148
The Usefulness of Intracoronary Electrocardiography during Primary Percutaneous Coronary Intervention in
Patients with Acute Myocardial Infarction
Woong Kim, MD1, Young-Jo Kim, MD1, Sang-Hee Lee, MD1, Hyong-Jun Kim, MD2, Geu-Ru Hong, MD1, Jong-Seon Park, MD1, Dong-Gu Shin, MD1 and Bong-Sup Shim, MD1
1Division of Cardiology, Department of Internal Medicine, Yeungnam University Medical Center, Daegu,
2Department of Internal Medicine, Dong Kang Hospital, Ulsan, Korea
ABSTRACT
Background and Objectives:Measurements obtained using an intracoronary electrocardiogram (IC-ECG) reflect the electrical activity in various regions of the myocardium. This technique can be easily used in the catheterization laboratory during percutaneous coronary intervention (PCI) procedures. Furthermore, IC-ECG could be used to evaluate myocardial viability in patients with acute myocardial infarction (AMI). The aim of this study was to eva- luate the usefulness of IC-ECG in predicting the microvascular integrity and late improvement of left ventricular (LV) function after primary PCI in patients with AMI. Subjects and Methods:A total of 78 patients (62 male, 16 female) who underwent primary PCI with stent implantation were enrolled in this study. After the implantation of the stent, IC-ECG was recorded from the tip of an insulated angioplasty guidewire before and after balloon oc- clusion of the infarct-related artery. The IC-ECG was obtained from the inferior and inferolateral areas in inferior wall MI, or apex and apical anterior wall regions in anterior wall MI. Significant ST segment elevation was defined as a further ST segment elevation of ≥0.2 mV at 80 msec after the J-point in comparison to the baseline value. The microvascular integrity of the myocardium was evaluated by myocardial contrast echocardiography (MCE) one day after the PCI was performed. Six months later, all of the patients were followed up by echocardiography and the wall motion score index (WMSI) and ejection fraction (EF) were measured. Results:Significant ST elevation was no- ted in 47 patients (Group A) after coronary occlusion. There was no significant change in the other 31 patients (Group B). MCE showed microvascular perfusion in 41 patients in group A (87%) and in four patients in group B (13%) (p<0.05). The six-month follow-up echocardiography showed that group A had a lower WMSI (1.20±0.18 vs 1.56±0.34, p<0.05) and higher EF (57.6±7 vs 47±11, p<0.05) than group B. The LV end diastolic dimension (LVEDD) in group B was increased compared to group A (p=0.021). The LV end systolic dimension (LVESD) was also increased in group B; however, the LVESD in group A was decreased after six months (p=0.002). Conclusion:
IC-ECG during PCI is a simple and useful method for assessing the microvascular integrity of the myocardium and for predicting the long-term improvement of LV function. (Korean Circulation J 2007;37:148-153)
KEY WORDS:Myocardial infarction;Ventricular function;Electrocardiography.
Introduction
Differentiating viable myocardium from necrotic tis- sue in patients with acute myocardial infarction(MI) has
both prognostic and therapeutic significance, especially when a revascularization procedure is being considered.1-3) The identification of nonviable myocardium during per- cutaneous coronary intervention(PCI) in the catheteri- zation laboratory provides additional information that can be used to guide the procedure and subsequent pa- tient follow-up.
