Spinal fractures commonly occur in the thoracolumbar region, with burst fractures accounting for 21% to 58%
of all thoracolumbar fractures.1-3) Most authors believe that burst fractures require surgical intervention; how- ever, there is some controversy regarding treatment.4,5) Advances in spinal instrumentation have brought short- segment instrumentation into successful clinical practice.
Among the surgical methods for thoracolumbar burst fractures, short-segment pedicle screw fixation (SSPSF) is the most common and simple treatment option.6) On the other hand, many studies have shown that SSPSF alone led to a high incidence of implant failure and kyphosis recur- rence, which accounted for approximately 9% to 54%.7) Moreover, collapse of the disc space and recurrent kypho- sis are commonly observed after instrumented reduction of thoracolumbar vertebral burst fractures.7,8) Whether correction loss can be influenced mainly by the fractured vertebral body or the disc-endplate complex is uncertain.
This study examined the relationship between superior disc-endplate complex (SDEC) injury and reduction loss after SSPSF in a group of young adult patients with stable
The Relationship between Superior Disc-Endplate Complex Injury and Correction Loss in
Young Adult Patients with Thoracolumbar Stable Burst Fracture
Kyu Yeol Lee, MD, Min-Woo Kim, MD, Sang Yun Seok, MD, Dong Ryul Kim, MD, Chul Soon Im, MD
Department of Orthopedic Surgery, Dong-A University College of Medicine, Busan, Korea
Background: To determine the relationship between superior disc-endplate complex injury and correction loss after surgery in a group of young adult patients with a stable thoracolumbar burst fracture.
Methods: The study group was comprised of young adult patients who had undergone short-segment posterior fixation and bone grafting under the diagnosis of a stable thoracolumbar burst fracture from March 2008 to February 2014. Follow-up was available for more than 1 year. Before surgery, magnetic resonance imaging was performed to determine injury to the anterior longitudinal ligament, posterior longitudinal ligament, and superior and inferior intervertebral discs and endplates. Correction loss was evaluat- ed by the Cobb angle, intervertebral disc height, upper intervertebral disc angle, vertebral wedge angle, and vertebral body height.
Results: No significant relation was noted between correction loss and an injury to the anterior longitudinal ligament, posterior longitudinal ligament, inferior intervertebral disc/endplate, and fracture site, whereas an injury to the superior endplate alone and superior disc-endplate complex showed a significant association. Specifically, a superior intervertebral disc-endplate complex injury showed statistically significant relation to postoperative changes in Cobb angle (p = 0.026) and vertebral wedge angle (p = 0.047).
Conclusions: A superior intervertebral disc-endplate complex injury may have an influence on the prognosis after short-segment fixation in young adult patients with a stable thoracolumbar burst fracture.
Keywords: Stable burst fracture, Short segment fusion, Correction loss
Copyright © 2017 by The Korean Orthopaedic Association
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Clinics in Orthopedic Surgery • pISSN 2005-291X eISSN 2005-4408 Received April 20, 2017; Accepted July 6, 2017
Correspondence to: Min-Woo Kim, MD
Department of Orthopedic Surgery, Dong-A University College of Medicine, 32 Daesingongwon-ro, Seo-gu, Busan 49201, Korea
Tel: +82-51-240-5166, Fax: +82-51-254-6757 E-mail: drkimminwoo@naver.com
thoracolumbar burst fractures (STLBFs).
METHODS
This study reviewed retrospectively 37 patients followed up for a minimum of 1 year among adult patients younger than age 45 years who had undergone short-segment posterior fixation and allograft after being diagnosed with a stable burst fracture of the thoracolumbar spine from March 2008 to February 2014. A stable burst fracture is a descriptive term for compressive injury to the anterior and middle columns of the vertebral body due to axial compression, and the posterior column is typically normal or associated with a vertical fracture of the vertebral arch.
