Thoracic involvement is more common in systemic lu- pus erythematosus (SLE) than in any other connective tissue diseases (1, 2), and more than half of all patients with the disease suffer from respiratory dysfunction during the course of their illness (2-5). Respiratory dis- ease may be due to direct involvement of the lung or as a secondary consequence of the effect of SLE on other organ systems. This pictorial essay will review the radi- ographic and CT findings of various pulmonary mani- festations of SLE, including secondary pulmonary mani- festations.
Primary Involvement of the Respiratory System
Acute lupus pneumonitis
Acute lupus pneumonitis is an abrupt febrile pneu- monic process mostly without infectious etiology, and antibiotics usually fail to favorably alter its course. A fa-
vorable response to corticosteroid, with normalization of the clinical and radiological manifestations, can be help- ful in establishing its diagnosis. The histopathologic findings are not diagnostic or pathognomonic (1, 2), but include alveolar wall damage and necrosis, inflammato- ry infiltrates, hemorrhage, edema, and hyaline mem- brane. The radiologic findings consist of patchy unilater- al or bilateral areas of ground glass opacity or air space consolidation, involving mainly lung bases (2) (Figs. 1, 2), features which may be indistinguishable from those of a pneumonic process caused by bacterial and nonbac- terial opportunistic infection, or of thromboembolic dis- ease. Because infection is common, particularly in pa- tients undergoing corticosteroid or immunosuppressive therapy, differentiation between these causes is critical (2).
Pulmonary hemorrhage
Pulmonary hemorrhage in SLE, the pathogenesis of which is unknown, varies from a mild, subclinical, chronic form to acute, massive, life-threatening bleed- ing. Some of its cardinal features, such as hemoptysis and hypoxemia, may be lacking even where hemor- rhage is severe. In patients with hemoptysis, two find-
Pulmonary Manifestations of Systemic Lupus Erythematosus
1Kee Hyuk Yang, M.D., Yo Won Choi, M.D., Seok Chol Jeon, M.D., Choong Ki Park, M.D., Kyung Bin Joo, M.D., Chang Kok Hahm, M.D., Seung Ro Lee, M.D.
Pulmonary involvement is more common in systemic lupus erythematosus (SLE) than in any other connective tissue disease, and more than half of patients with SLE suffer from respiratory dysfunction during the course of their illness. Although sepsis and renal disease are the most common causes of death in SLE, lung disease is the pre- dominant manifestation and is an indicator of overall prognosis. Respiratory disease may be due to direct involvement of the lung or as a secondary consequence of the ef- fect of the disease on other organ systems.
Index words :Lung, diseases Lupus erythematosus
1Department of Radiology, Hanyang University Seoul Hospital Received April 2, 2003 ; Accepted October 6, 2003
Address reprint requests to : Yo Won Choi, M.D., Department of Radiology, Hanyang University Hospital, 17 Haengdang-dong, Sungdong- gu, Seoul 133-792, Korea.
Tel. 82-2-2290-9161 Fax. 82-2-2293-2111 E-mail: ywchoi@hanyang.ac.kr
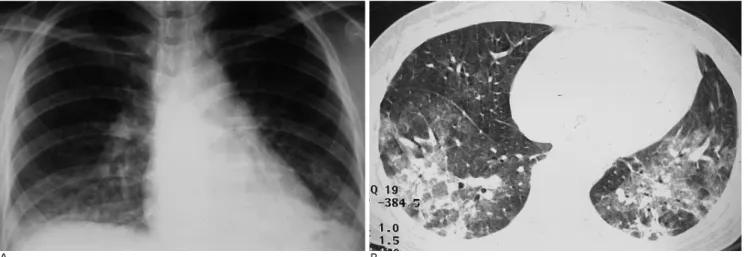
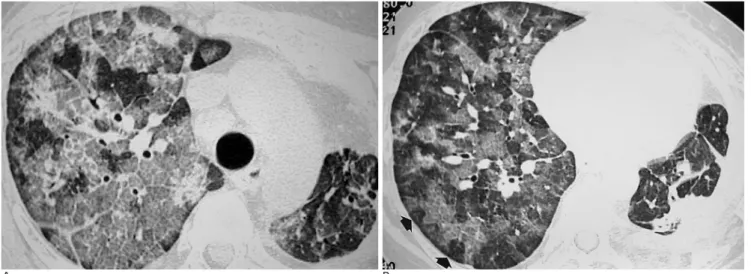
A B Fig. 1. Acute lupus pneumonitis in a 46-year-old woman with SLE.
