Palliative Hepatectomy for Advanced Hepatocellular Carcinoma with Multiple Metastases: A Case Report
Non-surgical treatment is usually performed for the cases of hepatocellular carcinoma (HCC) that are not suitable for curative treatment, such as those cases with a large tumor size with an insufficient hepatic remnant after resection, those cases with extensive and multifocal bilobar tumors or those cases with extrahepatic metastases of the disease. However, in this case report we present a case of palliative hepatectomy for treating advanced HCC with multiple metastases and the patient has had an excellent 1-year follow-up outcome. A 71-year-old man was referred to our hospital and the imaging studies showed a 10 cm mass in the right liver, with multiple variable sized masses in both lungs and a 1 cm nodule in the left adrenal gland. A lung biopsy revealed HCC; therefore, the working diagnosis was HCC with multiple lung metastases and a left adrenal gland adenoma or metastasis. We expected the cause of death would be deterioration of the hepatic function as the liver mass increased in size. Therefore, we performed a palliative right trisectionectomy for the primary liver mass. After recovery from the hepatectomy, the patient was managed with sorafenib. During the 1-year follow-up period after palliative hepatectomy, the patient is still alive with a good general performance status and no evidence of intrahepatic recurrence, even though there has been an aggravation of the lung metastases in size and number, and a slight increase in the size of the left adrenal gland. We suggest that in highly selected patients with advanced HCC and multiple extrahepatic metastases, and especially in the cases involving a large HCC with mild liver cirrhosis and a good general performance status, an aggressive treatment strategy with palliative hepatectomy can be an optional treatment modality to improve the overall survival.
Jae-myeong Lee, M.D.1, Kwang- Min Park, M.D., Ph.D.2, Julian Choi, M.D.2, Sang-Hoon Chon, M.D.2, Dae Wook Hwang, M.D.2, Young-Joo Lee, M.D.2
1Department of Surgery, Ajou
University School of Medicine, Division of Hepato-Biliary & Pancreas Surgery,
2Department of Surgery, University of Ulsan College of Medicine, Asan Medical Center
Corresponding Author Kwang-Min Park
Division of Hepato-Biliary & Pancreas Surgery, Department of Surgery, University of Ulsan College of Medicine, Asan Medical Center, 86,
Asanbyeongwon-gil, Songpa-gu, Seoul 138-736, Korea
Tel: +82-2-3010-3493 Fax: +82-2-3010-6701 E-mail: kmpark@amc.seoul.kr
Key Words : Hepatocellular carcinoma, Metastasis, Palliative treatment, Hepatectomy
Received: 2009. 9. 2 Accepted: 2009. 12. 4
INTRODUCTION
Only 10∼30% of hepatocellular carcinomas (HCCs) are amenable to curative surgical resection at the time of diagnosis.1 Most HCC patients are diagnosed in advanced stages and cannot be given optimal radical treatment.2 Therefore, the prognosis of HCC is poor and depends on the stage of the tumor and the degree of liver function
impairment induced either by the tumor itself or by the underlying cirrhosis.3
The general criteria for HCC unresectability commonly utilized by surgeons include large tumor size with an insufficient hepatic remnant after resection, extensive and multifocal bilobar tumors, and extrahepatic metastases.1 For HCC not suitable for curative treatment, non-surgical and surgical interventions are available for palliative care.4,5 Several methods of surgical treatments for unresectable
HCC have been introduced, such as cytoreductive surgery (also termed tumor debulking, tumor mass reduction, volume reduction, or reductive surgery) or salvage surgery.
The purpose of cytoreductive surgery is to remove or destroy all macroscopic tumors, allowing microscopic foci to persist while at the same time preserving as much functional liver tissue as possible, with peri-operative therapy eradicating residual microscopic tumor cells.1,6 Cytoreductive surgery has been shown to prolong survival and provide good symptomatic relief for patients with good surgical risks in non-randomized studies.7-10 Salvage surgery after successful downstaging has also been reported to provide long-term control of disease in a small proportion of patients with unresectable HCC.1,11
However, palliative hepatectomy, in which macroscopic residual tumor in the liver or other metastatic sites persit is not usually performed, and the efficacy of this type of surgery with respect to improving patient survival or providing symptomatic relief, has not been established. We present herein a case of palliative hepatectomy for advanced HCC with multiple metastases with an excellent 1 year follow-up outcome.
