J Korean Soc Transplant
2008;22:267-270 □ 증 례 □
267
책임저자:유영경, 서울시 서초구 반포동 505
가톨릭대학교 강남성모병원 간담췌외과, 137-701 Tel: 02-590-2686, Fax: 02-590-1406
E-mail: yky602@catholic.ac.kr
접수일:2008년 9월 30일, 게재승인일:2008년 11월 11일
Living-Donor Liver Transplantation with Renoportal Anastomosis using an Interposition Polytetrafluoroethylene Graft for a Patient with Large Spontaneous Splenorenal Shunt: A Case Report
Department of Hepato-Biliary-Pancreas-Surgery, The Catholic University of Korea College of Medicine, Seoul, Korea Young Kyoung You, M.D., Sang Kuon Lee, M.D., Jung Hyun Park, M.D., Dong Goo Kim, M.D. and Kyung Keun Lee, M.D.
비장정맥-신정맥간의 큰 측부 혈행이 있는 환자에 서 폴리테트라플루오로에틸렌 인조혈관을 이용한 신정맥-간문맥 문합 생체부분 간이식 1예
가톨릭대학교 의과대학 강남성모병원 간담췌외과 유영경ㆍ이상권ㆍ박정현ㆍ김동구ㆍ이경근
간이식 수술에서 적절한 문맥 혈류의 확보는 필수적인 요 소이다. 말기 간질환 환자에서는 비장정맥과 신정맥간의 큰 측부 혈행과 이로 인한 문맥혈류의 감소를 흔히 볼 수 있다. 간 이식수술에서는 이식 편으로의 문맥혈류를 충분 히 확보하기 위하여 측부 혈행을 차단해야 하는데 이러한 술기는 출혈 등의 위험이 커서 매우 힘든 수술 조작이다.
한편 생체부분 간이식에서는 적절한 크기의 대치혈관을 얻기가 곤란한 경우가 있으므로 이를 확보하는 것이 때로 는 중요하다. 저자들은 비장정맥-신정맥간의 큰 측부 혈 행이 있는 52세 남자 환자에서 신정맥-간문맥 문합 생체 부분 간이식을 시행하였는데, 좌 신 정맥을 하대정맥 부위 에서 분리하고 좌신 정맥의 원위부와 이식편의 문맥을 16 mm 폴리테트라플루오로에틸렌 인조혈관을 이용하여 단 단문합하여 측부 혈행을 보존하였다. 환자는 수술 후 6 병 일째 이식 간 주위의 출혈로 혈종제거술 및 지혈술, 수술 후 12병일째 간문맥의 혈전제거술을 받고 이식 수술 10주 후 좋은 상태로 퇴원하였다. 폴리테트라플루오로에틸렌 인조혈관을 이용한 신정맥-간문맥 문합 생체부분 간이식 은 비장정맥-신정맥간의 큰 측부 혈행이 있는 환자에서
시행할 수 있는 술식이라고 본다.
(대한이식학회지2008;22:267-270)
중심 단어: 생체부분 간이식, 비장정맥-신정맥간의 측부 혈행, 신정맥-간문맥 문합, 폴리테 트라플루오로에틸렌 인조혈관
INTRODUCTION
Adequate portal inflow is an essential component in the liver transplantation. Not a few patients suffering from the end-stage liver disease have portal hypertension accompanied by collateral circulation that bypasses the portal inflow. Among these, splenorenal collateral is one of the common spontaneous portosystemic connections. Although most of these patients are successfully transplanted with conventional surgical procedure, patients who have portal vein thrombosis or poor portal inflow require an additional reconstruction technique. Direct approach to the collateral circulation for diversion of portal flow to the graft in the liver transplantation in patient with portal hypertension is extremely challenging for the patient because of bleeding, and usually it is not successful in the restoration of adequate portal circulation. Concomitant splenectomy would increase the risk of infection and portal vein thrombosis after liver transplantation.(1) Miyamoto et al. reported that the renoportal anastomosis using recipient internal jugular vein graft in the living donor liver transplantation is an effective method of portal vein reconstruction in a patient with large spontaneous splenorenal collateral.(2)
Herein, we describe a successful end-to-end renoportal anastomosis to maintain adequate portal inflow in living-donor liver transplantation using an interposition polytetrafluoroethylene (PTFE) (W. L. Gore & Associates, Inc, Flagstaff, Ariz) graft for a patient who has large spontaneous splenorenal shunt.
CASE REPORT
A 53 year-old man weighing 43 kg has been diagnosed with
alcoholic liver cirrhosis when he was 35 years old. Liver
function had gradually deteriorated and preoperative computed
268 대한이식학회지:제 22 권 제 2 호 2008
Fig. 1. Preoperative abdominal CT scan revealed a large spontaneous splenorenal collateral (arrow).
Fig. 2. Schematic illustration of renoportal anastomosis using an interposition polytetrafluoroethylene graft for a patient with large spontaneous splenorenal shunt.
