757 J. of Korean Orthop. Assoc. 2003; 38: 757-62
목 적 : 본 연구의 목적은 고주파 에너지가 사람의 연골 세포에 미치는 영향을 관찰하고 공초점 레이저 현미경 소견과 연골의 방사성 동위원소 부착 황산 염의 흡수 정도, 그리고 조직학적 소견의 연관관계를 연구하여 임상적 이용에 유용한 지침을 정하는데 있다.
대상 및 방법 : 인공관절성형술을 받은 환자에게서 얻은 관절연골 표면에 3.0 mm의 ArthroWand를 이용하여 연골 성형술을 시행하였다. ArthroWand를 초 당 10 mm의 속도로 움직이면서 연골 표면에 접촉한 상태와 접촉하지 않을 상태로 각각 3가지 출력 강도의 고주파 에너지를 사용하여 시술하였다. 시술 후 연골세포의 생사 여부는 confocal laser microscopy와 연골세포 대사의 표식자로 연골 조직의35S 흡수 정도를 분석하였다.
결 과 : 공초점 레이저 현미경에 의한 검사에서는 시술 방법에 상관없이 관절 연골의 부분적인 연골세포 손상을 보였고, 고주파 에너지에 의하여 연골 전층 에 이르는 연골 세포 파괴는 없었다. ArthroWand를 접촉한 상태에서의 시술에 의해서는 에너지 출력의 강도와 시술 횟수에 비례하여 조직의 제거 정도는 증가하였다. 방사선 동위원소 부착 황산염의 흡수 정도는 시술 방법과 에너지 출력의 강도와는 상관없이 유의한 차이를 보이지는 않았다.
결 론 : 고주파 에너지에 의한 관절 연골의 연골세포의 손상의 정도는 에너지 방출 기기의 속도를 10 mm/sec 이상으로 했을 때, 이전에 보고된 것처럼 그 렇게 심각하지는 않았다. 기기의 비접촉 상태에서의 시술은 연골조직의 제거에 효과적이지는 않았으나, 고주파 에너지는 연골 표면에 직접 접촉 상태로 적 당한 출력 강도와 시간동안 가하였을 때 손상된 연골 조직을 제거하는데 유용할 것으로 사료된다.
색인 단어 : 관절 연골, 연골 성형술, 고주파 에너지, 공초점 레이저 현미경
757
고주파 에너지(Radiofrequency energy)가 사람의 관절연골에 미치는 영향
- 에너지 강도와 치료 방법이 연골세포의 사활에 미치는 영향에 대하여 -
고승희∙김기수∙최용수∙정영률∙송준영∙박봉희∙최진배∙김대중∙김윤식*∙이재혁�
광주기독병원 정형외과, 광주기독병원 체외수정실*, 전남대학교 의과대학 병리학교실�
Mechanical, chemical and microbiological factors may dam- age cartilage, resulting in fibrillation, fragmentation and de-
lamination of the articulating surface. Partial thickness carti- lage defects have been treated by shaving of the loose super-
757 757 통신저자 : 고 승 희
광주광역시 남구 양림동 264 광주기독병원 정형외과
TEL: 062-650-5064∙FAX: 062-650-5066 E-mail: oskosh@hanmail.net
The Effects of Radiofrequency Energy on Human Articular Cartilage - The Effect of Power Setting and Mode of Treatment on Chondrocyte Viability -
Seung-Hee Ko, M.D., Kee-Soo Kim, M.D., Yong-Soo Choi, M.D., Young-Youl Chung, M.D., June-Young Song, M.D., Bong-Hee Park, M.D., Jin-Bae Choi, M.D., Dae-Joong Kim, M.D., Yoon-Sik Kim, M.T.*, and Jae-Hyuk Lee, M.D.�
Department of Orthopaedic Surgery, Gwangju Christian Hospital, Gwangju; In-Vitro Fertility Room*, Gwangju Christian Hospital, Gwangju;
Department of Pathology�, Chonnam National University, Gwangju, Korea
Purpose:The objective of this study was to investigate the effects of radiofrequency energy on human chondrocyte viability, and to cor- relate confocal laser microscopy fluorescence to sulfate uptake and to the histological integrity of articular cartilage.