Intracoronary ECG(IC-ECG) was first developed by Meier et al.,4) Meier and Rutishauser,5) and Friedman.6) IC-ECG determines the regional myocardial electrical ac- tivity and can easily detect myocardial ischemia during PCI with greater sensitivity than surface ECG.6-9) IC-
Received:January 12, 2007 Revision Received:February 2, 2007 Accepted:February 9, 2007
Correspondence:Young-Jo Kim, MD, Division of Cardiology, Department of Internal Medicine, Yeungnam University Medical Center, 317-1 Dae- myong-dong, Nam-gu, Daegu 705-717, Korea
Tel: 82-53-621-3310, Fax: 82-53-620-3313 E-mail: yjkim@med.yu.ac.kr
ECG has been used as a tool for detecting myocardial viability.10) Myocardial contrast echocardiography(MCE) has emerged as a relatively new and non-invasive echo- cardiographic tool for the assessment of myocardial per- fusion. MCE is another useful method for assessing mi- crovascular integrity and myocardial viability in patients with MI.11-13)
We hypothesized that if the local myocardium were via- ble after MI, the ST segment on the IC-ECG would be elevated from the baseline value. Based on the data col- lected on the IC-ECG, we evaluated the viable myocar- dium as determined by MCE, and used echocardiogra- phy to compare the left ventricular(LV) function between two groups after six months. The goal was to determine whether IC-ECG could be used to assess the microvas- cular integrity of the myocardium during the acute phase of MI, and to predict the improvement of LV function at a later date after the MI.
Subjects and Methods Population and study protocol
A total of 78 patients(62 male, 16 female) with acute ST segment elevation MI who were referred to our ca- theterization laboratory for primary PCI within 12 hours of symptom onset between March 2005 and January 2006 were enrolled in this study. The diagnosis of acute MI was based on the presence of ischemic chest pain lasting >30 minutes, ST elevation ≥0.1 mV in ≥2 con- tiguous leads on standard ECG and a ≥three-fold in- crease in serum levels of creatine kinase. All patients un- derwent coronary angiography within 60 minutes of admission. The coronary angiography was then followed by stenting of the infarct-related artery(IRA). The exclu- sion criteria included: contraindication to the coronary angiogram, >50% stenosis in the left main coronary artery, >75% stenosis in another major coronary artery, prior MI, cardiogenic shock, cardiomyopathy, and right or left bundle branch block detected on the ECG. Each patient provided written informed consent prior to ca- theterization in accordance with the hospital guidelines.
Echocardiography was performed prior to PCI and MCE was performed one day after the PCI. All patients were followed up with echocardiography six months after PCI in order to measure the wall motion score index(WMSI) and ejection fraction(EF).
Coronary angiography and angioplasty
All patients received an intravenous bolus injection of 5000 U of heparin, and 5 mg/h of isosorbide dinitrate was continuously administered intravenously soon after the diagnosis was established. Emergency coronary an- giography was performed by the femoral approach accor- ding to the standard procedure. An insulated angioplasty guidewire(Wizdom, Cordis, USA) was placed at the distal
portion of the target coronary artery. The guidewire ser- ved as a unipolar electrode placed distal to the lesion.
The external end was connected to the chest lead termi- nal of a CardioLab® system(Prucka Engineering, Inc.
USA) using an alligator clamp. The surface and IC-ECGs were simultaneously recorded on the CardioLab® system.
The initial dilatation was performed with an angiopla- sty balloon catheter of small diameter(2.0 mm) to recana- lize and obtain a Thrombolysis in Myocardial Infarction (TIMI) grade 3 flow prior to conducting the study. The baseline level was defined as the ST segment level on the IC-ECG following the improvement of the reperfu- sion arrhythmia and injury. The IC-ECG and balloon occlusion were recorded in regular sequence ten minutes after the stent implantation.
The balloon diameters used for occlusion were chosen according to the stent size and a short balloon, usually less than 15 mm, was used in all patients. The balloon pressure could not be elevated over 6 atmospheres. Each patient’s balloon was inflated for 120 sec. The IC-ECG was obtained from the inferior and inferolateral wall in cases of inferior wall MI and from the apex and apical anterior wall in cases of anterior wall MI.
Any further ST segment elevation greater than 0.2 mV on the IC-ECG occurring during the balloon occlu- sion inflation was considered to be a significant change.
All ST segment deviations were measured manually at 80 ms after the J-point using the PR interval as the iso- electric point of reference.