CASE REPORT
A 71-year-old man was referred to our hospital for evaluation of a lung mass which was incidentally detected during a regular check-up 1 year ago. The mass was located in the left upper lobe and was a very tiny nodule at the time of first detection. However, the nodule increased in size after a 1 year follow-up period. He complained of a mild cough, with white sputum during the past 4 years, and easy fatigability. He also had a 5 kg weight loss in 2 months. His medical history included pulmonary tuberculosis that was cured after 3 months of medication and hypertension which was being controlled with medications. The physical examination revealed no significant findings. He had a 50-pack-year smoking history. His family history was unremarkable.
The laboratory investigations did not show any signi- ficant abnormalities. His viral markers were positive for hepatitis C virus (HCV) by enzyme-linked immunosorbent assay (EIA). HCV ribonucleic acid (RNA) real-time quanti- tative polymerase chain reaction (RQ-PCR) was 2.3×105 IU/mL (normal range, <30 IU/mL). The tumor marker, alpha-fetoprotein (AFP), was 12.4 ng/μL (normal range, 0
∼7 ng/μL), and protein induced by the vitamin K absence or antagonist II (PIVKA II) test was >2,400 mAU/mL (normal range, <40 ng/mAU/mL).
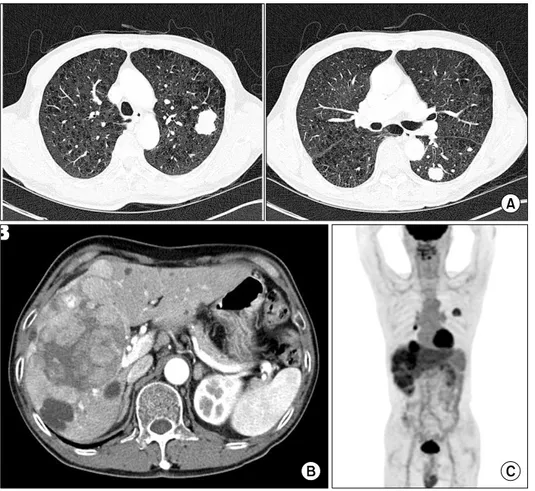
A chest computed tomography (CT) showed multiple nodules of variable size and masses in both lungs, which was suggestive of hematogenous metastases and a large mass in the right liver (Fig. 1A). The liver dynamic CT showed a 10 cm mass thought to be HCC and a 1 cm nodule in the left adrenal gland suggestive of an incidental adenoma or metastasis. There was also enlargement of multiple lymph nodes (LN) around the hepatoduodenal ligament and celiac trunk (Fig. 1B). Fusion whole body positron emission tomography (PET) showed similar findings with CT scan and there was no another lesion, which showed a hypermetabolic activity (Fig. 1C). The nodular lesion in the left adrenal gland showed focal mild hypermetabolic activity (SUVmax=2.4), therefore we could not confirm the lesion to be a metastatic tumor. A lung biopsy was performed to assist with developing a thera- peutic plan. The biopsy revealed HCC.
Although the patient had advanced HCC with multiple metastases, he showed well-compensated hepatic function (Child classification A) and excellent general performance with mild symptoms. However, we expected the hepatic function to decrease in step with the increase in the size of the liver mass. Therefore, we performed a palliative hepatectomy for the primary liver mass.
We performed a right trisectionectomy with LN dissection around the hepatoduodenal ligament. The permanent biopsy revealed diffusely scattered multiple well - demar- cated irregular masses, up to 10×9×8.5 cm in size, with a complete fibrous capsule. The tumor revealed HCC with
Fig. 1. The image findings at the initial time of diagnosis. (A) The chest computed tomography (CT) showed multiple nodules which are suggestive of hematogenous metastases in both lungs. (B) The liver dynamic CT revealed mul- tiple variable-sized masses in the right hepatic lobe and segment IV, suggestive of hepatocellular carci- noma (HCC) with enlargement of multiple lymph nodes around the hepatoduodenal ligament and ce- liac trunk. A 1 cm nodular lesion and thickened left adrenal gland was noted, suggestive of hema- togenous metastasis rather than nodular adrenal hyperplasia. (C) A fusion whole body positron emission tomography (PET) scan showed a hypermetabolic mass or nodular lesions in the right lobe &
S4 of the liver, hepatoduodenal, and portocaval areas, and the left adrenal gland and both lungs, suggestive of HCC with multiple extrahepatic metastases.
5% necrosis and vascular invasion without capsular inva- sion. The Edmonson-Steiner grade was 3/2. The resection margin was clear. There was no tumor invasion to the LNs.