Materials and Methods:The chondroplasty procedure for chondromalacic articular cartilage was performed using a 3.0-mm ArthroWand (Arthroscopic Electrosurgery System, ArthroCare Corporation) on fresh human articular cartilage. Radiofrequency energy was applied to the cartilage surface through the probe at a velocity of 10-mm per second in contact and non-contact mode. Three power settings were used. The treated cartilage was analyzed for chondrocyte viability by confocal laser microscopy and 35S uptake.
Results: Confocal laser microscopy demonstrated partial-thickness chondrocyte death irrespective of treatment method. No mode of treatment or radiofrequency energy power setting resulted in full-thickness chondrocyte death. The depth of cartilage ablation was increased in the treated areas in contact mode in proportion to the power level and the time of treatment. No statistically significant difference in radiolabeled sulfate uptake of the specimens was observed with respect to the treatment modes and power settings.
Conclusion:The extent of chondrocyte death by radiofrequency energy was not as significant as reported previously when the probe was moved at the speed of 10 mm/sec. Radiofrequency energy may be useful to treat chondromalacic cartilage in a contact mode using a proper energy level and delivery time.
Key Words: Articular cartilage, Chondroplasty, Radiofrequency energy, Confocal laser microscopy
Address reprint requests to Seung-Hee Ko, M.D.
Department of Orthopaedic Surgery, Gwangju Christian Hospital 264 Yanglim-dong, Nam-gu, Gwangju 503-040, Korea Tel: +82.62-650-5064, Fax: +82.62-650-5066 E-mail: oskosh@hanmail.net
ficial fragments using a mechanical rotating device5,6,10,16). The limitation of this treatment is the inability to obtain a smooth and stable articulating surface5,15). Electrosurgical probes using radiofrequency energy have been developed for arthroscopic cartilage and synovium ablation and shrinkage as an alterna- tive to mechanical shavers3,4,6,11,14). However, the effects of ra- diofrequency energy on chondrocyte viability vary with meth- ods of its use and assessment6-8). The objectives of this study are 1) to investigate the effects of radiofrequency energy on human chondrocyte viability and to correlate confocal laser microscopy fluorescence to sulfate uptake and 2) to determine the appropriate method of radiofrequency energy treatment.
MATERIALS AND METHODS
Fresh human articular cartilage was obtained from discarded bones of fifteen patients who had undergone total knee arthro- plasty for degenerative osteoarthritis. The osteochondral pieces that were taken from distal resections of the lateral femoral condyle were trimmed as large as possible to rectangular shape.
All the specimens used in this study fell within Outerbridge grade 2.
The chondroplasty procedure for chondromalacic articular cartilage was performed using an ArthroCare 2000 bipolar radiofrequency energy system (ArthroCare, Sunnyvale, CA) with 3.0 mm ArthroWand (#A1330, ArthroCare). The cus- tom-made jig was applied on the prepared specimen to make a consistent treatment area along a marked line. To determine the effects of distance from electrosurgical probe tip to carti- lage surface and voltage output, the radiofrequency energy was delivered 1mm above the articular cartilage surface (group 1; non-contact mode, single pass) at one of three power set- tings: S1 [90-110 kHz per Vrms (voltage root mean square)], S3 [135-165 kHz per Vrms], S5 [180-220 kHz per Vrms].
The radiofrequency energy treatment was performed on the specimen in contact with the electrosurgical probe at the same voltage levels (group 2; contact mode, single pass). The same procedure was repeated at the treated site to compare the ther- mal effect of repeated application of radiofrequency energy (group 3; contact mode, double pass) simulating the clinical situation. The probe was moved at a consistent speed of 10 mm/sec. There were total nine different treatment subgroups in this study, and five specimens were made for each subgroup.
Following the procedure, an osteochondral section 1.0 mm thick was cut at the mid-portion of the treated area for con- focal laser microscopy. Two chondral cubes about 2 mm in dimension were obtained from other treated area for assess-
ment of 35S uptake.
1. Confocal laser microscopy
Viability of chondrocytes can be determined by their ability to exclude fluorescent dyes12). The cell membranes of dead or damaged cells were penetrated by ethidium homodimer to stain their nuclei red. Living cells with intact plasma mem- branes and active cytoplasm metabolize calcein and show green fluorescence. Osteochondral sections, 1.0-mm thick, were incu- bated for 30 minutes at room temperature in a 2 M calcein- AM (acetoxyethylester) and 4 M ethidium homodimer-1 solution (Live/Dead Viability/Cytotoxicity Kit [L-3224], Mo- lecular Probes, Eugene, OR). The location of viable and non- viable cells was determined by the difference in their ability to exclude fluorescent dyes using the confocal laser microscope equipped with an argon laser and the necessary filter systems.