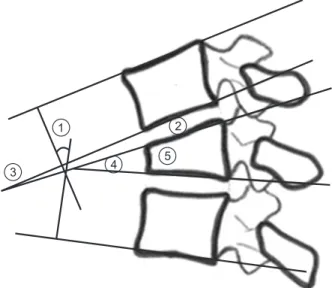
The indications for surgery were the patient wanting to re- turn to his/her daily life early and presence of one or more of the following three radiological findings: (1) 30% or higher compression rate of the fractured anterior column of the vertebral body; (2) sagittal index of 15° or greater (sagittal index is the measurement of kyphosis at a motion segment [1 vertebra and 1 disc] adjusted for the baseline sagittal contour at the level); and (3) invasion of bone frag- ments into the spinal canal by 30%. For kyphosis correc- tion and reduction of the collapsed vertebral body, fixation was performed using the mono-axial pedicle screw system by bending a metal rod for a slight overcorrection of ky- phosis after inserting pedicle screws parallel to the epiphy- seal plate into the normal vertebral bodies located superior and inferior to the fractured vertebral body. In all cases, bone allograft was performed through the dorsal portion of the lamina after decortication to support the fractured vertebra. All procedures were conducted by a single spine surgeon (KYL) using the same surgical technique. The surgical instrument used was a posterior vertebral fixation device (Mega Spine set from BK Meditech, Hwaseong, Korea). All patients were placed on bed rest for an aver- age of 2.2 days (range, 1 to 3 days) after surgery, and were allowed to start ambulation using ambulatory assistive devices. After confirming bone union or stabilization of the fractured vertebra at an outpatient follow-up, the assis- tive devices were removed at 11.7 weeks postoperation on average. The degree of postoperation reduction loss was assessed by examining the Cobb angle (CA), intervertebral disc height (IDH), upper intervertebral disc angle (UIDA), vertebral wedge angle (VWA), and anterior vertebral body height (AVBH) on the radiographs taken immediately and 1 year after surgery, and the changes were calculated. Mea- surements were performed three times each by two spine specialists using a digital ruler and a protractor on the true lateral views of the spine radiographs taken precisely using
a picture archiving and communication system. The in- traclass correlation coefficient between the two observers was calculated as 0.873 (range, 0.796 to 0.925) indicating a high agreement. Thus, the average of the measurements obtained by two observers was used for analysis. The CA was measured between the superior margin of the upper vertebra and the inferior margin of the lower vertebra in- cluded in spine fusion. The IDH was defined as the mini- mum distance between the superior margin of the injured vertebra and the inferior margin of the upper vertebra.
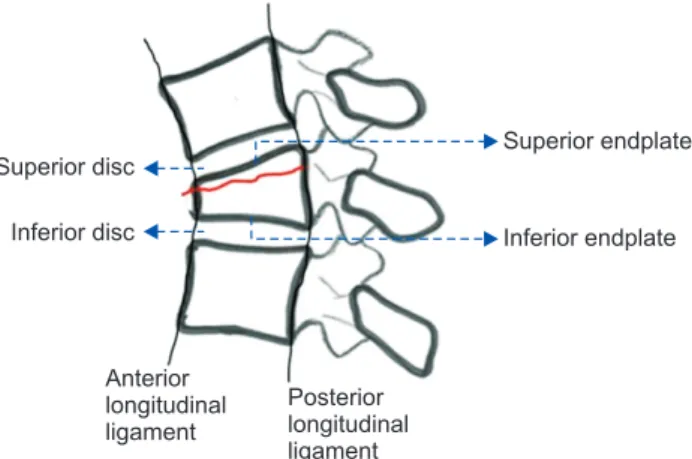
The UIDA was measured between the superior margin of the vertebra and the inferior margin of the upper vertebra at the hinge area in a wedge-shaped deformity of the in- jured spine after fracture. The VWA was defined as the an- gle between the superior margin and the inferior margin of the injured vertebral body, while the AVBH was defined as the height of the anterior vertebral body of the fractured area (Fig. 1). To explore the relationship between injury to the vertebral structures and the degree of reduction loss, the presence of injuries to the anterior longitudinal liga- ment (ALL), posterior longitudinal ligament (PLL), and the superior and inferior discs and endplates was exam- ined based on the preoperative magnetic resonance imag- ing (MRI) findings (Fig. 2). An injury was defined as any continuity loss of each structure, signal change, or edema.9) The impacts of the injuries of the ALL, PLL, fractured vertebral area, superior disc, superior endplate, inferior disc, and inferior endplate on radiological reduction loss were evaluated. Furthermore, the different effects of SDEC
1 2
3 4 5
Fig. 1. Radiological evaluation using plain lateral radiography. ①: Cobb angle, ②: intervertebral disc height, ③: upper intervertebral disc angle,
④: vertebral wedge angle, ⑤: anterior vertebral body height.
injury and superior endplate injury alone on radiological reduction loss were compared based on the assessment of changes for radiological parameters.