She was presented with abrupt onset of dyspnea and fever, but laboratory data showed no evidence suggestive of infectious origin.
A. Frontal chest radiograph shows ill-defined hazy opacities in both lower lungs.
B. Thin-section CT at the level of basal lung shows areas of nodular consolidation and ground-glass attenuation in both lower lobes.
After steroid pulse therapy for 2 weeks, most lung lesions resolved (not shown).
A
C
B
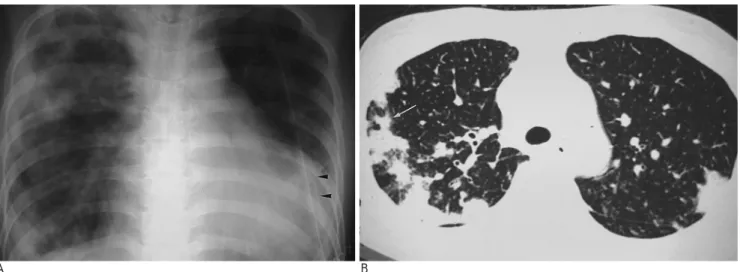
Fig. 2. Acute lupus pneumonitis in a 21-year-old woman with SLE.
A. Frontal chest radiograph shows focal air-space consolidation in the left upper lung.
B. CT scan at the level of the aortic arch shows air-space consoli- dation and multiple, ill-defined nodular opacities. Laboratory studies, including biopsy of the lung, did not reveal any infec- tious organism at this time.
C. Thin-section CT at the level similar to B, obtained after steroid medication for 1 month, shows improvement of the con- solidation but newly developed lung cysts or airway dilatation (arrows).
ings may suggest significant pulmonary hemorrhage: a marked drop in hematocrit over a period of 12 to 36 hours, and an otherwise unexplained increase in the dif- fusive capacity of carbon monoxide, or DLCO (2). Chest radiography depicts areas of ill-defined, patchy, acinar opacity that are usually bilateral and located in the low- er lung zones (Fig. 3). With the cessation of hemoptysis, the findings of radiography improve rapidly and often normalize within 2-4 days (2). CT demonstrates ground-glass opacity and, sometimes, frank consolida- tion. A nodular pattern with no zonal predominance or bronchocentricity may be also seen, especially during complete or partial clinical remission (3).
Bronchiolitis obliterans organizing pneumonia
Bronchiolitis obliterans organizing pneumonia (BOOP) is a pathologic entity characterized by the formation of plugs of fibrous tissue in bronchioles and alveolar ducts.
Most cases are idiopathic, but a BOOP-like reaction has been described in association with several connective
Fig. 3. Pulmonary hemorrhage in a 33-year-old woman with SLE.
She was presented with abrupt onset of fever, dyspnea, and anemia. Frontal chest radiograph shows air space consolida- tion in parahilar and lower lung field bilaterally. The patient revealed increased diffusing capacity for carbon monoxide, or DLCO, and hemosiderin-laden macrophages in bron- choalveloar lavage, confirming the diagnosis.
