저작자표시-비영리-변경금지 2.0 대한민국 이용자는 아래의 조건을 따르는 경우에 한하여 자유롭게 l 이 저작물을 복제, 배포, 전송, 전시, 공연 및 방송할 수 있습니다. 다음과 같은 조건을 따라야 합니다: l 귀하는, 이 저작물의 재이용이나 배포의 경우, 이 저작물에 적용된 이용허락조건 을 명확하게 나타내어야 합니다. l 저작권자로부터 별도의 허가를 받으면 이러한 조건들은 적용되지 않습니다. 저작권법에 따른 이용자의 권리는 위의 내용에 의하여 영향을 받지 않습니다. 이것은 이용허락규약(Legal Code)을 이해하기 쉽게 요약한 것입니다. Disclaimer 저작자표시. 귀하는 원저작자를 표시하여야 합니다. 비영리. 귀하는 이 저작물을 영리 목적으로 이용할 수 없습니다. 변경금지. 귀하는 이 저작물을 개작, 변형 또는 가공할 수 없습니다.
Magnetic resonance lymphography for
sentinel lymph node detection
in patients with oral cavity cancer:
A preliminary clinical study
Sohi Bae
Department of Medicine
The Graduate School, Yonsei University
[UCI]I804:11046-000000516250
[UCI]I804:11046-000000516250
[UCI]I804:11046-000000516250
Magnetic resonance lymphography for
sentinel lymph node detection
in patients with oral cavity cancer:
A preliminary clinical study
Directed by Professor Jinna Kim
The Doctoral Dissertation
submitted to the Department of Medicine,
the Graduate School of Yonsei University
in partial fulfillment of the requirements for the degree
of Doctor of Philosophy
Sohi Bae
This certifies that the Doctoral
Dissertation of Sohi Bae is approved.
---
Thesis Supervisor : Jinna Kim
---
Thesis Committee Member#1 : Hyung-Jin Kim
---
Thesis Committee Member#2 : Yoon Woo Koh
---
Thesis Committee Member#3: Woong Nam
---
Thesis Committee Member#4: Sun Och Yoon
The Graduate School
Yonsei University
ACKNOWLEDGEMENTS
I acknowledge my deep gratitude to Professor Jinna Kim, who
is my thesis director, for supporting my efforts with total
commitment and facilitating every step of the process. My
appreciation for her guidance and encouragement is
tremendous. I am also indebted to Professor Hyung-Jin Kim,
Woong Nam, Yoon Woo Koh and Sun Och Yoon, for their
help for pertinent advice to assure the superior quality of this
paper.
<TABLE OF CONTENTS>
ABSTRACT ··· 1
I. INTRODUCTION ··· 3
II. MATERIALS AND METHODS ··· 4
1. Patients ··· 4
2. MR lymphography ··· 5
3. Sentinel LN identification and surgery ··· 6
III. RESULTS ··· 7
IV. DISCUSSION ··· 11
V. CONCLUSION ··· 13
REFERENCES ··· 14
LIST OF FIGURES
Figure 1. Result of sentinel LN evaluation in patients with
resectable oral cavity cancer planning elective neck dissection
··· 8
Figure 2. A 38-year-old woman with oral tongue cancer and
palpably negative neck ··· 9
Figure 3. A 71-year-old man with buccal mucosa cancer and
clinically negative neck ··· 10
Figure 4. 51-year-old patient with tongue cancer with metastatic
1
ABSTRACT
Magnetic resonance lymphography for sentinel lymph node detection in patients with oral cavity cancer: A preliminary clinical study
Sohi Bae
Department of Medicine
The Graduate School, Yonsei University
(Directed by Professor Jinna Kim)
Background and Purpose: Identification of sentinel lymph nodes (LNs) is important because sentinel LN biopsy is used as an alternative procedure to elective neck dissection in patients with oral cavity cancer and clinically negative neck. The purpose of this study was to evaluate the feasibility of magnetic resonance (MR) lymphography with interstitial injection of a gadolinium-based contrast agent for identifying sentinel LNs in patients with oral cavity cancer and clinically negative neck.
Methods: A total of 26 patients with resectable oral cavity cancer and clinically negative neck were recruited for this study. After peritumoral injection of 1-ml diluted gadobutrol, pretreatment MR lymphography with Differential Sub-sampling with Cartesian Ordering (DISCO) sequence was performed. The accuracy of sentinel LN identification of MR lymphography was assessed and compared with the final histopathological results after elective neck dissection.