All statistical analyses were performed using IBM SPSS ver. 19.0 (IBM Corp., Armonk, NY, USA). To deter- mine statistical significance, a Mann-Whitney U-test was used for comparison of two variables, and a Kruskal-Wallis test was used for comparison of more than three variables.
We conducted this study in compliance with the principles of the Declaration of Helsinki. The protocol of this study was reviewed and approved by the Institu- tional Review Board of Dong-A University Hospital (IRB No. DMC 2017-09-013-001). The informed consent was
waived.
RESULTS
A total of 37 subjects (26 male and 11 female patients) were enrolled in this study. Their mean age was 37.2 years (range, 21 to 44 years). The causes of injury were falls in 27 cases, traffic accidents in nine, and blunt trauma by the impact of an object in one. The mean duration from in- jury to surgery was 4.7 days, and the mean follow-up was 13.4 months. On the preoperative MRI scans, the ALL was injured in 35 cases and not injured in two, whereas the PLL was injured in 30 cases and not injured in seven. The most frequently injured level was L1 in 16 cases, followed in order by L2 in eight cases, L3 in six, T12 in four, and L4 in three. On the superior endplate injuries, injury to both the disc and endplate regions was observed in 20 cases; the endplate alone was injured in 12; and no injury was pres- ent in five. On the inferior endplate injuries, both the disc and endplate were injured in four cases; injury to the end- plate alone was observed in five, and none of these areas was injured in 28. Statistical analysis data on the impact of the presence of injuries on radiological parameters of re- duction loss are presented in Tables 1 and 2. No significant relation was observed between reduction loss and the ALL or PLL injury, level of the fractured vertebra, and injury to the inferior disc/endplate. On the other hand, there was a statistically significant difference in the change of CA (p
= 0.026) among patients with the superior endplate injury Fig. 2. Radiological evaluations using T2-weighted sagittal magnetic
resonance imaging.
Superior disc
Inferior disc
Superior endplate
Inferior endplate
Anterior longitudinal ligament
Posterior longitudinal ligament
Table 1. Factors Affecting the Change of Radiologic Parameters Presence
of injury No.
Cobb angle difference Disc height difference Upper intervertebral disc angle difference Vertebral wedge
angle difference Anterior vertebral body height difference Mean ± SD p-value Mean ± SD p-value Mean ± SD p-value Mean ± SD p-value Mean ± SD p-value
ALL ○ 35 11.6 ± 2.2 0.168 1.6 ± 1.9 0.363 3.8 ± 3.0 0.243 6.9 ± 2.7 0.508 1.5 ± 1.6 0.589
× 2 3.3 ± 1.6 2.9 ± 1.2 7.9 ± 2.2 9.7 ± 3.9 0.1 ± 1.3
PLL ○ 30 10.6 ± 3.4 0.835 1.5 ± 2.2 0.293 3.6 ± 2.0 0.100 6.9 ± 3.8 0.690 1.1 ± 2.5 0.531
× 7 13.5 ± 3.9 2.3 ± 1.7 5.9 ± 2.7 7.7 ± 2.4 2.4 ± 1.6
Level L1 16 11.9 ± 5.4 0.123 1.6 ± 1.4 0.843 4.2 ± 1.6 0.828 5.9 ± 3.3 0.268 1.6 ± 2.8 0.564
L2 8 11.0 ± 6.5 1.6 ± 2.7 3.3 ± 2.0 8.5 ± 4.0 0.2 ± 4.8
L3 6 10.8 ± 4.6 1.2 ± 1.1 4.8 ± 2.3 6.5 ± 4.6 0.4 ± 4.0
L4 3 1.5 ± 1.9 1.6 ± 1.1 4.0 ± 3.1 1.7 ± 3.4 3.3 ± 2.1
T12 4 16.8 ± 5.0 2.4 ± 1.6 3.6 ± 2.4 13.9 ± 7.4 3.0 ± 1.8
SD: standard deviation, ALL: anterior longitudinal ligament, PLL: posterior longitudinal ligament.
alone, SDEC injury, and none of the injuries (Fig. 3). A significant difference was also observed in the change in CA (p = 0.029) and VWA (p = 0.047) between patients with a SDEC injury and those with a superior endplate in- jury alone (Table 3).