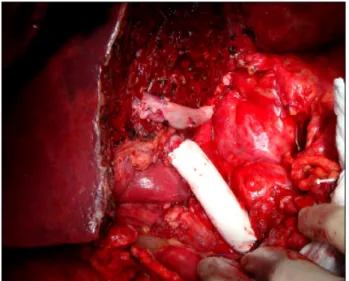
Fig. 3. Portal vein anastomosis. The donor portal vein is anastomosed to the left renal vein with an interposition polytetrafluoro- ethylene graft in an end-to-end fashion.
tomography scan and ultrasound revealed markedly narrowed portal vein due to organized thrombus with small hepatofugal portal flow and a large spontaneous splenorenal collateral (Fig.
1). Living donor liver transplantation using the right hemiliver (820 gram, graft-to-body weight ratio : 1.9) from his son was performed.
1) Operative procedure
At surgery, massive ascites, markedly shrinked cirrhotic liver, and huge engorged collateral veins were found around the pancreas and stomach. The extrahepatic portal vein which showed phlebosclerotic change was isolated without difficulty.
The area of spleno-superior mesenteric venous confluence was not able to approach due to abundant venous collaterals. The duodenal second portion and pancreatic head area were mobilized from the anterior surface of inferior vena cava through the relatively avascular plane, and full length of left renal vein was exposed with careful preservation of collaterals. After total hepatectomy of the recipient, the left renal vein was divided at the inferior vena caval joining point. The vena caval stump of left renal vein was suture closed and the distal left renal vein was anastomosed to a 16 mm in diameter interposition PTFE graft which was 6 centimeter in length in an end-to-end fashion (Fig. 2, 3). A right hepatic lobe graft was harvested from his 25 year-old son. At back table, the main right hepatic vein of the graft and the middle hepatic vein was anastomosed using a cryopreserved cadaveric iliac artery interposition graft to make large single hole for the anastomosis. Additional nearby located two inferior right hepatic veins were joined together as
a single lumen in a fish-mouth fashion. Then, the graft was
placed orthotopically and all of the graft hepatic veins were
anastomosed to the inferior vena cava. The graft portal vein
was anastomosed to the interposition PTFE graft. The clamps
applied to the hepatic venous outflow and portal inflow were
removed, and the graft liver was reperfused. The cold and
warm ischemic time was 135 min and 45 min, respectively. The
liver was reperfused promptly from the blood flow through the
left renal vein. Using microsurgical technique, the arterial
anastomosis was performed and the duct-to-duct biliary
reconstruction was done. Adequate blood flow in the intrahepatic
Young Kyoung You, et al:Living-Donor Liver Transplantation with Renoportal Anastomosis using an Interposition Polytetrafluoroethylene Graft 269
Fig. 4. Reconstructed angio-CT image 3 months after transplantation showing a patent interposition polytetrafluoroethylene graft (arrow).
portal vein, hepatic artery and hepatic veins were detected on intraoperative Doppler ultrasonography before abdominal wall closure.
2) Postoperative course
Hypovolemic shock and active bleeding from drains developed on the 6
thpostoperative day, and exploratory laparotomy was performed. At surgery, minor bleeders in the perihepatic area were successfully controlled. Liver function deteriorated abruptly on the 12
thpostoperative day, and reexploratory laparotomy was performed. There was huge hematoma around the porta hepatis and perihepatic space, and the interposition PTFE graft was displaced and collapsed, filled with thrombus. After hematoma removal and subsequent thrombectomy in the interposition PTFE graft, liver function recovered gradually. Since then, adequate portal blood flow and patency of the interposition PTFE graft was maintained throughout the postoperative period, which was determined by serial Doppler ultrasound and contrast-enhanced axial tomography scan. The patient was discharged with normal graft function 10 weeks after transplantation. Endoscopic retrograde biliary stent was inserted 3 months after transplantation owing to postoperative bile duct stricture. Angiographic computed axial tomography 3 months after liver transplantation revealed adequate hepatic parenchymal perfusion and sufficient portal inflow from the splenorenal collateral (Fig. 4). Flow rate in the portal vein ranged from 700
∼900 mL/minute throughout the postoperative course. Also, patent left renal vein and interposition graft were observed.