2
Results: MR lymphography consistently visualized the 44 sentinel LNs, defined as the first LNs to show any enhancement at the periphery portion of LNs near the injection site, in all 26 patients. After elective neck dissection, 42 assumed sentinel LNs were obtained in 24 patients, and histopathology revealed that 27 LNs from 11 patients were metastatic. In all but one patient with pathologically positive neck, assumed sentinel LNs revealed metastatic involvement.
Conclusions: Pretreatment MR lymphography is a safe and feasible imaging technique that can help clinicians identify sentinel LNs with a high risk of occult metastases in patients with oral cavity cancer and clinically negative neck, enabling focused preoperative biopsy in these high-risk patients
--- Key words : MR lymphography, oral cavity cancer, sentinel lymph node, lymph node metastasis
3
Magnetic resonance lymphography for sentinel lymph node detection in patients with oral cavity cancer: A preliminary clinical study
Sohi Bae
Department of Medicine
The Graduate School, Yonsei University
(Directed by Professor Jinna Kim)
I. INTRODUCTION
Cervical lymph node (LN) metastasis is the single most important prognostic factor in oral cavity squamous cell carcinoma, and accurate detection of cervical LN metastases is critical for surgical and adjuvant therapy planning, and prognosis prediction.1 However, currently available imaging techniques are
not sufficiently sensitive to detect cervical LN metastases, resulting in a high incidence rates (20–60%) of occult metastases.2 Therefore, elective neck
dissection, which is the standard treatment in patients with oral cavity cancer and clinically negative neck, is effective in only 20–60% of patients with occult LN metastases, with the remaining 40–80% requiring avoidable surgery that results in high morbidity and costs.
Several studies have validated the accuracy and efficacy of sentinel LN biopsy in patients with oral cavity cancer, and reported its high sensitivity and negative predictive value, which results in lower morbidity and costs relative to elective neck dissection.2-6 Accordingly, in institutions where it is available,
4
sentinel LN biopsy is considered a viable alternative to elective neck dissection for the identification of occult cervical metastasis in patients with early oral cavity cancer, in accordance with the 2017 National Comprehensive Cancer Network Clinical Practice Guidelines.7
Magnetic resonance (MR) lymphography is a technique that employs MR imaging after interstitial injection of extracellular gadolinium chelates to identify sentinel LNs. Recent studies in cancer patients and with animal models have shown the safety and utility of this technique.8-11 MR lymphography
provides detailed information of the sentinel LN and surrounding anatomy with high spatial resolution. Radioisotopes and blue dye, which are commonly used to localize sentinel LNs during surgery, have inherent limitations such as low spatial resolution, limited availability during surgery, and radiation exposure.12
Therefore, the purpose of this study was to evaluate the feasibility of MR lymphography using interstitial injection of a gadolinium-based contrast agent for detecting sentinel LNs in patients with oral cavity cancer and clinically negative neck.
II. MATERIALS AND METHODS 1. Patients
This study was approved by the institutional review board of our hospital, and written informed consent was obtained from all patients. Between November 2015 to March 2017, we recruited 37 consecutive patients with newly diagnosed resectable oral cavity squamous cell carcinoma and clinically negative cervical LN confirmed by physical examination and conventional computed tomography (CT) imaging. We excluded four patients with multiple primary tumors, previous head and neck cancer history, or prior neck dissection, and seven patients in whom MR imaging was contraindicated or who refused to undergo additional MR examination. Thus, 26 patients (19 men, 7 women; mean age: 60.7 years; range: 36–82 years) were included in this study. The
5
primary tumor sites were the oral tongue (n = 17), buccal mucosa (n = 3), alveolar ridge (n = 4), and floor of the mouth (n = 2). The median tumor size was 2.2 cm (range: 1.0–4.6 cm), with 6 T1 tumors, 11 T2 tumors, 6 T3 tumors and 3 T4a tumors, according to the 8th edition of the American Joint Committee on Cancer (AJCC) staging system for head and neck cancer.13
2. MR lymphography
MR imaging was performed on a 3.0-Tesla system (Discovery MR750; GE Medical Systems, Milwaukee, WI, USA) with a 6-channel carotid coil. Each patient assumed a supine position with a foam support under the neck as an immobilization aid. Before the administration of contrast agent, conventional MR images consisting of spin-echo T1-weighted and fat-saturated fast spin-echo T2-weighted images were obtained in the transverse and coronal planes according to our routine protocol for the head and neck with a repetition time/echo time (TR/TE) of 640 ms/10 ms and 2000 ms/70 ms, respectively. All images were obtained with a 22–25-cm field of view (FOV), which was adjusted for each patient.