Echocardiography
All patients underwent a complete transthoracic study before PCI, which included the analysis of images taken from multiple viewpoints using a commercially available imaging system(Vivid 7, GE Healthcare, USA). Systolic wall thickening and inward wall motion were visually assessed offline by two experienced operators. Investiga- tors who were blinded to the results of the intracoronary and surface electrocardiograms interpreted the results of the echocardiograms. Three apical views(four- and two-chamber and long axis) were analyzed, and the left ventricle was divided into 16 segments. A four point segmental wall motion scoring system was used(1, nor- mal; 2, hypokinesis; 3, akinesis; 4, dyskinesis). Each zone included nine segments, and the apical inferior and api- cal-lateral segments were considered to be overlapping segments. The infarct zone WMSI was obtained by ave- raging the sum of the scores of all of the visualized seg- ments in the infarct zone divided by the number of the scored segments. Biplane measurements of LV volumes and EF were also obtained as previously reported.14) Myocardial contrast echocardiography(MCE)
MCE was performed using perfluorocarbon-enhan- ced sonicated dextrose albumin(PESDA) as the contrast
agent.15) After the onset of biplane echocardiography, 60 mL of saline was mixed with 40 mL of PESDA and the mixed fluids were then slowly infused intravenously at a rate of 1 mL/min in order to examine uniformly per- fused myocardium by microbubbles. High-energy ultra- sound was injected to eliminate microbubbles in the myocardium. The refilling pattern of the microbubbles in the myocardial wall was examined and recorded by S-VHS video. The refilling pattern of the microbubbles was analyzed in the apical four-chamber view, the apical three-chamber view and the apical two-chamber view and the presence of reperfusion was evaluated in each view.
Myocardial reperfusion abnormalities were identified when microbubbles did not refill through the tenth end- systole after the removal of the high-energy ultrasound.
MCE was performed using a digital ultrasound system (Vivid 7, GE Healthcare, USA) and real time MCE was performed using low mechanical index Power Modula- tion imaging(MI<0.1). The optimal gain was adjusted to the best level prior to the examination and was main- tained at that level throughout the examination.16) Statistical analysis
Statistical analysis was performed using SPSS 12.0 for Windows(SPSS Inc. Chicago, Illinois, USA). All quan- titative data are presented as the means±standard devia- tion. A paired t-test was used to compare the recorded variables within the same group, while the unpaired t- test was used to compare another group[AH3]. Statistical significance was defined at p<0.05.
Results Patient characteristics
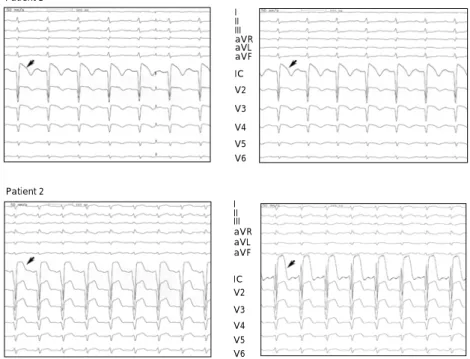
Emergency angiography revealed that 47 patients(61%) had significant ST segment elevation as shown in Fig. 1- patient 2(group A), and that there were 31 patients(39%) who did not have significant ST segment elevation(Fig. 1) (patient 1, group B). The patient characteristics for the two groups are summarized in Table 1. There were no significant differences with regard to age, gender, diabe- tes, hypertension, smoking and dyslipidemia. However, the peak creatine kinase, MB levels were greater in group B than in group A(p=0.012). LVEF was greater in group
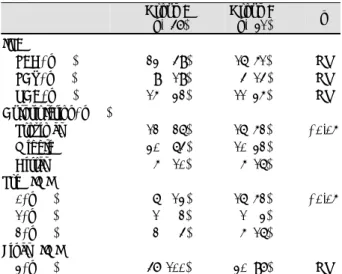
Table 1.Comparison of the baseline characteristics between the two groups
Group A (n=47)
Group B
(n=31) p
Age (years) Male, n (%) HTN, n (%) DM, n (%) Dyslipidemia, n (%) Smoking, n (%) Peak CK-MB (ng/mL) LVEF (%)
WMSI
Onset to balloon time (hr) Door to balloon time (min)
.057±140 38 (81) 20 (43) 16 (34) 19 (40) 31 (66) .119±123 .051 ±700 1.35±0.2 04.6±300 0.83±170
058±100.