The surrounding liver showed HCV-associated chronic he- patitis and no fatty changes. There were no postoperative complications.
After recovery from the hepatectomy, the patient has been managed with sorafenib (Nexabar, a tyrosine kinase inhibitor of chemotherapeutic agents). During the 1-year follow-up period after palliative hepatectomy, the patient is still alive with good general performance. Even though the imaging study showed aggravation of lung metastases in size and number, and a slightly increased size of the left adrenal gland, there was no evidence of intrahepatic recurrence (Fig. 2).
DISCUSSION
Surgical resection for HCC is recommended for patients who have a single lesion and no evidence of cirrhosis, or cirrhosis with well-preserved liver function, a normal bilirubin level, and a hepatic vein pressure gradient <10 mmHg.12 In the case of unresectable HCC, palliative treat- ments without intent-to-cure, ranging from basic sympto- matic treatment to palliative surgery, radiofrequency abla- tion, alcohol injection, chemoembolization, hormone the- rapy, and systemic chemotherapy, are attempted. The in- dications for these palliative therapies are less well-defined as a consequence of the poor efficiency of each available form of therapy. However, in some cases, palliative therapy can obtain good response rates and even improve survival.2 Extrahepatic metastasis is a common cause of death after resection of the primary liver tumor. Solitary metastasis can
Fig. 2. The CT findings at last follow-up, 1 year after palliative hepatectomy. (A) There was no change in multiple cysts in the liver and no new lesions in other abdominal organs. (B) Several lung nodules in both lungs were of increased size and number, suggestive of aggravation of hem- atogenous metastasis. However, small bilateral mediastinal lymph nodes appeared stable. (C) The nodules in the left adrenal gland showed an increased size from 1 cm to 1.9 cm.
offer a unique opportunity for surgical resection.13 How- ever, most extrahepatic metastases from HCC usually have multiple metastases and can only be offered supportive care or palliative chemotherapy. In a report from Japan, such patients who have undergone symptomatic treatment for extrahepatic metastasis from HCC have not survived for more than 2 years.14 The 1- and 3-year survival rates after development of extrahepatic metastasis in the patients who received treatment in the form of surgery, chemotherapy, radiotherapy, or immunotherapy were 42.3% and 17.8%, respectively.14 Aramaki et al.15 suggested that combined locoregional therapy for intrahepatic recurrence and sys-
temic chemotherapy for extrahepatic metastasis may be effective in prolonging survival in patients with both intra- and extra-hepatic recurrences.
In our case, even with multiple extrahepatic metastases from HCC, the patient had an excellent general perfor- mance with good liver function. The patient and the family members requested aggressive treatment modality. At first, we regarded systemic chemotherapy followed by salvage surgery or systemic chemotherapy with transarterial chemo- embolization as an optimal therapy for our patient. How- ever, we determined that the main cause of death for this patient would be deterioration in liver function along with
the increased tumor mass in the liver prior to multiple lung metastases or severe deterioration in his physical condition.
Moreover, because of portal vein thrombosis or portal flow disturbance due to huge HCC, ascites could occur.
However, if we removed the liver mass, we could resect the entire intrahepatic mass and attempt systemic chemo- therapy after hepatectomy. We also reasoned that the patient would tolerate major hepatectomy with a low rate of possible morbidities, such as postoperative liver failure or respiratory failure associated with anesthesia at that time.
Therefore, we decided to perform palliative right trisection- ectomy for this patient and he recovered postoperatively without complications.
Sorafenib is now considered the standard of care for patients with advanced and metastatic HCC who are not candidates for curative or locoregional therapies.1 Sorafenib tosylate is an oral multikinase inhibitor that blocks tumor cell proliferation by targeting the Raf/mitgen-activated pro- tein kinase/extracellular signal regulated kinase (Raf/MEK/
ERK) signaling pathway and exerts an anti-angiogenic effect by targeting the tyrosine kinases (TKs), VEGF receptor 2 (VEGFR-2), VEGFR-3, and platelet-derived growth factor receptor beta (PDGFR-beta). According to the results of two randomized, double-blind, placebo-controlled, multicentre, phase III trials (the SHARP [Sorafenib HCC Assessment Randomized Protocol] trial and the Asia-Pacific trial), monotherapy with oral sorafenib (400 mg twice daily) prolonged median overall survival compared to the control group (46.3 weeks vs. 34.4 weeks) and delayed the median time to progression in patients with advanced HCC com- pared to the control group (24 weeks vs. 12.3 weeks).1,16 Our patient, who had taken oral sorafenib after palliative hepatectomy for about 1 year, showed progression of multiple pulmonary metastases without intrahepatic recur- rence. We cannot confirm that the excellent prognosis of our patient was due to sorafenib; however, we will continue to prescribe sorafenib for this patient.