A
C
B
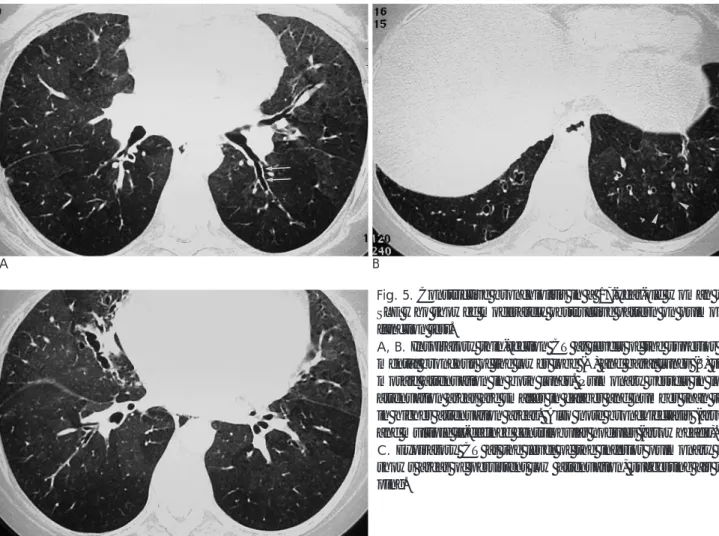
Fig. 4. Bronchiolitis obliterans organizing pneumonia in a 24- year-old woman with SLE and lupus cardiac disease.
A. Frontal chest radiograph shows cardiomegaly, bilateral pleur- al effusion, and peripheral patchy increased opacities, predomi- nantly in the right lung. Also note a chest tube (arrowheads) in the left pleural space which was inserted to drain pleural effu- sion. BOOP was confirmed by gun biopsy. Frontal chest radi- ograph became normalized after steroid pulse therapy for one month (not shown).
B, C. Thin-section CT scans at levels of the aortic arch (B) and basal lungs (C) at the same time as A show nodules (arrow) and consolidations predominantly in the peripheral lung.
Interlobular septal thickening and dilated pulmonary veins (ar- rowhead) indicate pulmonary congestion associated with lupus cardiac disease.
tissue diseases including SLE. The prognosis is generally excellent. Bronchiolitis obliterans organizing pneumonia typically manifests with scattered, bilateral ground-glass attenuation or air space consolidation. All lung zones are equally affected (1, 2). Distinct subpleural and/or peri- bronchial distribution may be seen in 50-60% of cases (Fig. 4), and discrete centrilobular nodules may be asso- ciated.
Constrictive bronchiolitis (obliterative bronchiolitis) At lung function testing, constrictive bronchiolitis is characterized by airflow obstruction due to submucosal and peribronchiolar inflammation and fibrosis, which primarily involves respiratory bronchioles, and the ab- sence of diffuse parenchymal inflammation. Chest radi- ography usually reveals no parenchymal abnormality.
The most obvious thin-section CT findings are focal, of- ten sharply defined, areas of decreased lung attenuation associated with vessels of decreased caliber in the ab- sence of parenchymal consolidation; bronchiectasis, mainly at a subsegmental level, may also be noted (Figs.
5, 6). In addition, expiratory CT shows focal areas of air trapping consistent with small airway obstruction. In rare cases, areas of opacity, either centrilobular branch- ing or ill-defined centrilobular, may be a predominant finding (Fig. 5).
Chronic interstitial pneumonitis and fibrosis
The prevalence of clinically significant interstitial lung disease in SLE has been reported in as few as 1-6% of patients. However, with the use of thin-section CT, the detection rate of early, SLE-associated, interstitial dis- ease is increasing (1, 4). Although the disease which complicate SLE resemble those of idiopathic pulmonary fibrosis, including both usual and nonspecific interstitial pneumonitis, both pathologically and radiologically, its course is usually less severe from clinical and functional points of view. The radiographic findings include bibasi- lar areas of irregular linear opacity, ground-glass attenu- ation, and loss of lung volume (Fig. 7). The typical CT appearance includes interlobular and intralobular inter- stitial thickening, areas of ground-glass attenuation, and
A
C
B
Fig. 5. Constrictive bronchiolitis in a 17-year-old woman with SLE who showed moderately obstructive pattern on pulmonary function test.