24 (77) 11 (35) 10 (32) 12 (39) 17 (55) 204±182 .046±800 1.55±0.3 04.8±20.
.085±16.
NS NS NS NS NS NS
<0.05
<0.05
<0.05 NS NS HTN: hypertension, LVEF: left ventricular ejection fraction, WMSI:
wall motion score index, DM: diabetes mellitus, CK-MB: creatine ki- nase-MB
Patient 1
Baseline
I II III aVR aVL aVF
IC V2 V3 V4 V5 V6
Patient 2 I
II III aVRaVL aVF IC V2 V3 V4 V5 V6
Balloon occlusion
III III aVR aVLaVF
IC V2 V3 V4 V5 V6
III III aVRaVL aVF
IC V2 V3 V4 V5 V6
Fig. 1. Significant and insignificant ST segment changes in the intracoronary ECG (IC-ECG) during percutaneous coronary intervention. In patient 1, baseline IC-ECG was recorded but no significant ST changes were found following balloon occlusion. In patient 2, a significant ST segment eleva- tion over 0.2 mV was noted after balloon occlusion. Arrow head indicates ST segment changes. ECG: electrocardiogram, IC: intracoronary.
A than in group B(p=0.034). WMSI was greater in group B than in group A(p=0.013). The pain onset to balloon time and door to balloon time were not statis- tically different between the two groups(Table 1).
Angiographic findings
Table 2 shows the features observed during coronary angiogram in the two groups. There were no differences in the IRA or final TIMI 3. However, significant diffe- rences were found in the culprit lesions and the pre TIMI score: group B had more proximal lesions(p=0.001) and lower pre-TIMI scores than group A(p=0.004).
Results of MCE
The sensitivity and specificity of IC-ECG and its re- lationship to the findings of microvascular perfusion are shown in Table 3. The IC-ECG had an 87% sensitivity and specificity.
In-hospital and out-of-hospital prognosis
There was no difference in the frequencies of recur- rent MI, restenosis or death between the two groups (Table 4). Two patients in group A and one patient in group B showed target lesion restenosis at the six-month angiographic follow-up following PCI. Although one pa- tient did show restenosis on the coronary angiogram at
six months after PCI, this patient had no symptoms of ischemia and showed no evidence of ischemia in the non-invasive test. Therefore, revascularization was not performed. However, PCI was performed in two patients.
There were no cases of recurrent MI nor of in-hospital or out-of-hospital death.
Left ventricular function by echocardiography six months after PCI
The differences in LV function according to TTE were compared between the two groups six months after PCI and the results are shown in Table 4. Group A showed greater improvement in LV function than group B: group A had a decreased WMSI(p=0.002) and an increased LVEF(p=0.007) compared to group B. The LV end diastolic dimension(LVEDD) in group B was greater than that of Group A(p=0.021), and the LV end systolic dimension(LVESD) in group B was increased;
however, the LVESD in group A decreased after six months(p=0.002).
