on post-operative day 1 with minimal narcotic requirements. The length of the operation was 95 minutes. The patient was seen in follow up clinic at 2 weeks and was recovering well with no complications. The final pathology revealed adrenal hemangioma. 5.5 × 3.5 × 3 cm lesion. Histologic analysis Fig. 3. Intraoperative image of the adrenal tumor sitting on superior pole of kidney.
Fig. 4. Isolation of the adrenal vein.
demonstrated a well circumscribed mass with proliferation consisting of large vascular spaces lined with flattened cells.
DISCUSSION
Adrenal hemangiomas are a rarity. As with our patient these tumors are usually nonfunctional.
Adrenal incidentalomas are found on around 0.4% of CT scans (2-4). An incidentaloma is defined as a lesion of the adrenal gland that is >1 cm and found on imaging performed for other means, The incidence of an adrenal carcinoma in patients with an adrenal incidentaloma is 2%–5% (5).
Therefore, surgical intervention is appropriate and remains the gold standard of treatment.
Adrenal hemangiomas can be difficult to diagnose preoperatively as their imaging can be indeterminate and unable to be differentiated from an adenoma or a malignancy. If the hemangioma has the classic appearance consisting of a peripheral patchy enhancement and a highly dense rim of peripheral tissue a CT or magnetic resonance imaging is useful the diagnosis. The larger masses frequently have areas of calcification representing areas of previous hemorrhage however this is not pathognomic for hemangiomas (2). Therefore, surgical intervention is appropriate and remains the gold standard of treatment and in most cases the final diagnosis is made by histopathology after surgical resection.
The algorithm to treatment of an adrenal mass discovered incidentally takes into account tumor size, its secreting character or not and imaging data suggestive of malignancy.
Resection of adrenal incidentalomas are indicated if tumors are functional regardless of the size, in tumors >4 cm even if nonfunctional, when there is an increase in size of the adrenal lesions during a 4 year follow up, or if preoperative imaging demonstrates any factors to suggest a malignant lesion (6). These factors would include irregular margin of the tumor on imaging, surrounding tumor invasion, nonuniform enhancement of the lesion, >10 HU on non-contrast CT scan, or low contrast washout rate is low in the delayed view of a contrast CT scan 4. Other indications for surgery include mass-effect type symptoms from neighboring organs causing compressive symptoms, or adrenal rupture (6). In our case there was a high suspicion for malignancy due the increase in size of the tumor, heterogenous features with calcification on imaging, and clinical picture of weight loss.
Surgical approach depends on the size and features of the tumor. The approach can be laparoscopic transabdominally, retroperitoneoscopic, or a laparotomy. The laparoscopic transabdominal approach is an anterior approach with the patient in the lateral position.
The retroperitoneoscopic approach is a laparoscopic approach through the patient back into the retroperitoneal space. A laparotomy is typically though a midline incision if necessary.
In our case the tumor was 4.0 cm on preoperative imaging, taking into account the patients small body habitus and history of surgical procedures done through the anterior abdomen, a retroperitoneoscopic approach was pursued.
In conclusion, adrenal hemangioma is a rare entity of benign adrenal tumors. This diagnosis is hard to establish in the preoperative setting but should be included in differential diagnosis of adrenal neoplasms. The treatment of choice is surgical resection for confirmative
diagnosis and to rule out a malignant lesion. Laparoscopic retroperitoneal resection is in option in these benign tumor entities. Patient comorbidities should be taken into account to create a surgical plan.
REFERENCES
1. Johnson CC, Jeppesen FB. Hemangioma of the adrenal. J Urol 1955;74:573-7.
PUBMED | CROSSREF
2. Otal P, Escourrou G, Mazerolles C, Janne d'Othee B, Mezghani S, Musso S, et al. Imaging features of uncommon adrenal masses with histopathologic correlation. Radiographics 1999;19:569-81.
PUBMED | CROSSREF
3. Feo CV, De Troia A, Pedriali M, Sala S, Zatelli MC, Carcoforo P, et al. Adrenal cavernous hemangioma: a case report. BMC Surg 2018;18:103.
PUBMED | CROSSREF
4. Zemni I, Haddad S, Hlali A, Manai MH, Essoussi M. Adrenal gland hemangioma: a rare case of the incidentaloma: case report. Int J Surg Case Rep 2017;41:417-22.
PUBMED | CROSSREF
5. Young WF Jr. Clinical practice. The incidentally discovered adrenal mass. N Engl J Med 2007;356:601-10.
PUBMED | CROSSREF
6. Lee JM, Kim MK, Ko SH, Koh JM, Kim BY, Kim SW, et al. Clinical guidelines for the management of adrenal incidentaloma. Endocrinol Metab (Seoul) 2017;32:200-18.
PUBMED | CROSSREF