Gadobutrol (Gadovist; Bayer Healthcare Pharmaceuticals, Whippany, NJ, USA) was injected interstitially and intravenously. Previously used contrast agents on MR lymphography were various, including gadopentetate dimeglumine, gadoteridol, gadoterate meglumine, gadodiamide and gadobutrol. Gadobutrol was chosen in our study because it was cyclic agent with relatively low osmolality among the currently used contrast agents in our institution. For interstitial injection, gadobutrol was diluted with sterile water and 2% lidocaine (0.3:1:0.2 contrast agent:water:lidocaine). The mixture proportion of diluted contrast was based on the result of the previously reported experiment.14 After
topical application of viscous lidocaine, a total 1 ml of diluted contrast agent was injected using a 1 ml tuberculin syringe and 30-guage needle at four peritumoral sites. The injection site was gently massaged for 30 seconds to
6
promote the migration of contrast agent.
MR lymphography was performed using a Differential Subsampling with Cartesian Ordering (DISCO) sequence with the following parameters: a FOV, 220 mm; matrix, 224 × 224; slice thickness, 1 mm; TR/TE, 4.4 ms/1.7 ms; and flip angle, 15°. Ten dynamic phases were acquired with a total acquisition time of 2 minutes 50 seconds. In addition, a liver acquisition with volume acceleration flex (LAVA-Flex) sequence, which is a 3D gradient dual echo imaging technique in which a second echo acquisition is added immediately after the first echo, was obtained with a two-point Dixon reconstruction to confirm the delayed enhancement of LNs with the following parameters: FOV, 220 mm; matrix, 224 × 224; slice thickness, 1mm; TR/TE, 5.0 ms/2.0 ms; and flip angle, 15°. Two phases were acquired with a total acquisition time of 2 minutes 20 seconds.
Then, gadobutrol was administered intravenously at a dose of 0.1 mL/kg body weight and a rate of 2 mL/s, and 40 seconds later, axial fat-saturated spin-echo T1-weighted images were acquired sequentially. Subjects were closely monitored for adverse reactions for 2 hours after contrast administration, and all adverse reactions were documented.
3. Sentinel LN identification and surgery
Two experienced head and neck radiologists analyzed the MR lymphography images prospectively. The first LNs which show any enhancement at the peripheral portion of LNs near the injection site during the dynamic scan were regarded as sentinel LNs. We identified and enumerated enhancing nodes in each scan, and categorized their location according to the cervical nodal levels of the AJCC staging system.13,15 If more than one LN was
enhanced first at the same phase, all were considered sentinel LNs.
On the basis of the MR lymphography findings, we performed sentinel LN localization under sonographic guidance on the day before the surgery. The
7
locations of sentinel LNs were marked on the skin with an oil painting pen by the radiologist who had reviewed the MR lymphography images.
The primary tumors were surgically removed with elective neck dissection on the ipsilateral side 1–2 weeks after MR examination, and sentinel LNs under the skin marking were dissected, marked, and sent separately to the pathology department. All specimens, including sentinel LNs, were fixed in formalin, and 2-mm serial sections were subjected to histopathologic examinations for the assessment of cancer metastasis. The number and cervical LN level of the sentinel LNs identified on MR lymphography were correlated with the final histopathological findings after elective neck dissection, which were used as a standard reference.
III. RESULTS
Sentinel LNs in all 26 patients were consistently visualized by MR lymphography. In total, 44 LNs were identified as sentinel LNs on MR lymphography. In 21 of 26 patients, several lymph vessels draining from the injection site were also observed. All patients showed first-enhanced LNs, regarded as sentinel LNs, on the 1st and 2nd phases of the DISCO sequence,
except in one patient with sentinel LNs on the 3rd phase of the DISCO sequence.