Table 2. Comparison of the angiographic findings between the two groups
Group A (n=47)
Group B
(n=31) p
IRA
LAD, n (%) LCX, n (%) RCA, n (%)
23 (049) 09 (019) 15 (032)
16 (51) 04 (14) 11 (35)
NS NS NS Culprit lesion, n (%)
Proximal Middle Distal
12 (026) 30 (064) 05 (010)
16 (52) 10 (32) 05 (16)
<0.05
Pre TIMI 0, n (%) 1, n (%) 2, n (%) Final TIMI
3, n (%)
06 (013) 01 (002) 02 (004) 47 (100)
16 (52) 01 (03) 05 (16) 30 (97)
<0.05
NS TIMI: Thrombolysis in myocardial infarction, IRA: Infarc-related ar- tery, LAD: left anterior descending artery, LCX: left circumflex artery, RCA: right coronary artery
Table 3. A comparison of the myocardial contrast echocardiogram (MCE) findings between the two groups
Group A (ST change)
Group B (no ST change) Microvascular perfusion +, n (%)
Microvascular perfusion -, n (%)
41 (87%) 06 (13%)
04 (13%) 26 (87%)
Total 47 31
Intracoronary ECG. Sensitivity=87%, Specificity=87%, ECG: elec- trocardiogram
Table 4.A comparison of the six-month follow-up echocardiographic findings between the two groups
Group A (n=47)
Group B
(n=31) p
LVEDD (mm) Baseline 6 Mo (F/U) Difference LVESD (mm) Baseline 6 Mo (F/U) Difference WMSI
Baseline 6 Mo (F/U) Difference
.-48±40.
.-48±40.
-0.4±4.2 .-35±40.
.-33±50.
-1.4±4.7 -1.352±0.230
-1.198±0.180 0-0.15±0.150
048±50 051±50 02.8±5.9
036±50 039±60 02.8±4.9 1.545±0.34 1.557±0.34 0.012±0.25
0.021
0.002
0.002 EF (%)
Baseline 6 Mo (F/U) Difference
-51±70 -57±70 0-6±70
0.46±800 0.47±110
0.24±100 0.007 WMSI: wall motion score index, F/U: follow up, EF: ejection fraction, LVEDD: left ventricular end diastolic dimension, LVESD: left ventri- cular end systolic dimension
Table 5.A comparison of the six-month follow-up morbidity and mor- tality between the two groups
Group A (n=47) Group B (n=31) p Recurrent MI
Restenosis Revascularization InHspt death OutHspt death
2 2 1 0 0
0 1 1 0 0
NS NS NS NS NS
Total 5 2 NS
MI: myocardial infarction, Restenosis: >50% diameter stenosis on co- ronary angiogram 6 month after PCI, InHspt: in hospital, OutHspt:
out of hospital, PCI: percutaneous coronary intervention
Discussion
Acute ST elevation myocardial infarction(STEMI) is a critical condition that requires prompt and accurate treatment. Time is one of the most important factors in the successful treatment of STEMI. Early reperfusion al- lows the residual myocardium to survive, which prevents mechanical and electrical complications that can develop from an acute MI. Therefore, the occluded coronary ves- sel must be recanalized and treated as soon as possible.
It is important to consider the amount of viable myo- cardium because residual myocardium determines long- term LV function and survival. Therefore, the detection of viable myocardium is useful for post-myocardial risk stratification and patient prognosis. Several diagnostic tools for the detection of viable myocardium are employed such as thallium-201 myocardial scintigrams,17)18) dobuta- mine stress echocardiography,19)20) myocardial contrast echocardiography21)22) and positron emission tomography.
However, imaging studies cannot adequately distinguish between infarcted, irreversibly damaged and stunned or hibernating myocardium. In addition, each of these te- chniques can only be performed during the post-infarc- tion time period. No studies have been easily performed during PCI. Therefore, IC-ECG is likely to be a very useful method for validating myocardial viability.
A patient’s prognosis can be predicted based on the detection of viable myocardium by IC-ECG, and the prognosis of STEMI is closely correlated with LV func- tion, which can be predicted by the detection of viable myocardium. Both short term and long term survival after STEMI depend on three factors: resting LV func- tion, residual potentially ischemic myocardium and sus- ceptibility to serious ventricular arrhythmias. The most important of these factors is the state of LV function.23) Therefore, IC-ECG can be used to predict long-term LV function.
In this study, we found good correlation between ST elevation detected on IC-ECG during balloon occlusion performed during the acute stage and an improvement in LV function by echocardiography at the chronic stage.
The sensitivity and specificity of significant ST elevation on the IC-ECG performed during PCI to assess viability based on the MCE, and the improvement of LVEF and WMSI on TTE at six months after PCI were very high.