A, B. Inspiratory thin-section CT at levels of the superior seg- mental bronchus of the lower lobe (A) and basal lungs (B) show mosaic attenuation in both lungs. Pulmonary vessels in lower attenuation areas are smaller in caliber and number than those in higher attenuation areas. Also note bronchiectasis (arrows) and multiple ill-defined centrilobular nodules (arrowheads).
C. Expiratory CT at the level of the inferior pulmonary vein shows areas of persistent low attenuation, suggesting air trap- ping.
traction bronchiectasis with predominantly subpleural and basal involvement (1, 4) (Fig. 7). End-stage disease is accompanied by honeycombing, traction bronchiecta- sis, and achitectual distortion, as in the case of usual in- terstitial pneumonitis (Fig. 7). Mild enlargement of the mediastinal lymph nodes is common.
Pulmonary vascular disease
Pulmonary vascular involvement in SLE may include the capillary, arterial, and venous systems. Venous in- volvement, however, is radiographically distinct from pulmonary hypertension caused by arterial involve-
ment.
Pulmonary arterial hypertension
In approximately 10% of SLE patients, clinically evi- dent pulmonary arterial hypertension is present (2, 3).
The potential mechanisms of the condition include in- terstitial pneumonitis, small pulmonary arterial vasculi- tis, thrombosis in situ or pulmonary thromboembolism, and primary pulmonary hypertension (2). Vascular ab- normalities typically afflict small muscular arteries (2).
During the early phase, chest radiographic findings may be normal, but advanced radiographic findings include
A B
Fig. 6. Constrictive bronchiolitis in a 21-year-old woman with SLE who showed severely obstructive pattern on pulmonary func- tion test.
A. Inspiratory thin-section CT at the level of basal lungs shows focal, relatively well defined normal areas of increased attenuation (arrows) interspersed with radiolucent areas indicative of air trapping. Also, note bronchial dilatation.
B. Expiratory thin-section CT at the same level as A show marked air trapping.
A B
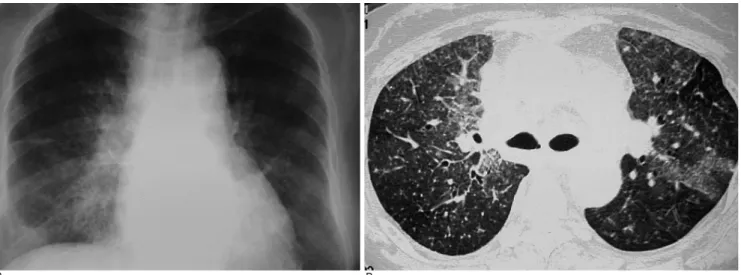
Fig. 7. Chronic interstitial lung disease in a 22-year-old woman with SLE.
A. Frontal chest radiograph shows ill-defined reticular opacity in the left lower lung.
B. Thin-section CT at the level of basal lungs shows interlobular and intralobular septal thickening and patchy ground-glass attenu- ation.
enlargement of the right ventricle, and prominent main pulmonary artery with distal attenuation of the arteries (3) (Fig. 8). Ventilation/perfusion scanning or pulmonary angiography can help exclude pulmonary embolism.
Pulmonary veno-occlusive disease
Pulmonary veno-occlusive disease is a rare form of pulmonary hypertension characterized pathologically by repeated pulmonary venous thrombosis, and clinical- ly by pulmonary arterial hypertension and edema. The
disorder has been reported in association with a variety of autoimmune diseases. Radiographically, pulmonary veno-occlusive disease shows signs of pulmonary arteri- al hypertension very similar to those associated with pri- mary pulmonary arterial hypertension or thromboem- bolic disease, but includes an important additional sign of pulmonary edema. The most common CT findings in- clude smooth interlobular thickening and areas of ground-glass attenuation consistent with interstitial pul- monary edema, enlarged central pulmonary arteries,
A B
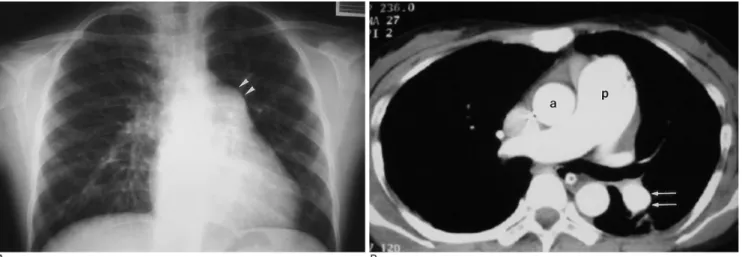
Fig. 8. Pulmonary arterial hypertension in a 16-year-old woman with SLE.