2. Radiolabled sulfate uptake
Exposing live cartilage to media containing radioactive 35S can be used as an index of sulfated proteoglycan synthesis and chonrocyte viability2,13). 35S-sulfate uptake has been used to showed differences in viability and metabolism rate in carti- lage of varying origins and disease states1,2).
Two groups, group 1 and 2, were involved in this procedure.
Ten cartilage samples of each radiofrequency energy treatment group were used for assessment of radiolabed sulfate uptake.
The untreated and frozen cartilage samples were included as controls. Each cartilage tissue sample was pre-incubated in 0.5 mL of serum-free Dulbecco’s modified medium (DMEM) for 30 minutes at 37℃in a humid CO2incubator. The medi- um was removed and 0.25 mL of 35S media (20 Ci/mL) was added to the tube and the cartilage was incubated for 4 hours at 37℃and 7.0% CO2. Media containing 35S was then re- moved and the cartilage was washed with 0.5 mL of phosphate buffered saline (pH 6) twice. Following wash 0.5 mL PBS containing 5 mM EDTA, 5 mM Cysteine and 0.25 mg/mL papain was added and the vial was placed in a 65℃water bath for 18 hours or until the cartilage dissolved completely. After digestion by papain the sample was precipitated three times with 1 mL of 100% ethyl alcohol. Following the last precipi- tation Ethyl alcohol was removed and the sample was re-sus- pended in 0.5 mL of PBS. The sample was removed from the vials and transferred to scintillation vials, and 10 mL of scin- tillation fluid was added to the vials. The amount of incorpo- rated35S was quantified as counts per minute (cpm) by a liquid scintillation counter (Packard, Pale Alto, CA).
Statistical analysis was performed using multiple compar- isons (Tukey HSD in SAS package), and the Kruskal-Wallis test was used to compare the results according to type of treat- ment and level of power with significance set at the p<0.05
(SPSS 10.0 for windows).
RESULTS
Gross inspection of the treated cartilage showed light dis- coloration without visible tissue ablation in the areas of non- contact treatment. The cartilage that was treated with contact mode and power level S3 and S5 showed apparent tissue abla- tion on the surface. Microscopically, the chondrocytes at the site of treatment looked viable without alteration of its nuclei, cytoplasm and lacunae.
The depth of chondrocyte death and cartilaginous tissue ablation was measured with the confocal laser microscope after calibration of the microscopic field (Table 1, Fig. 1, 2). Any mode of treatment or power setting of radiofrequency energy did not result in full-thickness chondrocyte death. The degree of chondrocyte death, however, was variable according to the
Treatment mode Depth of chondro- cyte death
Depth of tissue ablation
Non-contact, S1 0.112 0
Non-contact, S3 0.114 0.026
Non-contact, S5 0.122 0.032
Contact, S1 0.864 0.042
Contact, S3 0.298 0.218
Contact, S5 0.274 0.358
Contact, S1, double passes 0.836 0.120 Contact, S3, double passes 0.256 0.364 Contact, S5, double passes 0.278 0.722 Table 1.Depth of chondrocyte death and cartilaginous tissue ablation measured by confocal laser microscopy (converted to mm)
Non-contact Contact, Contact, single pass double pass 0.8
0.7 0.6 0.5 0.4 0.3 0.2 0.1 0
Fig. 2.Depth of tissue ablation (mm). The amount of tissue ablated increased in proportion of the power level and the frequency of treatment.
Power S1 Power S3 Power S5
Non-contact Contact, Contact, single pass double pass 0.9
0.8 0.7 0.6 0.5 0.4 0.3 0.2 0.1 0
Fig. 1.Depth of chondrocyte death (mm). Thermal penetration was significantly higher in contact mode at power level 1 (S1).