Therefore, IC-ECG may provide a very useful method for validating myocardial viability.
The peak CK-MB was significantly higher in patients in group B during PCI and in cases of culprit lesions and pre-TIMI 0: group B had more proximal and pre-TIMI 0 lesions than group A.
Patients with TIMI 0 have a totally occluded coronary artery and must have a larger infarct area or severe re- perfusion injury. Furthermore, the remaining viable myo- cardium is smaller in patients with TIMI 0 than in
patients with high-grade TIMI scores. These findings were significant in patients with no significant ST seg- ment elevation.
Therefore, the presence of significant ST segment ele- vation on the IC-ECG suggested the presence of viable myocardium. Our findings showed that IC-ECG can detect viable myocardium, and could therefore be used as a prognostic tool. Measurements can be easily perfor- med in the catheterization laboratory during PCI. Ag- gressive unloading therapy may be provided in cases where the IC-ECG shows no significant ST segment ele- vation. The variables affecting the results of the IC-ECG including more proximal site, TIMI 0 flow[AH4], were interrelated, which might be affect the results of the IC- ECG. However, we can only predict the fate of the myo- cardium diffusely about whether myocardium is alive or not[AH5]. In this situation, IC-ECG can provide addi- tional information regarding the viable myocardium and prognosis with high sensitivity and specificity.
This study had several limitations. Our analysis fol- lowed patients for six months, which is a relatively short period of time. The survival and quality of life over a longer period of time should be taken into consideration in future studies. Another limitation of our study was that we did not consider the impact of collateral chan- nels during balloon occlusion. The opening of the col- lateral vessels with severe coronary artery stenosis during PCI might have obscured the ST segment changes in the IC-ECG during the occlusion of the IRA. However, there was no angiographic evidence of preexisting col- lateral circulation in any of the patients studied, but the possibility remains that collateral circulation could have confounded the results. Another limitation of our study was that although the guidewire was positioned at the most distal part of the vessel, it was not possible to cover all corresponding regions of interest with the guidewire.
This may have resulted in discordant findings and may have introduced a certain degree of error in the assess- ment of myocardial viability based on the ST elevation.
It is possible that our results underestimated the diag- nostic accuracy of IC-ECG. It is also possible that bal- loon occlusion for IC-ECG itself might affect the peak CK-MB level. However, the effects of short balloon time and low pressure could be small and may not have alte- red our results from the IC-ECG.
In conclusion, IC-ECG during PCI is a simple and useful method for assessing the microvascular integrity of the myocardium and for predicting the long-term im- provement of LV function in patients with acute MI.
REFERENCES
1) Rahimtoola SH. The hibernating myocardium. Am Heart J 1989;
117:211-21.
2) Huitink JIM, Visser FC, Bax JJ, Visser CA. Detection of viability after myocardial infarction: available techniques and clinical re-
levance-a review. Int J Cardiol 1995;51:253-66.
3) Abaci A, Oguzhan A, Topsakal R, et al. Intracoronary electrocar- diogram and angina pectoris during percutaneous coronary in- terventions as an assessment of myocardial viability: comparison with low-dose dobutamine echocardiography. Catheter Cardio- vasc Interv 2003;60:469-76.
4) Meier B, Killisch JP, Adatte JJ, Casalini P, Rutishauser W. Intra- koronares elektrokardiogram warend transluminaler koronaran- gioplastie. Schweiz Med Wochenschr 1985;115:1590-3.
5) Meier B, Rutishauser W. Coronary pacing during percutaneous transluminal coronary angioplasty. Circulation 1985;71:557-61.
6) Friedman PL, Shook TL, Kiershenbaum JM, Selwyn A, Ganz P.
Value of the intracoronary electrocardiogram to monitor myocar- dial ischemia during percutaneous transluminal coronary angio- plasty. Circulation 1986;74:330-9.
7) Pande AK, Meier B, Urban P, Moles V, Dorsaz PA, Farve J.