Although there was a report of poor survival results (median survival of only 10.7 months) in 10 patients with
intrahepatic recurrences and multiple extrahepatic meta- stases after aggressive locoregional therapy for intrahepatic recurrence and systemic chemotherapy for extrahepatic metastasis,17 we achieved an excellent 1 year follow-up outcome in a patient who underwent palliative hepatec- tomy and oral sorafenib. Of course, we should follow- this patient carefully for detecting progression of metastases or intrahepatic recurrence and check the further prognosis.
However, palliative hepatectomy for advanced HCC, in spite of residual macroscopic extrahepatic metastases, can lead to a good outcome. Therefore, we suggest that palliative surgery is a good treatment modality in highly selected patients, especially in the case of a large HCC with mild liver cirrhosis and good general performance.
In conclusion, we suggest that in highly selected patients with advanced HCC and multiple extrahepatic metastases, an aggressive treatment strategy with palliative hepatectomy may be helpful to improve overall survival.
REFERENCES
1. Lau WY, Lai EC. Hepatocellular carcinoma: current manage- ment and recent advances. Hepatobiliary Pancreat Dis Int 2008;7:237-257.
2. Llovet JM, Burroughs A, Bruix J. Hepatocellular carcinoma.
Lancet 2003;362:1907-1917.
3. Borie F, Bouvier AM, Herrero A, et al. Treatment and prognosis of hepatocellular carcinoma: a population based study in France. J Surg Oncol 2008;98:505-509.
4. Lai EC, Lau WY. The continuing challenge of hepatic cancer in Asia. Surgeon 2005;3:210-215.
5. Lau WY, Yu SC, Lai EC, Leung TW. Transarterial chemoem- bolization for hepatocellular carcinoma. J Am Coll Surg 2006;
202:155-168.
6. McCarter MD, Fong Y. Role for surgical cytoreduction in multimodality treatments for cancer. Ann Surg Oncol 2001;
8:38-43.
7. Lau WY, Leung TW, Leung KL, et al. Cytoreductive surgery for hepatocellular carcinoma. Surg Oncol 1994;3:161-166.
8. Nagashima J, Okuda K, Tanaka M, Sata M, Aoyagi S.
Prognostic benefit in cytoreductive surgery for curatively unresectable hepatocellular carcinoma - comparison to trans- catheter arterial chemoembolization. Int J Oncol 1999;15:
1117-1123.
9. Inman JL, Kute T, White W, Pettenati M, Levine EA. Absence of HER2 overexpression in metastatic malignant melanoma.
J Surg Oncol 2003;84:82-88.
10. Lai EC, Tang CN, Ha JP, Tsui DK, Li MK. Cytoreductive surgery in multidisciplinary treatment of advanced hepato- cellular carcinoma. ANZ J Surg 2008;78:504-507.
11. Lau WY, Lai EC. Salvage surgery following downstaging of unresectable hepatocellular carcinoma--a strategy to increase resectability. Ann Surg Oncol 2007;14:3301-3309.
12. Bruix J, Sherman M; Practice Guidelines Committee, American Association for the Study of Liver Diseases.
Management of hepatocellular carcinoma. Hepatology 2005;
42:1208-1236.
13. Pandey D, Tan KC. Surgical resection of adrenal metastasis from primary liver tumors: a report of two cases. Hepato-
biliary Pancreat Dis Int 2008;7:440-442.
14. Imamura I. Prognostic efficacy of treatment for extrahepatic metastasis after surgical treatment of hepatocellular carci- noma. Kurume Med J 2003;50:41-48.
15. Aramaki M, Kawano K, Kai T, et al. Treatment for extra- hepatic metastasis of hepatocellular carcinoma following suc- cessful hepatic resection. Hepatogastroenterology 1999;46:
2931-2934.
16. Keating GM, Santoro A. Sorafenib: a review of its use in advanced hepatocellular carcinoma. Drugs 2009;69:223-240.
17. Poon RT, Fan ST, O'Suilleabhain CB, Wong J. Aggressive management of patients with extrahepatic and intrahepatic recurrences of hepatocellular carcinoma by combined resec- tion and locoregional therapy. J Am Coll Surg 2002;195:
311-318.