DISCUSSION
This study revealed the relationship between preopera- tive SDEC injury and correction loss after SSPSF with a bone graft in young adult patients with a STLBF. Jun et al.9) reported that ALL injury, superior endplate and disc injury, and high level of bone edema were critical factors that determine the progression of a kyphotic deformity in conservatively treated STLBFs. However, there are only a few reports on the influence of disc and endplate injury on the postoperative outcomes in patients with STLBFs. Age, osteoporosis, and degree of comminution of the vertebral body are the known risk factors for poor surgical out- comes in thoracolumbar burst fractures.10,11) In this study, we assessed the influence of disc and endplate injury in adult patients younger than 45 years and diagnosed with an STLBF without any injury to the posterior structures.
Although collapse of the disc common in STLBFs, the mechanism has yet to be established. A disruption of the vascularity of the endplates is believed to be one of the major causes of the degenerative disc disease.12,13) Zhao et al.14) noted that when the vertebrae are compressed naturally by the adjacent intervertebral discs, superior endplates usually fail before the inferior endplates because they are thinner and supported by less dense trabecular bone. The vertebral endplates contain marrow cavities that allow the bone marrow to lie adjacent to the calcified hyaline cartilage, which is widely regarded as an important route for metabolite transport.15) An endplate injury is likely to result in disc degeneration due to calcification and blocking of the endplate’s nutritional route. In the present study, a disc injury did not occur solely but appeared only in association with an endplate injury. A disc injury occurs after an endplate injury develops. Changes in radiologi- cal parameters of reduction loss during the postoperative follow-up had no significant association with an ALL injury, PLL injury, level of vertebral injury, and inferior structure (disc/endplate) injury. On the other hand, a su- perior structure (disc/endplate) injury had a statistically significant influence on the CA and VWA. Furthermore, combined injury to the superior disc and endplate was more common than that to the inferior disc and endplate, and SDEC injury occurred more frequently than superior endplate injury alone. In light of these findings, we believe Table 2. Factors Affecting the Change of Radiologic Parameters Presence of injury No.Cobb angle differenceIntervertebral disc height differenceUpper intervertebral disc angle differenceVertebral wedge angle differenceAnterior vertebral body height difference EndplateDiscMean ± SDp-valueMean ± SDp-valueMean ± SDp-valueMean ± SDp-valueMean ± SDp-value Superior○○2015.1 ± 4.50.0262.4 ± 2.00.3024.3 ± 3.30.3338.4 ± 2.80.1371.8 ± 1.10.665 ○×12 7.2 ± 3.40.8 ± 1.32.9 ± 2.47.4 ± 3.80.8 ± 1.1 ×× 5 5.2 ± 1.90.6 ± 2.15.7 ± 2.51.1 ± 2 .71.2 ± 2.0 Inferior○○ 414.9 ± 3.80.1872.1 ± 2.80.3985.2 ± 2.10.6403.4 ± 2.50.3303.6 ± 2.80.379 ○× 5 5.6 ± 1.80.4 ± 2.33.0 ± 2.93.7 ± 2.60.9 ± 2.5 ××2811.6 ± 3.61.8 ± 2.94.0 ± 3.28.2 ± 3.01.2 ± 1.7 SD: standard deviation.
that the frequency of SDEC injury is high in patients with STLBFs, and SDEC injury appears to influence postopera- tive radiological results.