During the dynamic scan after contrast injection, 16 of the 26 patients (61.5%) showed enhancement in a single assumed sentinel LN, whereas 10 patients (38.5%) showed enhancement in multiple assumed sentinel LNs. Of the 26 patients, 13 (50.0%) showed assumed sentinel LNs with level I involvement, seven (26.9%) showed level II involvement, five (19.2%) showed both level I and II involvement, and one (3.8%) showed level III involvement.
The performance algorithm and results of MR lymphography in terms of sentinel LN identification in patients with oral cavity cancer and clinically negative neck are shown in Figure 1. Primary tumor removal and LN dissection was performed in 24 of 26 patients, and neck dissection was not performed in
8
the other two patients with T1 stage oral tongue cancer and T1 stage alveolar ridge cancer because of the adoption of a “wait-and-see” approach. During surgery, all sentinel LNs identified on MR lymphography were easily resected under the guidance of skin markers. In total, 42 assumed sentinel LNs were dissected, with an average of 1.8 per patients.
Figure 1. Result of sentinel LN evaluation in patients with resectable oral cavity cancer planning elective neck dissection
The final histopathologic examinations after primary tumor removal and elective neck dissection revealed metastasis in 27 (3.9%) of the 697 dissected LNs, in 11 of the 24 patients, yielding an occult LN metastasis rate of 45.8%. Metastatic LNs were most frequently found in the ipsilateral level II (n = 14), followed by level I (n = 11) and level III (n = 2). The overall median size of all dissected LNs was 9 mm (range: 3–26 mm), while the median size of metastastic LNs was 11 mm (range: 6–26 mm), with three N1 tumors and eight
9
N2 tumors. In the remaining 13 (54.2%) patients, LN metastasis could not be detected despite thorough histopathologic evaluations of the dissected LNs.
Among the 11 patients with pathologically positive neck, 10 patients (90.9%) with metastatic sentinel LNs were accurately identified by MR lymphography; representative MR lymphography images are shown in Figures 2 and 3. The remaining one patient presented sentinel LNs in the ipsilateral level III on MR lymphography, but three metastatic LNs in the ipsilateral level I were observed without level III involvement on final histopathologic examination (Figure 4). Therefore, the rate of missed detection of sentinel LN on MR lymphography was 9.1% (one of the 11 patients).
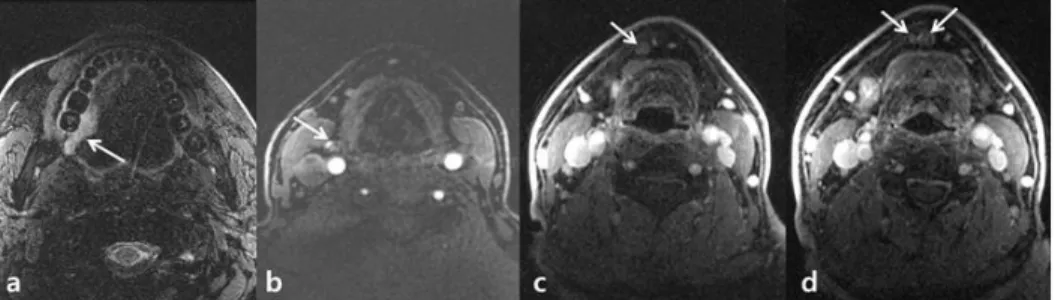
Figure 2. A 38-year-old woman with oral tongue cancer and palpably negative neck. Fat-saturated T2-weighted magnetic resonance (MR) images (a and b) show a shallow infiltrative tumor on the left lateral surface of oral tongue (arrow) and several small lymph nodes in submandibular areas. After peritumoral injection of contrast, MR lymphography (c and d) revealed two first-enhancing lymph nodes in left level IB and IIA (arrows) on the 1st phase of
10
dynamic scan, respectively. The maximum intensity projection reconstruction image of MR lymphography (e) shows the contrast injection site in the tongue (thick arrow), the assumed sentinel lymph node (thin arrow), and the lymph vessel connecting them (arrowhead). After neck dissection, metastasis of the assumed sentinel lymph nodes observed on MR lymphography could not be detected on histologic examination.