A. Frontal chest radiograph shows typical features of pulmonary arterial hypertension, including bulging of the pulmonary conus (arrowheads) and prominent proximal pulmonary arteries.
B. Thin-section CT obtained before contrast administration show the enlarged pulmonary trunk (p), which is larger in diameter than the ascending aorta (a). Also note enlarged left pulmonary arteries (arrows).
A B
Fig. 9. Pulmonary veno-occlusive disease in a 14-year-old woman with SLE. Echocardiography showed right ventricular enlarge- ment, mild tricuspid valvular regurgitation, and normal global systolic function. Cardiac catheterization revealed normal pul- monary capillary wedge pressure. These features clinically confirmed the diagnosis of pulmonary veno-occlusive disease.
A. Frontal chest radiograph shows prominent hilar shadows and diffuse haziness in both lower lungs. Also note left pleural effu- sion (arrow).
B. Thin-section CT at the level of basal lungs shows thickening of interlobular septa (long arrow) and bronchial wall, and focal con- solidations (short arrows).
and pulmonary veins of normal caliber (Fig. 9). A mosa- ic pattern of lung attenuation, as well as pleural effu- sion, is frequently present.
Secondary Involvement of the Respiratory System
Severe multi-organ diseases often confound the clini- cal status of patients with SLE, treatment for such dis- ease, and its attendant complications. Renal failure, cen- tral nervous system involvement, or cardiac involve- ment may lead to pulmonary edema (Fig. 10). In addi- tion, pericardial effusion, neuromuscular disease, and diaphragmatic dysfunction can affect the respiratory system, resulting in passive atelectasis, for example, and oxygen therapy or cytotoxic chemotherapy may cause pulmonary toxicity. Infection, however, is the most im- portant cause of indirect involvement of the lungs in SLE (2).
Pulmonary infection other than tuberculosis in SLE Pulmonary infection is a major cause of morbidity and mortality in SLE, with either common bacterial agents or more unusual opportunistic organisms causing pul- monary infections. Opportunistic infections in SLE pa- tients include aspergillosis, cryptococcosis, pneumocys- tis carinii (Fig. 11), cytomegalovirus, and nocardia.
Though the exact impact of early diagnosis of oppor- tunistic infection is difficult to predict, clearly some
such infections, including Pneumocystis carinii, Candida albicans, and Nocardia, may be treatable.
Uncommon clinical and radiographic abnormalities may, however, accompany common bacterial infec- tions. The risk of infection in the absence of immuno- suppression is small, though an aggressive diagnostic ap- proach to exclude infection in any patient with SLE pre- senting with new pulmonary infiltrates is warranted, particularly if immunosuppressive therapy is ongoing.
A B
Fig. 11. Pneumocystis carinii pneumonia in a 33-year-old woman with SLE who had been taking pulse therapy with corticosteroid and cyclosporin for a month.
A, B. Thin-section CT scans at levels of the aortic arch (A) and basal lungs (B) show mosaic pattern of ground-glass opacities ad- mixed with intra- and interlobular septal thickening, namely crazy-paving appearance. Also note clear sparing of isolated sec- ondary lobules (arrows). Left lung shows fibrosis and marked volume contraction secondary to longstanding tuberculosis. The or- ganism was isolated from bronchoalveolar lavage fluid.
Fig. 10. Pulmonary edema in a 34-year-old woman with SLE.