Rigid screw fixation with fusion might also lead to stress shielding of the intervertebral disc, resulting in bio- chemical changes.16) Previous MRI studies showed that the signal intensity change of the disc was observed in most cases and the most significant changes were related to morphological alterations in the disc space.17,18) Posterior reduction with pedicle screw instrumentation probably reduces only the periphery of the endplate with its strong
annular attachments, while the central area remains de- pressed. Therefore, one of the major mechanisms of loss of correction may be the creeping of the disc back into the central depression of the endplate. Knop et al.19) showed that the VWA on the initial injury film correlated signifi- cantly with the postoperative loss of reduction. The pres- ent study showed that the postoperative VWA was related to SDEC injury. Interestingly, the group with an SDEC injury and the group with a superior endplate injury only showed similar changes in the IDH and UIDA during the postoperative follow-up, but significant differences Fig. 3. (A-D) Magnetic resonance imaging (MRI) scans and X-rays showing correction loss in a patient with superior disc-endplate injury. The Cobb angle decreased (dotted lines) in the patient. (E-H) MRI scans and X-rays of a patient without correction loss. (A, E) Initial X-rays. (B, F) Initial T2 MRI scans. (C, G) Postoperative X-rays. (D, H) One-year follow-up X-rays.
A B C D
E F G H
Table 3. Impact of the Superior Disc-Endplate Complex and Superior Endplate Injury Alone
Presence of injury No.
p-value Cobb angle
difference
Intervertebral disc height
difference
Upper intervertebral disc angle difference
Vertebral wedge angle
difference
Anterior vertebral body height
difference
Superior disc-endplate complex 20 0.029 0.146 0.307 0.047 0.454
Superior endplate alone 12
between the groups were noted in the changes of CA and VWA. The presence of disc injury had been expected to affect the postoperative disc height and disc angle. How- ever, we found that disc-endplate complex injury could have a greater impact on the vertebral body morphology compared to an endplate injury alone. In addition, disc injury appeared to have an insignificant impact on the disc morphology. Such short-term follow-up findings may be attributed to six-screw fixation and rigid fixation with bone grafting. However, it is difficult to predict correction loss based on the follow-up radiograph because the cor- relations among the variable parameters were relatively weak. To decrease correction loss, surgeons who perform SSPSF should pay more attention to restoring the fractured VWA.
The addition of pedicle screws in the fractured vertebra improves fracture reduction, and through the lordosis effect, provides a better chance of placing the fractured vertebral body in front of the gravity line.20) Simultaneously, it creates a buttress effect that allows ver- tebral body fracture healing before collapse. In the present study, there were only four cases with a load sharing clas- sification score higher than 7 points. However, this study was not designed to examine the effects of vertebral body comminution on radiological outcomes and compare the study results according to the load sharing classification score. We performed fixation using six pedicle screws in the superior and inferior vertebral bodies including the
fractured area for stabilization of the fracture site. Despite the remaining controversy over the treatment efficacy, bone union and slight correction loss were observed and the integrity of pedicle screw fixation using an allograft was maintained in the first postoperative year. Additional studies are needed to determine if the anterior support is essential considering the posterior column and posterior ligament complex are intact in STLBFs.
This study had some limitations. Clinical outcomes were not included in the analysis; thus, the relationship between radiological findings and clinical outcomes is still a matter of discussion. Further research involving a larger patient population and a more long-term follow-up is war- ranted to address the unresolved issue. Other limitations include the retrospective study design and assessment of parameters on the lateral plain radiographs.
A superior intervertebral disc-endplate complex in- jury may have an impact on the prognosis after short-seg- ment fixation in young adult patients who have a STLBF.
Correction loss after SSPSF assessed by CA and VWA may be associated with superior intervertebral disc-endplate complex injury in STLBFs.
CONFLICT OF INTEREST
No potential conflict of interest relevant to this article was reported.
REFERENCES
1. Dai LY, Yao WF, Cui YM, Zhou Q. Thoracolumbar fractures in patients with multiple injuries: diagnosis and treatment.
A review of 147 cases. J Trauma. 2004;56(2):348-55.
2. Gertzbein SD. Scoliosis Research Society: multicenter spine fracture study. Spine (Phila Pa 1976). 1992;17(5):528-40.
3. McCormack T, Karaikovic E, Gaines RW. The load shar- ing classification of spine fractures. Spine (Phila Pa 1976).
1994;19(15):1741-4.