Figure 3. A 71-year-old man with buccal mucosa cancer and clinically negative neck. Fat-saturated T2-weighted MR images (a and b) show an infiltrative tumor on the right buccal mucosa (arrow) and a few small lymph nodes in the right submandibular area. MR lymphography after peritumoral contrast injection (c) revealed a first-enhancing lymph node in right level IB (arrow) on the 1st phase of the dynamic scan. After neck dissection, metastasis involvement
of the assumed sentinel lymph node observed on MR lymphography was confirmed on histologic examination.
11
the sentinel LN. Fat-saturated T2-weighted images (a) shows malignant infiltrative tumor on the right lateral surface of oral tongue. MR lymphography (b) revealed a sentinel LN in the right level III. After neck dissection, three metastatic LNs in right level IA were confirmed. There was no definite contrast enhancement in those metastatic LNs on MR lymphography (c and d).
All patients completed their examinations successfully without serious adverse events. Two patients with oral tongue cancer experienced swelling at the injection site, which resolved without intervention within 30 minutes after MR examination. No patients experienced nausea, vomiting, allergic reaction or infection of the injection site.
IV. DISCUSSION
In this study, we reported the successful use of MR lymphography with interstitial injection of gadolinium contrast agents for the preoperative identification of sentinel LNs. By adding only 5 minutes of scan time to the routinely performed preoperative MR imaging of the neck, we were able to clearly visualize the lymphatic channels from the peritumoral injection site to the cervical LNs by MR lymphography in all patients. The major strengths of the contrast-enhanced MR imaging of LNs are higher spatial resolution, higher signal-to-noise ratio, and fewer artifacts than other imaging modalities,9
although we did observe minor side effects such as mild, transient pain and swelling due to interstitial contrast injection. Therefore, by accurately identifying sentinel LNs in patients with oral cavity cancer and clinically negative neck precisely, MR lymphography might help identify patient groups at high risk of neck metastasis as candidates for focused biopsy during or even before surgery. Accordingly, MR lymphography might also help identify patients who do not require elective neck treatment, which is unnecessary in patients who do not show sentinel LN metastasis on preoperative imaging
12
studies.
Notably, all but one patient with pathologically positive neck showed metastatic sentinel LN involvement on MR lymphography. Non-opacification of sentinel LNs on MR lymphography might be caused by delayed drainage due to hindrance of lymphatic flow by intranodal tumor tissue or inhomogeneous contrast distribution due to large tumor size, This potential drawback of using interstitial contrast administration should be addressed and solved in the future.16,17
Any enhancement visible only at the LN periphery, which might be due to contrast agent uptake by the afferent lymphatics located in the cortex, was an imaging criterion for sentinel LN identification in this MR lymphography study; however, we did not analyze contrast distribution and signal characteristics. In fact, a major weakness of this technique is its inability to differentiate between benign and malignant LNs. In tumor-bearing LNs, interstitially injected contrast medium will be taken up by either the functional LN tissue or the tumor cells, resulting in poor signal contrast between the benign and malignant structures.18-22 Even on delayed images, it was impossible to differentiate
between the benign and malignant LNs by enhancement pattern in our study, because contrast enhancement was visible only at the LN periphery without filling inside the LN. The recently introduced lymphotrophic gadolinium-based T1-contrast agents such as gadopentetate dimeglumine-polyglucose associated macrocomplex (PGM) or gadoflurine M, which might accumulate in functional LN tissue after intravenous injection, can provide high contrast between malignant and functional LN tissues, and therefore, their future clinical applications need to be further investigated.23,24
This study has some limitations. First, this preliminary study included small number of patients from a single institution. A large-scale prospective study is warranted to determine if this technique will improve the clinical decision-making process. In addition, preoperative immunohistochemical
13
analysis of the sentinel LNs might provide additional information for estimation of the risk of neck metastasis. Second, we did not analyze sentinel LNs on a node-by-node basis. We could not be completely sure that the observed sentinel LNs depicted on images exactly matched the same node in the neck dissection. However, all patients were placed in same position during repeated examinations as well as surgery, and an experienced radiologist who reviewed the MR lymphography results performed sonography with skin marking. In addition, we believe that this limitation did not significantly affect the accuracy of the detection of sentinel LNs on MR lymphography because the current imaging modalities are sufficiently acceptable, providing excellent image resolution for discrimination of the location, size and morphological character on a node-by-node basis, and showing detailed anatomy of the adjacent neck area. Third, we did not include follow-up results to support the necessity of sentinel LNs selection, such as nodal recurrence after surgery and clinical outcome, which might reveal additional false-negative cases due to skip metastasis to non-dissected LNs.25
V. CONCLUSION
In conclusion, pretreatment MR lymphography using interstitial injection of gadolinium-based contrast agent is a safe and feasible imaging technique for accurate assessment of sentinel LNs in oral cavity cancer patients with clinically negative neck.