Thin-section CT at the level of the diaphragm shows typical features of pulmonary edema, including dilated pulmonary vessels (arrow), smooth thickening of the interlobular septa (arrowheads), and areas of ground-glass attenuation.
Pulmonary Tuberculosis in SLE
Pulmonary tuberculosis in patients with SLE may manifest differently than in immunocompetent patients, and because of the abnormal functioning of alveolar macrophages and exposure to corticosteroid and cy- totoxic drugs, the incidence in the former may be higher (5). Delayed diagnosis may contribute to a higher inci- dence of miliary, far-advanced, and extrapulmonary tu- berculosis. In patients with SLE who are taking steroids, the radiologic findings can be similar to those seen in secondary tuberculosis, such as areas of apical nodular opacity (Fig. 12), or in primary tuberculosis, such as large air-space consolidation, lymphadenitis, pleural ef-
fusion, or miliary tuberculosis (Fig. 13) (5). Thin-section CT findings of miliary tuberculosis resemble those de- scribed in that previous report: miliary nodules associat- ed with interlobular septal thickening, intralobular retic- ulation, ground-glass attenuation, and pleural effusion (Fig. 13).
Conclusion
Because pulmonary disease is the predominant mani- festation of the illness and a primary indicator of overall prognosis, an understanding of the various radiographic and CT findings of pulmonary involvement in SLE per-
A B
Fig. 12. Pulmonary tuberculosis in a 26-year-old man who had been taking steroid medication for SLE for one year.
A. Magnified frontal chest radiograph shows poorly-defined nodular and linear opacities in both upper lungs.
B. Magnified thin-section CT showing the right lung apex reveals centrilobular nodular and branching opacities (arrowheads) in the right upper lobe.
A B
Fig. 13. Miliary tuberculosis in a 58-year-old woman who had been taking steroid therapy for SLE for 6 months.
A. Plain chest radiograph obtained at admission shows innumerous tiny nodular shadows in the entire lung.
B. Thin-section CT at the level of the carina shows miliary nodules of random distribution and areas of ground-glass attenuation.
mits appropriate patient management.
References
1. Bankier AA, Kiener HP, Wiesmayr MN, et al. Discrete lung in- volvement in systemic lupus erythematosus: CT assessment.
Radiology 1995;196:835-840
2. Wiedemann HP, Matthay RA. Pulmonary manifestations of sys- temic lupus erythematosus. J Thorac Imaging 1992;7:1-18
3. Kim JS, Lee KS, Koh EM, Kim SY, Chung MP, Han J. Thoracic in- volvement of systemic lupus erythematosus: clinical, pathologic, and radiologic findings. J Comput Assist Tomogr 2000;24:9-18 4. Fenlon HM, Doran M, Sant SM, Breatnach E. High-resolution
chest CT in a systemic lupus erythematosus. AJR Am J Roentgenol 1996;166:301-307
5. Kim HY, Im JG, Goo JM, Lee JK, Song JW, Kim SK. Pulmonary tu- berculosis in patients with systemic lupus erythematosus. AJR Am J Roentgenol 1999;173:1639-1642
대한방사선의학회지 2004;50:37-45
전신홍반성루푸스의 폐병발 소견1
1한양대학병원 진단방사선과
양기혁・최요원・전석철・박충기・주경빈・함창곡・이승로
전신홍반성루푸스(systemic lupus erythematosus)는 다른 어느 교원조직질환보다도 폐 병발이 흔하며 전신홍반성 루푸스 환자의 반 이상이 질환 경과 중에 호흡기 장애를 호소한다. 전신홍반성루푸스에서 폐혈증과 신장 질환이 가장 흔한 사망 원인이지만 폐 질환이 주된 병변을 이루며 전체 예후의 지표가 된다. 폐 질환은 폐에 직접적 병발을 하는 루 푸스 폐렴, 폐출혈, 폐색성 기관지염, 간질성 섬유화, 폐혈관성 질환 등이 포함되고, 다른 기관의 질환으로 인한 이차적 병변과 감염 등의 간접적 병변들이 포함된다.