Intracoronary electrocardiogram during coronary angioplasty. Am Heart J 1992;124:337-41.
8) Piessens J, Vrolix M, Sionis D, Glazier JJ, De Geest H, Willems J. The value of the intracoronary electrogram for the early detec- tion of myocardial ischemia during coronary angioplasty. Eur Heart J 1991;12:1176-82.
9) Saito S, Watanabe I, Hibiya K, et al. Intracoronary ST-segment alternans during coronary balloon angioplasty. Jpn Heart J 1998;
39:221-4.
10) Yajima J, Saito S, Honye J, Takayama T, Ozawa Y, Kanmatususe K. Intracoronary electrocardiogram for early detection of myo- cardial viability during coronary angioplasty in acute myocardial infarction. Int J Cardiol 2001;79:293-9.
11) Ahn JC, Shim WJ, Rha SW, et al. Myocardial reperfusion and long-term change of left ventricular volume after acute anterior wall myocardial infarction. Korean Circ J 1997;27:1138-46.
12) Shim WJ. Assessment of myocardial perfusion by myocardial con- trast echocardiography. Korean Circ J 2001;31:285-9.
13) Aggeli C, Theocharis C, Bonou M, Stefanadis C. Contrast echo- cardiography: a new method for the assessment of myocardial perfusion in coronary artery disease. Hellenic J Cardiol 2003;
44:400-7.
14) Lang RM, Bierig M, Devereux RB, et al. Recommendations for chamber quantification: a report from the American Society of
Echocardiography’s guidelines and standards committee and the chamber quantification writing group, developed in conjuction with the European Association of Echocardiography, a branch of the European Society of Cardiology. J Am Soc Echocardiogr 2005;
18:1440-63.
15) Porter TR, Xie F, Kricsfeld D, Armbruster RW. Improved myocar- dial contrast with second harmonic transient ultrasound response imaging in humans using intravenous perfluorocarbon-exposed sonicated dextrose albumin. J Am Coll Cardiol 1996;27:1497-501.
16) Min PK, Jung JH, Kang WC, et al. The role of myocardial con- trast echocardiography in acute chest pain without ST elevation.
Korean Circ J 2003;33:284-93.
17) Bonow RO, Dilsizian V, Cuocolo A, Bacharach SL. Identification of viable myocardium in patients with chronic coronary artery disease and left ventricular dysfunction: comparison of thallium scintigraphy with reinjection and PET imaging with 18F-fluoro- deoxyglucose. Circulation 1991;83:26-37.
18) Marin-Neto JA, Dilsizian V, Arrighi JA, et al. Thallium reinjection demonstrates viable myocardium in regions with reverse redistri- bution. Circulation 1993;88:1736-45.
19) Pierard LA, De Landsheere CM, Berthe C, Rigo P, Kulbertus HE.
Identification of viable myocardium by echocardiography during dobutamine infusion in patients with myocardial infarction after thrombolytic therapy: comparison with positron emission tomo- graphy. J Am Coll Cardiol 1990;15:1021-31.
20) Watada H, Ito H, Oh H, et al. Dobutamine stress echocardiogra- phy predicts reversible dysfunction and quantitates the extent of irreversibly damaged myocardium after reperfusion of anterior myocardial infarction. J Am Coll Cardiol 1994;24:624-30.
21) Ragosta M, Camarano G, Kaul S, Powers ER, Sarembock IJ, Gimple LW. Microvascular integrity indicates myocellular viabi- lity in patients with recent myocardial infarction: new insights using myocardial contrast echocardiography. Circulation 1994;
89:2562-9.
22) Ito H, Maruyama A, Iwakura K, et al. Clinical implications of no reflow phenomenon: a predictor of complications and left ventri- cular remodeling in reperfused anterior wall myocardial infarction.
Circulation 1996;93:223-8.
23) Zipes. Braunwald’s Heart Disease: a textbook of cardiovascular medicine. 7th ed. Philadelphia: W.B. Saunders; 2005. p.1216-8.