DISCUSSION
Until now, the only therapeutic modality for end-stage liver disease is liver transplantation whether cadaveric or living-related. Not a few end-stage liver disease patients have portal vein thrombosis which is an obstacle for liver transplantation.(3,4) The outcome of liver transplantation in severe grade of portal vein thrombosis is relatively poor, but in most cases the operative procedures such as portal venous thrombectomy, low dissection, mesoportal jump graft can be the solution for the adequate portal inflow.(3) Often, diffuse portal thrombosis and abundant collaterals do not allow to dissect the splanchnic venous structures in the peripancreatic area. Therefore, the flow from the vena cava or renal vein is used sometimes for the portal inflow. Although the long-term outcomes remains unknown, cavoportal or renoportal anastomosis have been performed in selected cases of the insufficient portal inflow and diffuse portal vein thrombosis.(5) Occlusion of the portal venous system had led to splenorenal collaterals, however interruption of the collaterals to divert portal flow to the hepatic graft in liver transplantation is very challenging and dangerous procedure due to markedly engorged and friable vessels. Excellent outcome of the end-to-end renoportal anastomosis in liver transplantation after surgical splenorenal shunt was reported in 5 patients, including two patients with hepatofugal portal flow and one, with phlebosclerotic, very small portal venous status.(6) Miyamoto et al. performed the renoportal anastomosis for the first time in living-related liver transplantation using an interposition graft harvested from the left internal jugular vein.(2)
In our case, the patient had a grade II portal venous thrombosis,
which is an 80% of the lumen occluded with organized thrombus.(3)
First, we tried to dissect the splenomesenteric confluence for
the anastomosis, but that area was not accessible due to
engorged collaterals and retropancreatic portion of the
mesenteric vein was too small with insufficient flow for the
anastomosis in this relatively large (graft to body weight ratio
1.9) hepatic graft. For the interposition graft, diameter of the
autogenic graft such as internal jugular vein or iliac vessels of
the recipient was too small, so we used 16 mm in diameter
PTFE graft which is one of the limbs a bifurcated 8×16 mm
graft for the size matching to the left renal vein. On postoperative
12
thday, relaparotomy due to acute portal vein occlusion was
performed. External compression by the hematoma surrounding
porta hepatis was suspected as a direct cause of this acute
thrombosis. After hematoma evacuation and endvenectomy, an
270 대한이식학회지:제 22 권 제 2 호 2008
Adequate portal perfusion is essential in liver transplantation. End-stage liver disease is often accompanied by a large spontaneous splenorenal shunt and poor portal flow. To secure an adequate portal perfusion of the graft, collaterals including splenorenal shunt should be interrupted during liver transplantation. However, this procedure is usually too demanding because of massive bleeding, as well as time-consuming. As in living-donor liver transplantation size-matched liver graft and vascular grafts are not always available, an alternative must be sought. We performed living-donor liver transplantation with renoportal anastomosis in a 52 year-old male with a large spontaneous splenorenal shunt. During surgery, left renal vein was divided at the caval junction and the distal stump was end-to-end anastomosed to the graft portal vein using 16 mm interposition polytetrafluoroethylene graft without ligation of collaterals. The initial postoperative course of this patient was uneventful. However, on postoperative day 6 and 12 perihepatic hematoma evacuation and portal vein graft thrombectomy were performed respectively. Since then, adequate portal blood flow and patency of the interposition polytetrafluoroethylene graft was maintained throughout the postoperative period. The patient was discharged with normal graft function 10 weeks after transplantation. Renoportal anastomosis using an interposition polytetrafluoroethylene graft in living-donor liver transplantation could be an acceptable alternative for patients with end-stage liver disease with a large spontaneous splenorenal shunt. (J Korean Soc Transplant 2008;22:267-270)
Key Words: Living-donor liver transplantation, Spontaneous splenorenal shunt, Renoportal anastomosis, Interposition polytetrafluoroethylene graft
Abstract
additional closed suction drain was placed around interposition PTFE graft for the protection from further external compression by hematoma. The disadvantage of poor expandability and easily collapsible PTFE graft can be overcome by using a PTFE graft especially manufactured for the venous interposition. During the postoperative course in our patient, renal function was well maintained; however, moderate ascites were noted during the 10-week hospitalization.
In conclusion, renoportal anastomosis using an interposition PTFE graft in living-donor liver transplantation could be an acceptable alternative for selected patients with end-stage liver disease with a large spontaneous splenorenal shunt.
REFERENCES
1) Yoshizawa A, Sakamoto S, Ogawa K, Kasahara M, Uryuhara K, Oike F, et al. New protocol of immunosuppression for liver transplantation across ABO barrier: the use of Rituximab, hepatic arterial infusion, and preservation of spleen. Transplant
Proc 2005;37:1718-9.
2) Miyamoto A, Kato T, Dono K, Umeshita K, Kawabata R, Hayashi S, et al. Living-related liver transplantation with renoportal anastomosis for a patient with large spontaneous splenorenal collateral. Transplantation 2003;75:1596-8.
3) Yerdel MA, Gunson B, Mirza D, Karayalcin K, Olliff S, Buckels J, et al. Portal vein thrombosis in adults undergoing liver transplantation: risk factors, screening, management, and outcome. Transplantation 2000;69:1873-81.
4) Paskonis M, Jurgaitis J, Mehrabi A, Kashfi A, Fonouni H, Strupas K, et al. Surgical strategies for liver transplantation in the case of portal vein thrombosis - current role of cavoportal hemitransposition and renoportal anastomosis. Clin Transplant 2006;20:551-62.
5) Azoulay D, Adam R, Castaing D, Muresan S, Essomba A, Vibert E, et al. Liver transplantation with cavoportal or re- noportal anastomosis: a solution in cases of diffuse portal thrombosis. Gatroenterol Clin Biol 2002;26:325-30.
6) Kato T, Levi DM, DeFaria W, Nishida S, Tzakis AG. Liver transplantation with renoportal anastomosis after distal sple- norenal shunt. Arch Surg 2000;135:1401-4.