14
REFERENCES
1. Capote A, Escorial V, Munoz-Guerra MF, Rodriguez-Campo FJ, Gamallo C, Naval L. Elective neck dissection in early-stage oral squamous cell carcinoma--does it influence recurrence and survival?
Head Neck. 2007;29:3-11.
2. Salazar-Fernandez CI, Gallana-Alvarez S, Pereira S, Cambill T, Infante-Cossio P, Herce-Lopez J. Sentinel Lymph Node Biopsy in Oral and Oropharyngeal Squamous Cell Carcinoma: Statistical Validation and Impact of Micrometastasis Involvement on the Neck Dissection Decision. J Oral Maxillofac Surg. 2015;73:1403-9.
3. Matsuzuka T, Suzuki M, Saijo S, et al. Usefulness of sentinel node navigation surgery in the management of early tongue cancer. Auris
Nasus Larynx. 2014;41:475-8.
4. Chung MK, Lee GJ, Choi N, Cho JK, Jeong HS, Baek CH.
Comparative study of sentinel lymph node biopsy in clinically N0 oral tongue squamous cell carcinoma: Long-term oncologic outcomes
between validation and application phases. Oral Oncol.
2015;51:914-20.
5. Flach GB, Bloemena E, Klop WM, et al. Sentinel lymph node biopsy in clinically N0 T1-T2 staged oral cancer: the Dutch multicenter trial.
Oral Oncol. 2014;50:1020-4.
6. O'Connor R, Pezier T, Schilling C, McGurk M. The relative cost of sentinel lymph node biopsy in early oral cancer. J Craniomaxillofac
Surg. 2013;41:721-7.
7. National Comprehensive Cancer Network. Head and Neck Cancers (Version 2.2017).
8. Li C, Meng S, Yang X, Zhou D, Wang J, Hu J. Sentinel lymph node detection using magnetic resonance lymphography with conventional
15
gadolinium contrast agent in breast cancer: a preliminary clinical study.
BMC cancer. 2015;15:213.
9. Choi SH, Moon WK. Contrast-enhanced MR imaging of lymph nodes in cancer patients. Korean J Radiol. 2010;11:383-94.
10. Dimakakos E, Koureas A, Skiadas V, et al. Interstitial magnetic resonance lymphography with gadobutrol in rabbits and an initial experience in humans. Lymphology. 2006;39:164-70.
11. Nason RW, Torchia MG, Morales CM, Thliveris J. Dynamic MR lymphangiography and carbon dye for sentinel lymph node detection: a solution for sentinel lymph node biopsy in mucosal head and neck cancer. Head Neck. 2005;27:333-8.
12. Honda K, Ishiyama K, Suzuki S, et al. Sentinel lymph node biopsy using computed tomographic lymphography in patients with early tongue cancer. Acta Oto-Laryngologica. 2015;135:507-12.
13. Amin MB ES, Greene FL, et al, eds. AJCC Cancer Staging Manual, Eighth Edition. New York: Springer, 2017.
14. Loo BW, Draney MT, Sivanandan R, et al. Indirect MR
lymphangiography of the head and neck using conventional gadolinium contrast: a pilot study in humans. International Journal of Radiation
Oncology* Biology* Physics. 2006;66:462-8.
15. Som PM, Curtin HD, Mancuso AA. Imaging-based nodal classification for evaluation of neck metastatic adenopathy. AJR Am J Roentgenol. 2000;174:837-44.
16. Vassallo P, Matei C, Heston WD, McLachlan SJ, Koutcher JA, Castellino RA. Characterization of reactive versus tumor-bearing lymph nodes with interstitial magnetic resonance lymphography in an animal model. Invest Radiol. 1995;30:706-11.
17. Taupitz M, Wagner S, Hamm B. [Contrast media for magnetic resonance tomographic lymph node diagnosis (MR lymphography)].