Power S1 Power S3 Power S5
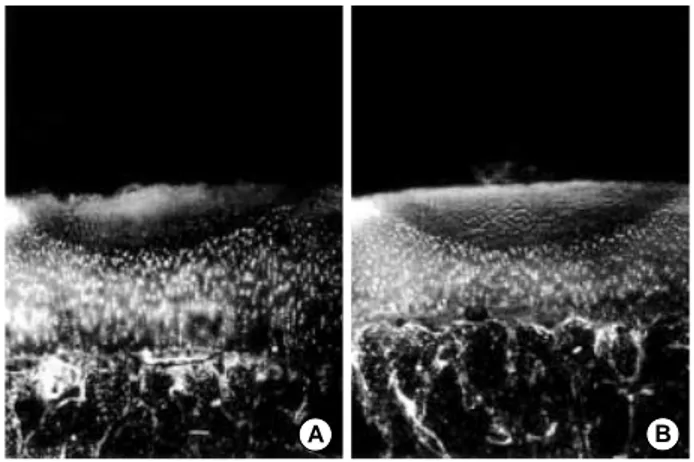
Fig. 3.Confocal microscopic images demonstrating negligable chondrocyte death or tissue ablation at the treated area in the non- contact mode at power setting S1 (A) and S5 (B) (calcein-AM/ethidi- um homodimer-1 stain, ×20).
A B
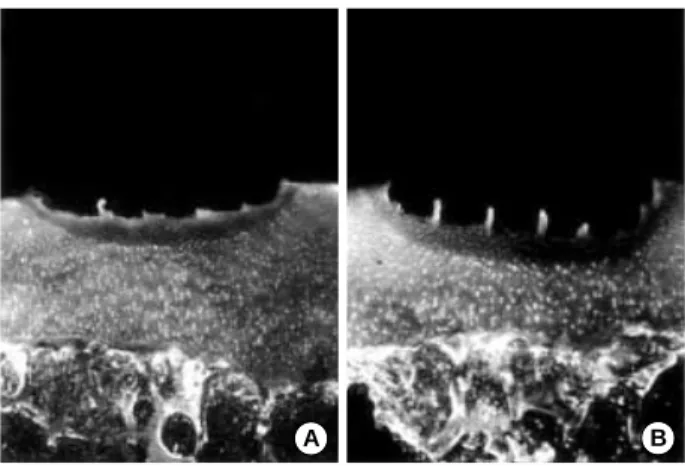
Fig. 4.Confocal microscopic images showing thermal damage to the cartilage by the contact mode and power setting S1 (calcein- AM/ethidium homodimer-1 stain, ×20): (A) single pass, (B) double pass.
A B
treatment mode and power level. The depth of tissue ablation and chondrocyte death was negligible in the group of non- contact mode of treatment at all power levels (Fig. 3). The contact mode of treatment with power level S1 caused signif- icantly deeper chondrocyte injury than same mode with higher power levels (S3, S5), but the amount of cartilaginous tissue ablation was minimal (p<0.05, Fig. 4). Repeated passage of the wand did not double the thermal effect of the radiofrequen- cy energy. The depth of cartilage ablation was increased in the contact treated areas in proportion to the power level at S3 and S5 and the frequency of treatment (Fig. 5, 6).
There was no statistically significant difference in radiola- beled sulfate uptake of the specimens according to the treat- ment mode and power setting (Table 2). The preserved frozen cartilage was significantly lower in scintillation count than in the untreated control and treated cartilages (p<0.05).
DISCUSSION
The radiofrequency energy has been used to remove the unstable superficial layer and contour the cartilage surface. The radiofrequency energy instrument allowed more precise tissue ablation and improved access to the damaged cartilage surface
than do the rotary mechanical debriders and hand instruments.
Turner et al.14)examined the effect of a bipolar ablation probe on experimentally roughened articular cartilage and compared it with the traditional mechanical shaving technique using the knee joint of sheep. The stains used for the specimens were Safranin-O Fast Green and Hematoxylin and Eosin (H-E).
The sections were examined using a modified Mankin Score (visual-analog scale) used for scoring histological damage in articular cartilage. They reported that the less severe histolog- ical change in the bipolar ablative radiofrequency energy treat- ed joints compared with the shave-treated joint suggested that bipolar ablation of articular cartilage might be a better treat- ment for chondromalacia compared with the usual shaving methods of debridement.