4. Kaneda K, Taneichi H, Abumi K, Hashimoto T, Satoh S, Fujiya M. Anterior decompression and stabilization with the Kaneda device for thoracolumbar burst fractures as- sociated with neurological deficits. J Bone Joint Surg Am.
1997;79(1):69-83.
5. Katonis PG, Kontakis GM, Loupasis GA, Aligizakis AC, Christoforakis JI, Velivassakis EG. Treatment of unstable thoracolumbar and lumbar spine injuries using Cotrel- Dubousset instrumentation. Spine (Phila Pa 1976).
1999;24(22):2352-7.
6. Shin TS, Kim HW, Park KS, Kim JM, Jung CK. Short- segment pedicle instrumentation of thoracolumbar burst- compression fractures: short term follow-up results. J Ko- rean Neurosurg Soc. 2007;42(4):265-70.
7. Wang XY, Dai LY, Xu HZ, Chi YL. Kyphosis recurrence after posterior short-segment fixation in thoracolumbar burst fractures. J Neurosurg Spine. 2008;8(3):246-54.
8. Wang J, Zhou Y, Zhang ZF, Li CQ, Zheng WJ, Liu J. Radio- logical study on disc degeneration of thoracolumbar burst fractures treated by percutaneous pedicle screw fixation.
Eur Spine J. 2013;22(3):489-94.
9. Jun DS, Shin WJ, An BK, Paik JW, Park MH. The relation- ship between the progression of kyphosis in stable thoraco- lumbar fractures and magnetic resonance imaging findings.
Asian Spine J. 2015;9(2):170-7.
10. Kim HS, Kim SW, Ju CI, Lee SM, Shin H. Short segment fixation for thoracolumbar burst fracture accompanying osteopenia: a comparative study. J Korean Neurosurg Soc.
2013;53(1):26-30.
11. Sapkas G, Kateros K, Papadakis SA, Brilakis E, Macheras G, Katonis P. Treatment of unstable thoracolumbar burst fractures by indirect reduction and posterior stabilization:
short-segment versus long-segment stabilization. Open Or- thop J. 2010;4:7-13.
12. Cinotti G, Della Rocca C, Romeo S, Vittur F, Toffanin R, Trasimeni G. Degenerative changes of porcine intervertebral disc induced by vertebral endplate injuries. Spine (Phila Pa 1976). 2005;30(2):174-80.
13. Kerttula LI, Serlo WS, Tervonen OA, Paakko EL, Vanharan- ta HV. Post-traumatic findings of the spine after earlier vertebral fracture in young patients: clinical and MRI study.
Spine (Phila Pa 1976). 2000;25(9):1104-8.
14. Zhao FD, Pollintine P, Hole BD, Adams MA, Dolan P. Verte- bral fractures usually affect the cranial endplate because it is thinner and supported by less-dense trabecular bone. Bone.
2009;44(2):372-9.
15. Urban JP, Smith S, Fairbank JC. Nutrition of the interverte- bral disc. Spine (Phila Pa 1976). 2004;29(23):2700-9.
16. Brickley-Parsons D, Glimcher MJ. Is the chemistry of col- lagen in intervertebral discs an expression of Wolff's Law?
A study of the human lumbar spine. Spine (Phila Pa 1976).
1984;9(2):148-63.
17. Oner FC, van der Rijt RR, Ramos LM, Dhert WJ, Verbout AJ. Changes in the disc space after fractures of the thoraco- lumbar spine. J Bone Joint Surg Br. 1998;80(5):833-9.
18. Oner FC, van Gils AP, Faber JA, Dhert WJ, Verbout AJ.
Some complications of common treatment schemes of tho- racolumbar spine fractures can be predicted with magnetic resonance imaging: prospective study of 53 patients with 71 fractures. Spine (Phila Pa 1976). 2002;27(6):629-36.
19. Knop C, Fabian HF, Bastian L, Blauth M. Late results of thoracolumbar fractures after posterior instrumentation and transpedicular bone grafting. Spine (Phila Pa 1976).
2001;26(1):88-99.
20. Guven O, Kocaoglu B, Bezer M, Aydin N, Nalbantoglu U. The use of screw at the fracture level in the treatment of thoracolumbar burst fractures. J Spinal Disord Tech.
2009;22(6):417-21.