16
Radiologe. 1996;36:134-40.
18. Misselwitz B. MR contrast agents in lymph node imaging. Eur J Radiol. 2006;58:375-82.
19. Murray AD, Staff RT, Redpath TW, et al. Dynamic contrast enhanced MRI of the axilla in women with breast cancer: comparison with pathology of excised nodes. Br J Radiol. 2002;75:220-8.
20. Luciani A, Dao TH, Lapeyre M, et al. Simultaneous bilateral breast and high-resolution axillary MRI of patients with breast cancer: preliminary results. AJR Am J Roentgenol. 2004;182:1059-67.
21. Kobayashi H, Kawamoto S, Star RA, Waldmann TA, Tagaya Y, Brechbiel MW. Micro-magnetic resonance lymphangiography in mice using a novel dendrimer-based magnetic resonance imaging contrast agent. Cancer Res. 2003;63:271-6.
22. Misselwitz B, Schmitt-Willich H, Michaelis M, Oellinger JJ. Interstitial magnetic resonance lymphography using a polymeric t1 contrast agent: initial experience with Gadomer-17. Invest Radiol. 2002;37:146-51. 23. Misselwitz B, Platzek J, Weinmann HJ. Early MR lymphography with
gadofluorine M in rabbits. Radiology. 2004;231:682-8.
24. Choi SH, Han MH, Moon WK, et al. Cervical lymph node metastases: MR imaging of gadofluorine M and monocrystalline iron oxide nanoparticle-47 in a rabbit model of head and neck cancer. Radiology. 2006;241:753-62.
25. Dias FL, Lima RA, Kligerman J, et al. Relevance of skip metastases for squamous cell carcinoma of the oral tongue and the floor of the mouth.
17 ABSTRACT(IN KOREAN) 구강암 환자에서 감시 림프절 탐지를 위한 자기공명림프관조영술에 대한 연구 <지도교수 김 진 아> 연세대학교 대학원 의학과 배 소 희 연구 배경 및 목적: 수술 전 림프절 전이가 명확하지 않은 구강암 환자에서 감시 림프절 생검은 선택적 경부 림프절 곽청술의 대안으로 사용될 수 있기 때문에, 수술 전에 영상 검사를 통해 감시 림프절을 확인하는 것은 임상적으로 중요하다. 이 연구에서는 수술 전 림프절 전이가 명확하지 않은 구강암 환자를 대상으로 가돌리늄 조영제를 주입 후 자기공명림프관조영술을 시행함으로써 수술 전 영상을 통한 감시 림프절 확인이 가능한지 알아보고자 하였다. 연구 방법: 구강암을 처음으로 진단받았으며 목에 촉지되는 림프절이 없는 환자 26명이 연구 대상으로 포함되었다. 희석시킨 가도부트롤 1mL를 구강암 원발병소 주변에 간질 주입한 뒤 자기공명림프관조영술을 시행하였다. 자기공명림프절조영술 영상에서 감시림프절을 확인하였고, 영상에서 관찰된 감시 림프절과, 환자가
18 경부 림프절 곽청술을 받고난 후의 최종 병리 결과와 비교하였다. 연구 결과: 자기공명림프관조영술을 통해 26명의 모든 환자에서 총 44개의 감시 림프절을 확인할 수 있었다. 감시 림프절은 자기공명림프관조영술 영상에서 주입된 조영제가 처음으로 림프절의 가장자리에서 관찰되는 림프절로 정의하였다. 총 24명의 환자가 경부 림프절 곽청술을 시행받았고, 이 환자들 중 11명의 환자에서 총 27개의 전이 림프절이 확인되었다. 전이 림프절이 확인된 11명 중 1명의 환자를 제외한 10명의 환자에서, 자기공명림프관조영술에서 확인되었던 감시 림프절이 모두 전이 림프절로 확인되었다. 결론: 수술 전 림프절 전이가 명확하지 않은 구강암 환자에서, 치료 전 자기공명림프관조영술은 감시림프절을 확인할 수 있는 안전하고 유용한 영상 기법이다. 추후 감시림프절 생검을 통해 잠복 림프절 전이의 가능성이 높은 환자를 판별하는데 도움을 줄 수 있는 영상 기법이다. --- 핵심되는 말 : 자기공명림프관조영술, 구강암, 감시림프절, 림프절 전이