Recent analysis of chondrocyte viability using the confocal laser microscopy, however, showed significant chondrocyte death immediately after the procedure7-9). Lu et al. used a var- ious treatment protocol with bipolar a radiofrequency energy instrument for contouring cartilage surface in their series of study: 1) 10-mm linear pass for 3 seconds, non-contact mode (1 mm above cartilage surface) 2) 1 mm/second, contact and non-contact mode 3) 10-mm linear pass over 1.0-cm2area for 5, 10, 15, 20, 30, 40 seconds, non-contact fashion. The con- focal laser microscopic findings were almost identical and sug- gested that bipolar radiofrequency energy delivered through the probes could result in significant chondrocyte death in chondromalacic human articular cartilage in vitro, posing a great danger for creating full-thickness chondrocyte death and subchondral bone necrosis. In their experiments, the speed of wand movement was relatively slow resulting in more ther-
Fig. 5.Confocal microscopic images of cartilage treated in contact mode at power setting S3 (calcein-AM/ethidium homodimer-1 stain,
×20). (A) Single pass of the wand caused partial-thickness carti- laginous tissue ablation and chondrocyte death. (B) After double pass of the wand the tissue was more ablated without further ther- mal damage.
A B
Fig. 6. Confocal microscopic images showing clear demarcation of the thermal damage and tissue ablation in contact mode at power setting S5 (calcein-AM/ethidium homodimer-1 stain, ×20): (A) sin- gle pass, (B) double pass. Power setting S5 removed the cartilagi- nous tissue more efficiently than power setting S3.
A B
Power/Mode of treatment Non-contact mode Contact mode
S1 481624 426953
S3 586345 662909
S5 599033 643571
Untreated cartilage 671912
Preserved cartilage 250610 p<0.05 Table 2.Uptake of 35S-Sulfate in counts per minute on wet weight
mal effect on the cartilage.
According to the manufacturer’s technological note, tissue ablation by bipolar radiofrequency energy is regarded as a non- heat driven process in contrast to conventional electrosurgery.
Radiofrequency energy is applied to a conductive medium, causing a highly focused plasma field to form around the elec- trodes. The plasma field is comprised of highly ionized par- ticles. These ionized particles have sufficient energy to break organic molecular bonds within tissue. Instead of exploding tissue, it causes a low temperature, molecular disintegration.
The result is volumetric tissue removal with minimal collateral tissue necrosis. Power level 3 and non-contact mode of treat- ment is recommended for the Outerbridge grade II cartilage lesion. On the other hand, it recommends using at set point four or five in a contact fashion for the grade III or IV lesions.
But there was no established guideline on the application time of radiofrequency energy and speed of the electrosurgical probe.
To use radiofrequency energy clinically, it seemed to be crit- ical to determine how to deliver radiofrequency energy on articular cartilage. The extent of chondrocyte death depends on several factors: power of radiofrequency energy, application time, mode of treatment (contact or non-contact), velocity of probe, design of probe and flow of the fluid.
In the study, radiofrequency energy was delivered through the electrosurgical probe at a velocity of 10-mm per second.
Confocal laser microscopic findings revealed that any mode of treatment did not cause full-thickness chondrocyte death.
These findings conflicted with those of Lu et al.7-9). We applied the radiofrequency energy to the cartilage surface for shorter time in the experiment than in their study. It suggests that if the velocity of the probe is maintained higher than 10-mm per second chondroplasty procedure can be performed using radiofrequency energy without full-thickness cartilage damage.
However, when the probe was moved at the velocity of 10-mm per second, there was little tissue ablation on the cartilage spec- imen that was treated in the non-contact mode. Even though the amount of tissue ablation was proportional to the power setting and frequency of treatment in the contact mode of treatment, the contact mode of treatment with power setting S1, low power level, was not sufficient to ablate cartilaginous tissue also, and caused more thermal injury to the cartilage.
So low power of radiofrequency energy and non-contact mode of treatment seemed should not to be used for cartilaginous tissue ablation.
In the study of Lu et al.7)there was a difference in depth of penetration between the bipolar radiofrequency energy devices
when evaluated in contact and non-contact modes. They re- garded the reasons for increased penetration for the ArthroCare device in a non-contact mode as related to the probe tip design and to the mechanism of radiofrequency energy similar to using a laser in a defocused mode. In addition, they postulated the ArthroCare device in a contact mode might increase the impedance between the anode and cathode of the device and reduced the temperature achieved at equivalent power settings when comparing contact and non-contact modes. This study, however, revealed the depth of chondrocyte death of non-con- tact mode was not deeper than that of contact mode, suggest- ing that non-contact mode of radiofrequency energy moving 10 mm/sec is not harmful to the articular cartilage neither is it useful clinically.
There was no significant difference of 35S uptakes relating to the modes and power levels. Compared with the findings of confocal laser microscopy, the measurement of incorporated
35S didn’t represent the degree of chondrocyte damage exactly.
It, however, showed that any mode of treatment or power lev- els didn’t cause full-thickness cartilage damage.
CONCLUSION
The non-contact mode of radiofrequency energy treatment was not effective to ablate cartilage tissue even at high power settings. The contact mode of treatment, however, was useful in tissue ablation with higher power levels and repeated appli- cation of radiofrequency energy. The extent of chondrocyte death was not as significant as reported before when the probe moved at the speed of 10 mm/sec. The bipolar radiofrequency energy may be a useful surgical tool with middle range of power levels, contact mode and adequate probe speed to treat chondromalacic cartilage. However the long-term fate of par- tially damaged cartilage by radiofrequency energy has not been investigated yet and further in vivo studies about the long-term benefit of bipolar radiofrequency energy need to be conducted.
REFERENCES
1. Czitrom AA, Keating S and Gross AE: The viability of articular carti- lage in fresh osteochondral allografts after clinical transplantation. J Bone Joint Surg, 72-A: 574-581, 1990.
2. DePalma AF, Tsaltas TT and Mauler GG: Viability of osteochondral grafts as determined by uptake of S35. J Bone Joint Surg, 45-A: 1565-1578, 1963.
3. Dillingham M: Arthroscopic electrothermal surgery of the knee. Oper Techn Sports Med, 6: 154-156, 1998.
4. Fanton GS: Arthroscopic electrothermal surgery of the shoulder. Oper Techn
Sports Med, 6: 139-146, 1998.
5. Grifka J, Boenke S and Schreiner C: Significance of laser treatment in arthroschpic therapy of degenerative gonarthritis. A prospective, randomized clinical study and experimental research. Knee Surg Sports Traumatol Ar- throsc, 2: 88-93, 1994.
6. Kaplan L, Uribe JW, Sasken H and Markarian G: The acute effects of radiofrequency energy in articular cartilage: An in vitro study. Arthroscopy, 16: 2-5, 2000.
7. Lu Y, Edwards RB, Cole BJ and Markel MD: Thermal chondroplasty with radiofrequency energy. An in vitro comparison of bipolar and monopo- lar radiofrequency devices. Am J Sports Med, 29: 42-49, 2001.
8. Lu Y, Edwards RB, Kalscheur VL, Nho S, Cole BJ and Markel MD:
Effect of bipolar radiofrequency energy on human articular cartilage: Com- parison of confocal laser microscopy and light microscopy. Arthroscopy, 17:
117-123, 2001.
9. Lu Y, Edwards RB, Nho S, Heiner JP, Cole BJ and Markel MD: Ther- mal chondroplasty with bipolar and monopolar radiofrequency -Effect of treatment time on chondrocyte death and surface contouring. Arthroscopy, 18: 2002.
10. Mandelbaum BR, Browne JE, Fu F, et al: Articular cartilage lesions of the knee. Am J Sports Med, 26: 853-861, 1998.
11. Obrzut SL, Hecht P, Hayashi K, Fanton GS, Thabit G and Markel MD:The effect of radiofrequency energy on the length and temperature prop- erties of the goenohumeral joint capsule. Arthroscopy, 14: 395-400, 1998.
12. Ohlendorf C, Tomford WW and Mankin HJ: Chondrocyte survival in cryopreserved osteochondral articular cartilage. J Orthop Res, 14: 413- 416, 1996.
13. Rodrigo JJ, Thompson E and Travis C: Deep-freezing versus 4℃ preser- vation of avascular osteocartiligenous shell allografts in rats. Clin Orthop, 218: 268-275, 1988.
14. Turner AS, Tippett JW, Powers BE, Dewell RD and Hallinckrodt CH: Radiofrequency (electrosurgical) ablation of articular cartilage: A study in sheep. Arthroscopy, 14: 585-591, 1998.
15. Wickersheim KA and Sun MH: Fluoroptic thermometry. Med Electron- ics, 84-91, 1987.
16. Wirth CJ and Rudert M: Techniques of cartilage growth enhancement:
A review of the literature [current concepts]. Arthroscopy, 12: 300-308, 1996.